Health Behavior Change
Online Continuing Education Course

Course Description
Enhance your professional clinician skills with the Health Behavior Change continuing education course. Learn to explain the concept of change, apply practical strategies for promoting healthier behaviors, and understand key models, such as the transtheoretical model. Gain insights into outcome-driven change, communication techniques, and factors influencing a patient's ability to change -- empowering you to become an effective change agent in healthcare. Applicable CEUs for nursing and occupational therapy nationwide and physical therapy in select states.
Course Price: $18.00
Contact Hours: 2
Course updated on
November 4, 2025
"Excellent course. Case studies were very beneficial. Kudos to the author!" - Monica, RN in California
"Interesting. I will apply the content when teaching patients lifestyle changes for better health." - Rita, RN in Kansas
"Great review and relevant content with good case examples. Enjoyed this CEU!" - Jennifer, RN in Nevada
"Excellent for all facets of life, and for all who want to help elicit change in self and others." - Kerri, RN in California
Health Behavior Change
Copyright © 2025 Wild Iris Medical Education, Inc. All Rights Reserved.
LEARNING OUTCOME AND OBJECTIVES: Upon completion of this continuing education course, you will be able to explain the concept of change and practical strategies for helping people change their health-related behaviors. Specific learning objectives to address potential knowledge gaps include:
- Explain the concept of a change agent.
- Discuss outcome-driven change.
- Describe the stages of the transtheoretical (stages of change) model.
- Explain various other models of change.
- Identify factors affecting an individual’s ability to change.
- Describe communication techniques that healthcare professionals use to facilitate behavioral change.
TABLE OF CONTENTS
INTRODUCTION
Changing a behavior and forming new habits are hard to accomplish, and healthcare professionals are often frustrated when patients do not follow medical advice or treatment recommendations. It may be difficult to understand the reluctance or unwillingness of a patient to make important changes that have been shown to improve health and well-being, especially after healthcare professionals have repeatedly stressed the importance of doing so. In the United States, for example:
- Only about 50% of patients who leave a healthcare setting with a prescription for medication take the medication as directed. The most common reasons given for not adhering to medication regimens are denial of illness, lack of understanding about the benefits of taking the medication, and cost.
- Nonadherence is believed to result in 125,000 deaths due to cardiovascular disorders each year.
- If patients adhered to their drug regimens, up to 23% of nursing home admissions, 10% of hospital admissions, many physician visits, many diagnostic tests, and many unnecessary treatments could be avoided.
- Although half of surveyed adults who smoke disclosed they are trying to quit, only 1 in 10 adults who attempt to quit are actually successful in a given year. It is not easy to stop smoking due to withdrawal symptoms (e.g., irritability, trouble concentrating) and daily activities associated with smoking (e.g., drinking coffee in the morning, during social situations where others are smoking).
(Lynch, 2025; CDC, 2024a)
THE CLINICIAN AS CHANGE AGENT
Recognizing both the difficulties and resistance to change, researchers continue to examine the nature of change and how healthcare professionals can motivate, educate, and support individuals throughout the process of change. All clinicians serve as change agents, whether they realize it or not. A change agent is a person or group that facilitates the change process (Grandison, 2022).
Change is essential for patients (and their loved ones) to achieve maximum wellness. Most, if not all, patients need to make some types of behavioral change. But providing adequate education and finding the time to teach makes working as an effective change agent challenging for clinicians.
Grandison (2022) suggests five ways to be an effective agent, which are adapted below for the healthcare setting.
Embrace Resistance
People are often resistant to change, and healthcare professionals must become comfortable when dealing with such resistance. Patients who must change diets, take new medications, or deal with a newly diagnosed chronic illness are likely to deny that a change is necessary. This can be an instinctive reaction to bad news. If healthcare professionals anticipate resistance, they will not be taken off guard when it occurs. It is important to identify common sources of resistance and plan for a variety of ways to address them. (See also “Factors Affecting Change” later in this course.)
Co-Create the Vision
Healthcare professionals, patients, and families should work together to create a vision of patient behavioral change. Frequent and consistent communication among these groups is absolutely necessary. Since time to facilitate change can be limited, it is helpful to develop a consistent manner of providing patient education, including establishing objectives, no matter the setting. While it is true that most healthcare facilities have written education materials to distribute, such materials are often not sufficient. It is imperative that actual learning be evaluated.
Get Buy-In
Patients and families will not change their behavior unless they want to change and have the means to do so. Getting “buy-in” has its foundation in realism and practicality. If patients see the change goal as achievable, they are more likely to buy in. Therefore, part of the education to achieve behavioral change must include a complete assessment, including issues such as finances, ability to plan meals, available transportation options, and so forth, to make sure the plan is achievable. These types of assessment questions should be included on any and all education assessment forms. Information gathered is then used to implement change.
For example, a patient at risk for obesity-related conditions may not feel the need to lose weight. The patient may say they “feel fine” and that they enjoy eating, especially at family get-togethers. They may also believe that any significant weight loss is impossible given their family’s eating habits. In cases such as these, it is imperative that families become invested in helping the patient “buy in” to achieve weight-loss goals. Healthcare professionals can meet with both patient and family members to discuss what factors might motivate them all to work on behavioral change. For instance, changes in what is served at family gatherings may allow for calorie reduction while maintaining social contact. Or incorporating exercise into family activities (such as walking together after meals) might seem more inviting if it allows the patient to spend more time with grandchildren.
Other patients may already want to change health-related behaviors to live longer or to feel better but may be unable to acquire what is necessary (e.g., the funds to purchase prescribed medications) to make necessary changes. It is imperative that healthcare professionals have knowledge of various resources designed to help offset healthcare expenses and that they share such knowledge with patients and families.
Create a Track Record
The vision of change must be implemented in a practical way. Consistency is important and helps to make the education process more time efficient. A written tool for assessment (with space for individualization) and the education plan should be documented in the medical record. This helps the entire healthcare team track what progress (or lack of progress) has been made. Ways of facilitating patient compliance, change, and patient/family education should be part of all staff meetings. Consistent discussion and established ways of implementing education in healthcare help to create a track record of success or lack of success and can improve outcomes.
Make Change Normal
It is important to help patients and families view change as normal, although this is easier said than done. Few people “love” change. Whether a change in one’s healthcare routine is temporary (for acute issues) or long-term (for chronic issues), helping change to become a regular part of a patient’s health maintenance will go far in facilitating compliance.
It is important to approach present behavioral health change as a normal process and to avoid making it overly complicated. Goals must be realistic and achievable. For example, a patient who is dealing with severe hypertension and has consumed a diet high in sodium throughout their life is not likely to immediately reduce their salt intake significantly. Expecting an immediate, total reduction in salt intake is unrealistic for patients such as this. Instead, the clinician can break the target goal of reduced sodium intake into incremental decreases.
CASE
Being a Change Agent
Juan is a 65-year-old construction engineer. He is looking forward to retiring within the next few months and spending more time with his wife and grandchildren and on his many hobbies. What Juan is not looking forward to is making some changes in his lifestyle per his physician’s recommendations.
Juan has dangerously high blood pressure. He is fond of high-sodium foods and is about 10 pounds overweight. His physician has prescribed an antihypertensive medication to be taken daily, a low-sodium diet, and consultation with a dietitian to help revise his diet in order to lose weight. Juan is also being encouraged to increase the amount of exercise he engages in.
Juan is fiercely independent and does not see the need to change his health-related behaviors. “I feel fine! I have almost as much energy as my grandchildren!” His wife concurs. She doesn’t understand the need for change when Juan looks and feels well.
Discussion
Juan is a person who falls into the category of “I don’t want to change; I don’t see the need for change.” How might healthcare professionals act as change agents to help Juan adopt more healthy behaviors?
First, accept that Juan is an intelligent adult who is accustomed to doing things his own way. He should be treated with respect and included in every step of the treatment planning process. Embracing his resistance allows the healthcare professional to acknowledge that Juan has his own goals and objectives. Simply telling Juan he must adhere to a new diet, exercise, and take medication, on the other hand, may be overwhelming. Unless Juan and his family “buy in” to the need for change, change will not take place.
How can healthcare professionals facilitate buy-in? Juan and his wife should discuss options with his healthcare providers. For example, since he enjoys being with his grandchildren, are there ways to add more exercise to his daily routine that include the grandchildren, such as going for a walk, playing a game of baseball, and so forth? This is exercise in a form that Juan might find pleasant.
Clinicians, Juan, his wife, and his family must be co-creators of the vision for change. Unless all parties involved agree on what is necessary, success is not possible. Manageable goals should be developed together. For instance, Juan may need to ease into dietary changes. He and his healthcare team might start with eliminating added salt in his diet, then progress to limiting or avoiding certain foods and so forth.
Juan and his wife not only need to know why changes will improve Juan’s health but also to see any proposed changes as part of a “normal” ongoing process. Can Juan and his wife add more walking simply by parking in a distant parking space when out on their normal routine, shopping, going to the movies, and so forth? Dietary changes can also become normalized by substituting a few ingredients in Juan’s favorite recipes. These changes can then be seen as the new normal.
Developing and documenting a plan of care for Juan’s improved health is imperative. Specific goals and objectives should be made clear, avoiding the confusion that might occur due to the many different viewpoints and actions. Success in achieving these goals and objectives can then be tracked at subsequent visits with all members of the healthcare team.
OUTCOME-DRIVEN CHANGE
All planned change has an end goal: a specific, long-term outcome the planner hopes to achieve. An outcome-driven approach concentrates on specific, measurable objectives to determine the impact a treatment or intervention has on the health of a patient or groups of patients (Badillo-Diaz, 2025).
For example, suppose a patient is working on losing a total of 50 pounds, which can sound overwhelming. An outcome-driven approach might employ agreeing with the patient on a measurable outcome, such as “lose 1 to 2 pounds a week for a total of 4 to 8 pounds before the next office visit in one month.”
Outcome Measures
The top seven healthcare outcome measures are linked to behavioral change. If patients do not adopt healthy behaviors, any one of the following outcomes can be compromised. These seven outcome measures are:
- Mortality. Failure to comply with treatment regimens can lead to an increase in mortality rates.
- Safety of care. Safety, in the instances of desired health-related behavioral changes, can be linked to education. Although healthcare professionals cannot “make” patients adopt important behavioral changes, they are responsible for making sure appropriate information is relayed and for objectively evaluating patient/family knowledge.
- Readmissions. Readmission because of noncompliance with treatment regimens is a significant problem.
- Patient experience. Patient-reported outcome measures (PROMs) are not only an important indicator of satisfaction with services but can provide information about how well patients were taught about their treatment regimens.
- Effectiveness of care. Effectiveness of care includes compliance with best-practice guidelines and actual achieved patient outcomes.
- Timeliness of care. Timeliness-of-care outcomes evaluate patient access to care. This includes not only how quickly adequate care is provided but also how effective patient education has been. In other words, did patients (and families) receive the necessary education to make appropriate behavioral changes in a timely manner?
- Efficient use of medical imaging. Although not directly related to behavioral change, efficient use of medical imaging indicates adherence to best-practice standards.
(Tinker, 2025)
Three essentials for successfully measuring healthcare outcomes are:
- Data transparency. Publicly reported healthcare outcomes help to show that patients are receiving the best care in the most cost-effective way.
- Integrated care and transitions of care. Patient transitions throughout the healthcare system should be coordinated. All members of the healthcare team are responsible for managing quality care and providing safe and appropriate care at all transitional points of care.
- Data interoperability. Sharing data between departments is essential. Achieving outcomes and system improvement depends on ability to share data across clinicians, labs, hospitals, clinics, staff, and so forth. Data interoperability provides a single source of truth.
(Tinker, 2025)
CASE
An Outcome-Driven Approach
Jim just learned he has type 2 diabetes. He knows nothing about diabetes and until now has paid little attention to his diet or health. Jim’s healthcare provider gives Jim several pamphlets about diabetes, refers him to a diabetes website, and suggests he attend classes offered by the local hospital. Though Jim reads the brochures and information he finds on the website, he does not understand how to apply it to his condition, nor does he grasp the importance of monitoring blood glucose levels. He is afraid of blood and needlesticks and therefore inconsistent in monitoring his blood glucose. He is also uncertain about what to do if readings are abnormal.
When Jim attends a diabetes education class at the hospital, he realizes he needs much more information as it applies to his own personal situation. He shares his fears and confusion, and he asks the diabetes educator leading the class for help. The educator agrees and consults with Jim’s physician. During a follow-up appointment, the diabetes educator identifies Jim’s barriers and specific, measurable objectives to help Jim meet his diabetes learning needs (outcome-driven approach).
One of the objectives they agree upon is “Jim will accurately perform a blood glucose test 100% of the time.” The educator explains the reason for the test and its relevance to Jim’s disorder. She encourages him to talk about his concerns and feelings about blood glucose monitoring. Then, she demonstrates how to accurately monitor blood glucose levels, what normal target ranges are, and what to do if levels are abnormal. Jim mirrors her demonstration until he can do it accurately. He also participates in role-playing examples of what to do for various abnormalities if and when they occur.
Discussion
The diabetes educator, acting as a change agent, linked the rationale for performing a blood glucose test to Jim’s disease and diet, further motivating Jim to change his behaviors. In doing so, the educator helped Jim to develop an outcome-driven approach that:
- Clearly states each specific, measurable objective (i.e., Jim will accurately perform a blood glucose test 100% of the time)
- Identifies barriers to changing behavior (i.e., Jim admits that he is afraid of blood and the pain associated with a needlestick)
- Looks for specific items and behaviors to facilitate change in the patient (i.e., the educator shows Jim how to use the blood drawing equipment to reduce the amount of blood drawn and the degree of pain felt with repeat tests)
- Arranges follow-up to help the patient maintain newly acquired healthy behaviors (i.e., the educator schedules regular clinic visits for Jim and enrolls Jim in a diabetes self-management program)
THEORIES AND MODELS OF CHANGE
In order to help patients make change and to maximize the success of interventions, it is important that healthcare professionals have a theoretical understanding of change. Such theory comes from the accumulated knowledge about what mediates and moderates change behavior. The table below describes four major theories and models of behavior change.
| Theory/model | Description |
|---|---|
| Transtheoretical model (TTM) (also referred to as stages of change) | Change is a process involving progress through a series of stages. |
| Theory of planned behavior (TBP) | Change in behavior is determined by intention to perform the behavior. |
| Health belief model (HBM) | Behaviors are based on attitudes and beliefs. |
| Social cognitive theory (SCT) | Change is driven through interaction between environment, personal factors, and attitudes. |
Transtheoretical Model (TTM)
Of the four major theories and models, the most widely applied and tested is the transtheoretical model (TTM), also referred to as stages of change. TTM can be applied across a wide variety of clinical education topics, including smoking cessation, alcohol use, sunscreen use, sexually transmitted infection (STI) prevention, and preventative healthcare measures such as cancer screening. TTM identifies sequential stages that people move through as they change from old behaviors to new ones:
- Precontemplation
- Contemplation
- Preparation
- Action
- Maintenance
- Termination
(UMBC, n.d.; Raihan & Cogburn, 2023)
PRECONTEMPLATION
Precontemplation is the stage when there is no conscious intent to make a change. In this stage, people are not even thinking about changing their behaviors. They may not see current behaviors as problematic or may think that the problem is being exaggerated.
CONTEMPLATION
Contemplation is the stage when individuals are aware that the behavior is a problem and intend to change behavior relatively soon, but they may vacillate for a long period of time. Often, people in the contemplation stage are not yet truly ready to change. They may procrastinate or doubt their ability to change. Individuals in this stage are often highly ambivalent, may be interested in learning about how to make change, but still cannot make a decision.
PREPARATION
Preparation is the stage in which individuals know they must change and become committed to take action to change. The pros of change outweigh the cons. Often something happens to motivate a person to take action, such as an emotion-laden crisis, recent illness, or plea from an important person in their life. During this stage, not all ambivalence has been resolved, but it is no longer an impossible barrier to overcome. The person may develop a plan of action but not yet be completely committed to actually changing the behavior (UMBC, n.d.).
ACTION
This is the stage where people believe they have the ability to change behavior and are actively involved in taking steps to do so. This is the beginning of actual change, when goals and objectives are identified. It is also the stage when relapse and subsequent regression to an earlier stage is most likely (UMBC, n.d.). Clinicians should be aware of this potential and help patients/families to be especially vigilant. The patient needs support from family and friends as well as from the healthcare team. Members of the team should check in more often with patients and listen to concerns and issues affecting change.
This is the stage when patients develop new habits and work toward what some have called “SMART objectives” (see table below).
| Objective | Example |
|---|---|
| (CDC, 2024b) | |
| Specific | Answers the question, “What is to be done?” (e.g., deciding, “I will no longer smoke cigarettes or any other substance.”) |
| Measurable | Answers the question, “How will I know I’ve met expectations?” (e.g., determining that “I will not keep any cigarettes, even an ‘emergency smoke,’ in my environment.”) |
| Achievable | Answers the question, “Can I do this?” (e.g., reassuring oneself by thinking, “I have overcome other cravings. Other people have stopped smoking, and I can too.”) |
| Relevant | Answers the question, “Should it be done and why?” (e.g., realizing that “Smoking is not necessary for me to enjoy life; in fact, it may kill me.”) |
| Time-bound | Answers the question, “When will this be accomplished?” (e.g., setting the goal, “I will stop smoking by January 1, the beginning of a new year.”) |
MAINTENANCE
Patients are thought to be in maintenance when they have attained and maintained desired behavioral change for at least six months. Although the risk for relapse still exists, it is less, and patients need to exert less effort to maintain the change (UMBC, n.d.).
TERMINATION
Termination is the point at which temptation to relapse is no longer a threat. This stage is the most difficult to achieve. The person now has complete confidence that change has been accomplished and no longer fears relapse. Examples of accomplishing this stage includes buckling a seat belt upon sitting down in a car or taking a medication at the same time each day (UMBC, n.d.; Raihan & Cogburn, 2023).
CASE
Stages of Change
Anna has smoked cigarettes for more than 35 years. She has heard that smoking is bad for one’s health, but she says, “I’ve smoked this long and it hasn’t killed me yet.” Recently, family members have begun insisting to her that she really must quit this time, but this angers her, and she tells them to stop harassing her about it. (Precontemplation)
Over the next few months, Anna develops a cough, especially at night, excessive sputum, and some shortness of breath. She also begins feeling more fatigued. She is hoping maybe she just has a cold, but she also suspects it might be related to her smoking and wonders whether her family is right about the need to quit. Finally, after a few more weeks of procrastinating, she makes an appointment to see her healthcare provider.
At her appointment, the physician examines Anna and eventually diagnoses her with chronic obstructive pulmonary disease (COPD). Faced with this new diagnosis, Anna is strongly urged to quit smoking. She is given information about the disease process and pamphlets that offer suggestions for stopping smoking. She takes them home, reads them, and thinks a lot about quitting. But other days, after enjoying her cigarette and morning cup of coffee, she can’t imagine giving it up. Then she remembers, “I’m not really enjoying this coughing and shortness of breath.” (Contemplation)
One very cold day, on the walk from her mailbox back up her long driveway, Anna becomes shorter and shorter of breath. Her chest feels tight, she begins to wheeze, and she can’t stop coughing. She barely makes it back into the house, lays down, and waits fearfully until she can breathe again. At that point, she decides it’s time to quit smoking. She calls her doctor’s office and says she wants to sign up for the smoking cessation classes mentioned in the pamphlets. (Preparation)
Anna is now ready to quit. At her first smoking cessation class at the local hospital, the educator helps her identify times when she usually smokes, plan other activities at those times, and arrange with friends for support when she needs it. The educator teaches Anna the “SMART” objectives. Anna decides to work on achieving realistic goals. First, she targets January 1 as the date to decrease her smoking from one pack to five cigarettes per day. Once January 1 rolls past and Anna reduces her smoking, she begins to struggle and cannot stick with her goal each day. At their next appointment, Anna and the educator acknowledge that relapse is not uncommon at this stage. Anna will need support, not condemnation, and together they reevaluate her goals for achievability. (Action)
With encouragement, Anna is able to meet her goal over the next couple of months, but she’s still finding it challenging and realizes she needs additional help to stick with it. She joins a community support group of other long-time smokers, all of whom are determined to stop smoking. Over the next few months, the other members encourage Anna and give her tips to prevent relapse. (Maintenance)
One year later, Anna no longer smokes and no longer wants to. In fact, she is turned off by the smell of secondhand smoke. Her COPD has not progressed, and she intends to keep it that way. (Termination)
Other Theories and Models of Change
Although the TTM is the most widely applied and tested model, there are other theories and models of change in use. Some of the more common ones are briefly explained below.
THEORY OF PLANNED BEHAVIOR (TPB)
The theory of planned behavior has been successfully used to predict and explain a wide variety of health behaviors such as smoking, drinking, utilization of health services, breastfeeding, and substance use. According to TPB, intentions are determined by three variables:
- Personal attitudes. Refers to the person’s positive and negative view of the behavior that needs to be changed. For example, a person with substance use disorder may think that drinking alcohol in excess makes them feel happy, but they also know it gives them a hangover in the morning and is expensive.
- Subjective norms. Refers to the belief about whether most people approve or disapprove of the behavior and relates to how family, peers, and other people important to the patient feel about the need for the behavioral change. For example, a person with substance use disorder knows that their family and friends believe they drink excessively and act inappropriately toward them when inebriated.
- Perceived behavioral control. Refers to the person’s perceptions of how easy or how hard changing behavior is going to be. For example, a person with substance use disorder may feel it will be very difficult to quit using because they have become addicted.
Based on these variables, people then develop intentions that lead to behaviors (Brookes, 2023).
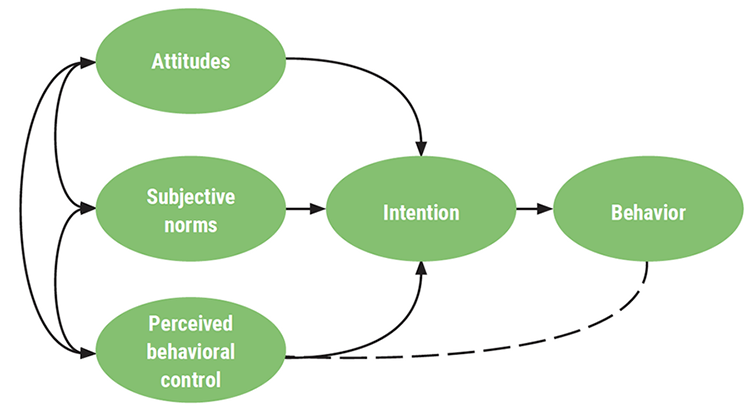
Theory of planned behavior. (Source: U3236610 Allana, CC BY-SA 4.0.)
HEALTH BELIEF MODEL (HBM)
The health belief model was developed to understand the failure of people to adopt disease prevention strategies or undergo screening tests for the early detection of disease. Its foundation comes from psychological and behavioral theory that proposes two components of health-related behavior: (a) the desire to avoid illness or to get well if already sick and (b) the belief that a specific health behavior will prevent or cure illness. A patient’s course of action depends on their perceptions of the benefits and barriers related to health behavior (Alyafei & Easton-Carr, 2024).
SOCIAL COGNITIVE THEORY (SCT)
The foundation of social cognitive theory is an emphasis on social influence and external and internal social reinforcement. SCT examines the unique ways in which individuals acquire and maintain behavior, taking into account the patient’s social environment and past experiences. Past experiences are believed to influence expectations, which shape whether a person will engage in a specific behavior and the reasons why a person engages in that behavior (Nickerson, 2025).
CHOOSING A MODEL OF CHANGE
In choosing a model of change, it is important to decide what one is appropriate to the patient’s desired outcomes and circumstances. For example, the health belief model does not account for environmental and social–cultural factors, whereas social cognitive theory (SCT) relies on interactions between people and their environments. Thus, if a patient’s lack of physical activity is heavily influenced by peers, work, or family, SCT might be the better approach (Luque, n.d.).
FACTORS AFFECTING CHANGE
There are three primary factors that affect change—motivation, knowledge/skills, and support—along with many potential barriers.
Motivation
Motivation is the willingness to do something or that which causes this willingness. Motivation is also described as enthusiasm for doing something (Cambridge Dictionary, 2025). Without motivation, health-related behaviors are unlikely to change. Therefore, it is important for healthcare professionals to help motivate their patients.
The following strategies have been found to be helpful when motivating patients:
- Implement shared decision-making. This enables patients to be active participants in the development of their plan of care and to make informed choices that are respected by the healthcare team. The healthcare professional should not assume ownership of the patient’s health. Patients must assume ownership of their own health status.
- Use motivational interviewing. Motivational interviewing is a conversation between patients and healthcare professionals to facilitate a patient’s motivation and commitment to change. Techniques such as using open-ended questions, affirmations, reflective listening, and summarization are important parts of the motivational interviewing. (See also “Motivational Interviewing in the Healthcare Setting” later in this course.)
- Use the 5 As behavior change framework, or ask, assess, advise, agree (collaboratively), and assist or arrange follow-up care. The 5 As is an evidence-based tool to motivate change in patients, such as losing weight, quitting smoking, eating healthy, and lowering alcohol consumption. For example, asking a patient if it is okay to discuss their weight may help open the door for communication. If so, then an assessment can be conducted and the patient can be advised via education and discussion of treatment options. Finally, patient and clinician can agree on a plan, and the clinician can assist the patient with resources, appropriate referrals, and proper follow up.
(Hartney, 2023; Harward, 2022)
EXERTING AND DEPLETING WILLPOWER
Willpower is related to motivation. It is also referred to as determination, drive, resolve, self-discipline, and self-control. The American Psychological Association defines willpower as:
- The ability to delay gratification, resisting short-term temptations in the interest of achieving long-term goals
- The ability to override unwanted thoughts, feelings, or impulses
- The implementation of conscious, effortful, regulation of the self
Willpower can be depleted. Research shows that frequently employing willpower to resist temptations (such as smoking or eating a high-calorie diet) takes a mental toll on patients and may affect brain function. Exertion of willpower may also lower glucose levels (APA, 2012).
Research also indicates that willpower depletion can be kept in balance by personal beliefs, attitudes, and behaviors. For example, patients who felt forced to exert willpower were more easily depleted compared to patients who exerted willpower based on internal goals and desires.
Certain strategies have been shown to build up self-control. Patients can be encouraged to:
- Focus on one goal at a time. Research shows that it is more effective to focus on one goal at a time rather than working on achieving multiple goals at once.
- Avoid temptations. In other words, do one’s best to limit distractions.
- Make a plan. Having a realistic plan helps to maintain equilibrium. Decide beforehand how to react to circumstances that can interfere with one’s goals.
- Monitor behavior, with focus on the end goal. Develop an objective, realistic plan to meet goals and monitor one’s progress on goal achievement.
- Reward oneself. When milestones are reached, reward oneself for achieving them.
- Get adequate sleep and rest. Sleep deprivation affects energy, focus, and determination.
- Seek support. Develop adequate support systems of trusted people who can provide support as one works on their goals.
(APA, 2012; APA, 2023)
Knowledge and Skills
Another major factor in helping patients commit to a plan with proven results is the acquisition of the right knowledge and problem-solving skills. The healthcare professional is often the source for such knowledge, offering appropriate resources, including formal training, to enhance skills needed to accomplish and maintain behavioral change. Healthcare professionals must acquire knowledge of the complex and dynamic interactions among individual patients, their environments, and the activities that are part of their daily lives (Haracz, 2025).
Support
A support system is defined as having a network of people that can provide practical or emotional support. Multiple studies have shown that social support is a significant influence on a person’s ability to make a successful behavior change. Individuals who receive support for change can strengthen willpower and stay on track toward meeting their goals (Hood, 2025).
With the proper support system, patients can learn how to make long-term changes in lifestyle and behavior. For example, if a patient is adopting a new diet because of a recently diagnosed health problem, loved ones can offer appropriate foods and avoid preparing meals that are blatantly contraindicated.
As change agents, healthcare professionals realize that even when their patients are well along on the path toward their objective, they must also provide support to help to prevent relapse. Though patients are confident they can continue their identified change, they are still vulnerable. For this reason, caregivers must arrange and encourage follow-up measures to help people maintain the changes they have worked so hard to achieve, such as ongoing visits, membership in support groups, participation in managed care that emphasizes wellness, and mentoring.
Barriers to Change
The American Medical Association (AMA, 2023) has published “8 Reasons Patients Don’t Take Their Medications.” These reasons can also be applied to most noncompliance issues:
- Fear. Fear of potential side effects can deter patients from taking their medications as prescribed. Some patients may have experienced side effects with other treatments, witnessed side effects experienced by family or friends, or heard about potential side effects from other patients. Patients need objective, factual information about both risks and benefits in order to influence them to take their medications as prescribed.
- Cost. Cost of treatments (e.g., medications, equipment) is often a major barrier to compliance. It is important that healthcare providers consider the cost of treatments and search for alternatives as necessary.
- Misunderstanding. Patients may not know how to comply with treatment plans. How to use equipment, how to perform procedures, or when to take mediations may be confusing to patients and families. Therefore, patient/family education is critical. Patients should, for example, demonstrate how to use equipment or describe how to recognize medication side effects. Learning must be objectively measured.
- Too many medications/treatments. Multiple treatments or medications can make for a complex schedule. Patients’ schedules should be as streamlined as possible.
- Lack of symptoms. Patients may stop treatment (e.g., taking medications) when they start to feel better. They might assume that their problem is resolved and that there is no need to continue treatment. Or they might think that the treatment is not helping. Patients must be taught the importance of adhering to treatment.
- Mistrust. Patients may not trust the healthcare system. Media coverage of negative aspects of healthcare and negative personal experiences or experiences of family and friends can contribute to a sense of mistrust. Ongoing negativity can cause patients to be suspicious of their own healthcare providers in particular and the healthcare system in general.
- Worry. Patients may worry about the effectiveness of treatments, their costs, and fears of becoming dependent on medications. Healthcare providers must communicate objectively and patiently and evaluate patients’ understanding of their treatment regimens.
- Depression. Patients who experience depression are not as likely to adhere to their treatment regimens as patients without depression. Patients must be screened for depression, assessed for the need for intervention, and evaluated to determine the success of any intervention initiated to treat the depression.
CASE
Factors Affecting Change
Mark is a 19-year-old college student and former elite-level athlete. He was injured in a car accident a few months ago and sustained a serious leg injury that resulted in amputation of his left lower leg. He is receiving both occupational and physical therapy services on an outpatient basis.
Mark is angry and showing signs of depression. He hates wearing his prosthesis but does not want to use crutches. He feels that he is different from all of his former teammates and that they regard him as someone to be pitied. He is finding it difficult to accept the fact that resuming his role on the college team will not be possible for him. Mark also distrusts members of the healthcare team, believing that they are all “too old” to remember what it was like to be young and healthy and, as he says, “disfigured.”
Mark is noncompliant with his prescribed at-home exercises and balance techniques. He falls frequently at home and in his college dormitory.
Discussion
Mark is coping with a great deal in life, not just his injury. At this developmental stage of late adolescence, he doesn’t want to be different from his friends. He also sees himself as disfigured and no longer able to dream of a future in sports.
To help decrease the barriers interfering with Mark’s therapy, the clinicians address the factors that may be affecting him. They:
- Suggest that Mark visit his college’s office of disability services and inquire about support groups, where he will meet others who have experienced the loss of a limb and are close to him in age. Having the opportunity to talk to someone he can relate to can be very helpful. (Support)
- Determine priorities from Mark’s point of view. He doesn’t want to be “different.” Implementing his exercise regimen can help to reduce falls and facilitate prosthesis use. (Motivation)
- Find out what about his prosthesis is so difficult for Mark. Does it cause pain? Does he feel that it doesn’t fit properly? (Knowledge and skills)
- Emphasize what adhering to treatment regimens can do to return Mark to a more “normal” life. (Motivation)
- Recommend a mental health consultation. Mark is showing signs of depression, and mental health interventions are important to help Mark maintain/achieve mental health, which should facilitate compliance. (Support)
COMMUNICATION TECHNIQUES FOR FACILITATING CHANGE
To bring about behavioral change, healthcare professionals use a variety of communication techniques to support patients in making significant, health-promoting changes in their lives. Some specific techniques used for this purpose are described below.
Motivational Interviewing in the Healthcare Setting
All of the following supportive techniques help to bring about behavioral change and comprise what is called motivational interviewing (MI). Those who practice motivational interviewing:
- Show nonjudgmental empathy. Nonjudgmental empathy is the ability to encourage patients to fully express themselves, allowing patients to dominate the discussion. The empathic listener is attentive to what is being said, does not judge, does not interrupt, is sensitive to the emotion being expressed, and attempts to see the world through the patient’s eyes.
- Listen attentively and reflectively to patients to draw out rather than impose ideas. Attentive listening involves the use of positive body language such as facing the person and making frequent eye contact to be “seen” as actively listening. (It is also important to be sensitive to cultural differences in communication; for instance, in some cultures, direct eye contact may be offensive.) Reflective listening involves expressing back to the patient what has been heard using either the patient’s own words or rephrasing them.
- Develop and examine the discrepancy between the individual’s goals and current behavior. This involves helping the person focus on how current behavior differs from desired behavior by describing what the person’s values are and how current behavior is in conflict with those values.
- “Roll” with resistance by recognizing, acknowledging, and exploring the patient’s resistance rather than opposing it. Resistance is evident by such behaviors as rejecting an idea, disagreeing, excusing, minimizing, inattention, ignoring, or being defensive. The clinician avoids arguing for change and addresses the underlying concerns and fear of change.
- Support self-efficacy. Self-efficacy is the patient’s belief that change is possible and that they have the ability to make change. The clinician focuses on eliciting and supporting optimism by recognizing past successes and highlighting skills and strengths.
(Hartney, 2023; Ingersoll, 2024)
EMPATHETIC COMMUNICATION
Empathetic communication is an important part of motivational interviewing. Some skills to facilitate communication include:
- Practicing reflective listening. Listen intently, and focus on the other person’s words and body language.
- Identifying patients’ various communication styles. Adapt to communication in ways that patients feel most comfortable with.
- Evaluating personal communication skills, their strengths, and their weaknesses.
- Managing one’s own emotions. Be aware of one’s own emotions as well as the patient’s emotions. During difficult conversations it is important that patients have a chance to process what is being said.
- Admitting mistakes. When communication mistakes are made, acknowledge them and work to improve how patient interactions occur.
(Hartney, 2023; Ingersoll, 2024)
Motivational interviewing is a particular type of conversation about change in which the patient rather than the healthcare professional brings forth the arguments for change. MI is also a collaborative process, a partnership that respects the patient’s autonomy, empowers, and gives responsibility for change to the patient. It requires the provider to recognize each patient’s worth and potential.
Using empathy, the healthcare professional strives to understand the patient’s perspective while affirming strengths and efforts. Through collaboration, the patient and provider negotiate a plan to help make change happen. Developing a partnership for change involves the willingness of the healthcare professional to suspend the reflex to give expert advice and to ask questions that allow for the exploration of the patient’s motivations.
The basic communication style of motivational interviewing, sometimes referred to by the mnemonic OARS, involves:
- Open questions
- Affirmations
- Reflective listening
- Summary
(Hartney, 2023)
ASKING OPEN QUESTIONS
Open questions invite the patient to elaborate and cannot be answered with a yes or no:
- Open question: “What makes change hard for you?” (“I’m not sure, but …”)
- Closed question: “Change is hard for you, isn’t it?” (“Yes, it is.”)
- Open question: “Tell me how drinking fits into your life.” (“I like to relax after work with a few drinks and …”)
- Closed question: “Do you think you drink too much?” (“No, not really.”)
(Hartney, 2023; Ingersoll, 2024)
USING AFFIRMATIONS
Affirmations are statements that recognize the patient’s strengths. They assist in building rapport and help the patient see themself more positively:
- “You are really taking this seriously.”
- “You’ve been successful in changing your smoking behaviors in the past.”
- “You showed a lot of courage in dealing with that problem.”
(Hartney, 2023)
REFLECTIVE LISTENING
Reflective listening is a crucial skill in which the listener paraphrases and restates both the feelings and the words of the speaker. It does not involve asking questions. Techniques of reflective listening include mirroring and paraphrasing.
Mirroring is repeating back key words or the last few words spoken while using the person’s tone of voice, pace of speaking, and body language:
- Patient (sarcastically): “I really am angry with everyone telling me to eat right and get more exercise!”
- Clinician: “You really seem angry to me!”
Paraphrasing is putting the patient’s message into your own words in an abbreviated form:
- Patient: “I wish I could wake up in the morning and feel ready to face the day.”
- Clinician: “You want to feel motivated to get up and do things.”
(Hartney, 2023; Ingersoll, 2024)
SUMMARIZING
Summarizing is a type of reflection in which the clinician recaps what has occurred in all or part of the interaction. Summaries communicate interest and understanding. They can also be used to shift attention and prepare the patient to move on.
- Clinician: “It sounds like you’re concerned about how much alcohol you are drinking because it has caused difficulties at home, and your wife wants you to stop. But you also said how important it is to have a few drinks when you get home from work so you can relax. That sounds like a difficult choice.”
(Hartney, 2023; Ingersoll, 2024)
ROADBLOCKS TO COMMUNICATION
People often have the tendency to jump in and “help” others by offering advice or reassurance to make them feel better. These responses may have the opposite effect and become “roadblocks” that fail to support good communication. Roadblocks tend to interfere with the person’s ability to explore and express their own perception of the problem. They may include:
| Roadblock | Example |
|---|---|
| Commanding, directing, ordering | “You have to …” |
| Threatening, warning | “If you don’t, then …” |
| Providing solutions, making suggestions, or giving advice | “Let me suggest …” |
| Using logic, lecturing, or arguing in order to persuade | “The facts are …” |
| Preaching, moralizing, using “should dos” | “You ought to …” |
| Judging, disagreeing, blaming, or criticizing | “Maybe you aren’t thinking clearly …” |
| Approving, praising, agreeing | “I couldn’t agree more …” |
| Ridiculing, labeling, shaming | “Men do tend to think that way …” |
| Sympathizing, consoling, or reassuring | “Look on the bright side …” |
| Probing with questions | “Why did you do that?” |
| Interpreting or analyzing | “What you’re doing is …” |
| Humoring, changing the subject, distracting, withdrawing | “Let’s talk instead about what’s going well …” |
(Gordon, n.d.)
Eliciting Change Talk
It is said that the more an individual talks about change, the more likely they are to change. Change talk consists of responses the clinician elicits from patients. Patients’ responses normally contain reasons for change that are important to them personally. Elements of change talk can be remembered using the mnemonic DARN-CAT.
| (NCNC, n.d.) | |
| Desire | “I want to stop overeating.” |
| Ability | “I know I can give up eating too many sugary foods.” |
| Reason | “It’s important to change because my blood sugars have been too high.” |
| Need | “I should really lose weight because of my high blood pressure and diabetes.” |
| Commitment | “I will make changes to my diet for my own health!” |
| Activation | “I am ready, prepared, and willing to change, starting now!” |
| Taking Steps | “My first action step will be going to the bookstore today to buy a weight-reduction cookbook for persons with diabetes.” |
The clinician elicits change talk by:
- Asking evocative questions (what, when, where, how) and avoiding “why” questions
- Exploring decisional balance (pros and cons of change)
- Asking for elaboration or example (“Tell me more about …”)
- Looking back to the time before the onset of the behavior (“How was it different/better?”)
- Looking to what life would be like a few years from now (goals and values)
- Asking about extremes (“What are the worst things that may happen if change does not occur, and what are the best things if it does?”)
- Siding with the status quo (“Drinking is so important to you that you won’t stop no matter what it costs you.”)
(Motivational Interviewing, n.d.)
It is important that clinicians elicit more information than they provide, ask rather than tell, and listen rather than advise. In order to provide information to the patient, the clinician should first find out what the patient already knows and then ask permission to add more.
- “What do you know about how smoking affects your circulation?”
- “I have some information about how to begin an exercise program. Would you be interested in hearing about it?”
CASE
Change Talk
Janet is 62 years old, 5 feet 7 inches tall, and weighs 201 pounds. She has been diagnosed with type 2 diabetes and is taking metformin (Glucophage), 500 mg, twice a day. Today Janet is returning to the clinic for her three-month follow-up visit. Her A1C level from yesterday was 7.9% (average blood glucose 180), and her log of blood sugar readings shows less than optimal control.
Clinician: “Hello, Janet. Nice to see you again. Tell me, how are things going with you?” (open question)
Janet: “Well, pretty good. I’m not very happy about my blood sugar readings, though.” (evoked elaboration)
Clinician: “You say your blood sugar readings are not where you want them.” (rephrasing)
Janet: “No, they’re not! And I’m really upset about that because I thought I was doing pretty well with everything.” (evoked elaboration)
Clinician: “You sound quite upset.” (mirroring)
Janet: “I am! I know it’s my fault. I’m having a real hard time sticking to this diet and trying to lose weight.” (evoked elaboration)
Clinician: “You’re blaming yourself for not sticking to the changes needed to keep your blood sugars under control.” (reflecting)
Janet: “That’s right. I have a hard time passing up desserts, and I love my wine with dinner.” (evoked elaboration)
Clinician: “Giving up desserts and wine is very hard for you.” (reflecting)
Janet: “Yes. I’m a foodie and a wino (laughs).” (asking for empathy)
Clinician: “I understand and can certainly relate to that!” (empathizing)
Janet: “You know, I just can’t understand why it’s so hard for me to lose weight. I’ve lost at least 500 pounds during my lifetime. But eventually I gain it all back.” (elaborating)
Clinician: “You’ve been successful at losing weight in the past.” (affirmation)
Janet: “Yes, I have, but eventually it gradually creeps back on.” (elaborating)
Clinician: “It sounds like you want to stick to your diet and lose weight, but you still want to enjoy the foods you like. That sounds like a dilemma to me.” (summarizing)
Janet: “It is. I know how important it is to manage my diabetes, and I really want to change things. I want to live long and healthy to see my grandchildren grow up. I know I can change but just can’t quite manage to.” (change talk)
Clinician: “Let’s see now, you’re telling me how important it is to be in good health in order to see your grandchildren grow up. At the same time, you’ve told me how eating the foods you like and drinking wine are important to you.” (developing and examining discrepancy)
Janet: “Both of those are true. But I really do want to be there for them, and I believe I really can make some changes.” (change talk)
Clinician: “You have strong motivations for wanting to change, and you believe you are capable of changing.” (supporting self-efficacy)
Janet: “Yes, yes. I do.” (change talk)
Clinician: “Well, Janet, tell me what you think you can do to make these changes.” (finding out what the patient already knows)
Janet: “Well, I know about the Atkins Diet, the South Beach diet, the Grapefruit Diet, and any other weight loss program you can name.” (elaborating)
Clinician: “That’s a lot of information you already have. Tell me, though, would you be interested in learning some other ways to accomplish your goals?” (asking permission to give information)
Janet: “I could be. What other suggestions do you have?” (collaborating)
Clinician: “Would you perhaps be interested in attending meetings with other people who have diabetes and are experiencing the same difficulties you are?” (collaborating)
Janet: “Well …, I don’t really think that would be good for me.” (resisting)
Clinician: “You think that you wouldn’t want to be in a group?” (rolling with resistance)
Janet: “Well, group ‘therapy’ always seems to me to be about being too weak to do something on your own.” (evoked elaboration)
Clinician: “You believe others in the group will think you’re too weak on your own.” (reflecting)
Janet: “Yeah. But … maybe I could give it a try.” (collaborating and negotiating)
Clinician: “Would you like me to arrange for you to attend our diabetes education classes?” (collaborating, negotiating a plan, empowering)
Janet: “Yeah. Okay. Why don’t we try that.” (collaborative response)
CONCLUSION
Change is hard, but change is not impossible. This is a fact that healthcare providers should remember when feeling frustrated by a patient’s failure to make changes known to improve their health and well-being. Understanding the nature of change, the stages of change, and factors affecting change can assist the clinician to remain supportive rather than dismissive of someone’s ability or willingness to change.
Using a variety of supportive techniques, healthcare professionals can help guide their patients through the process of change by collaborating with them, negotiating action plans with them, empowering them, and supporting their self-efficacy. Making change possible can result in a well-deserved sense of satisfaction for both clinicians and patients.
REFERENCES
Alyafei A, & Easton-Carr R. (2024). The health belief model of behavior change. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK606120/
American Medical Association. (2023). 8 reasons patients don’t take their medications. https://www.ama-assn.org/delivering-care/patient-support-advocacy/8-reasons-patients-dont-take-their-medications
American Psychological Association (APA). (2023). Harnessing willpower to meet educational goals. https://www.apa.org/topics/schools-classrooms/harnessing-willpower
American Psychological Association (APA). (2012). What you need to know about willpower: The psychological science of self-control. https://www.apa.org/helpcenter/willpower
Badillo-Diaz MA. (2025). 50+ examples of therapy goals and objectives. https://heyberries.com/blog/articles/examples-of-therapy-goals
Brookes E. (2023). The theory of planned behavior: Behavioral intention. Simply Psychology. https://www.simplypsychology.org/theory-of-planned-behavior.html
Cambridge Dictionary. (2025). Motivation. https://dictionary.cambridge.org/us/dictionary/english/motivation
Centers for Disease Control and Prevention (CDC). (2024a). Smoking cessation: Fast facts. https://www.cdc.gov/tobacco/php/data-statistics/smoking-cessation/index.html
Centers for Disease Control and Prevention (CDC). (2024b). Develop SMART objectives. https://www.cdc.gov/youth-advisory-councils/action-plans/smart-framework.html
Gordon T. (n.d.). The roadblocks to communication. Gordon Training International. http://www.gordonmodel.com/work-roadblocks.php
Grandison T. (2022). 5 steps to being an effective change agent. GovLoop. https://www.govloop.com/community/blog/5-steps-effective-change-agent/
Haracz K. (2025). Occupational therapy and health promotion. In P Liamputtong (Ed.), Handbook of concepts in health, health behavior and environmental health, Springer Singapore. https://doi.org/10.1007/978-981-97-0821-5
Hartney E. (2023). Understanding motivational interviewing. Verywellmind. https://www.verywellmind.com/what-is-motivational-interviewing-22378
Harward H. (2022). How to use the 5 As model to help your patients lose weight. MDatl.com. https://mdatl.com/2022/10/how-to-use-the-5-as-model-to-help-your-patients-lose-weight/
Hood J. (2025). The benefits and importance of a support system. Highland Springs Clinic. https://highlandspringsclinic.org/the-benefits-and-importance-of-a-support-system/
Ingersoll K. (2024). Motivational interviewing for substance use disorders. UpToDate. https://www.uptodate.com/contents/motivational-interviewing-for-substance-use-disorders?source=search_result&search=motivational%20interviewing&selectedTitle=1~50
Luque M. (n.d.). Behavior change science: Help clients stick with their program. National Academy of Sports Medicine. https://blog.nasm.org/behavior-change-and-motivation/behavior-change-science/
Lynch SS. (2025). Adherence to a drug regimen. Merck Manual. https://www.merckmanuals.com/professional/clinical-pharmacology/factors-affecting-response-to-drugs/adherence-to-a-drug-regimen
Motivational Interviewing. (n.d.). Ten strategies for evoking change talk. https://www.motivationalinterviewing.org/sites/default/files/Ten%20Strategies%20for%20Evoking%20Change%20Talk%20Sue%20EckMaahs.pdf
Nickerson C. (2025). Albert Bandura’s social cognitive theory. Simply Psychology. https://www.simplypsychology.org/social-cognitive-theory.html
North Carolina Network Consortium (NCNC). (n.d.). DARN-CAT of change talk. https://ncnc.unc.edu/files/2015/04/change-talk-cheat-sheet.pdf
Nundy S, Cooper LA, & Mate KS. (2022). The quintuple aim for health care improvement: A new imperative to advance health equity. JAMA, 327(6), 521–22. https://doi.org/10.1001/jama.2021.25181
Raihan N & Cogburn M. (2023). Stages of change theory. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK556005/
Tinker A. (2025). The top seven healthcare outcome measures and three measurement essentials. Health Catalyst. https://www.healthcatalyst.com/insights/top-7-healthcare-outcome-measures
University of Maryland Baltimore County (UMBC). (n.d.). About the TTM: The transtheoretical model of behavior change. https://habitslab.umbc.edu/the-model/





Customer Rating
5.0 / 173 ratings