Diabetes in Children and Adolescents
Symptoms and Management
Online Continuing Education Course

Course Description
Type 1 and type 2 diabetes diagnoses in youth are increasing. Learn about prediabetes, symptoms, and patient management for T1D and T2D in children and adolescents.
Note: This course is also available as part of a package. See Nursing CEU Bundle - 30 ANCC Hours
Course Price: $24.00
Contact Hours: 3
Course updated on
November 1, 2024
"Well presented material, the pathophysiology of diabetes is explained clearly and would be a useful tool for educating a patient and their family." - Meliza, RN in California
"Excellent course. Comprehensive and very thorough." - Kathy, RN in Delaware
"I thoroughly enjoyed this article. The information will be used in my personal and professional life." - Stephanie, RN in New Jersey
"The course provided a wealth of knowledge for me as a professional and for my family." - Sherri, RN in Virginia
Diabetes in Children and Adolescents
Symptoms and Management
Copyright © 2024 Wild Iris Medical Education, Inc. All Rights Reserved.
LEARNING OUTCOME AND OBJECTIVES: Upon completion of this continuing education course, you will have increased your understanding of the impact of diabetes on children and adolescents. Specific learning objectives to address potential knowledge gaps include:
- Describe the diagnosis of diabetes in children and adolescents.
- Summarize diabetes treatment and management strategies in youth.
- Explain the medical complications associated with diabetes in children and adolescents.
- Outline the common challenges facing youth with diabetes and their families.
- Discuss the transition from pediatric to adult diabetes care.
TABLE OF CONTENTS
- Introduction
- Diagnosis for Diabetes in Children and Youth
- Diabetes Management in Children and Adolescents
- Medical Complications Associated with Diabetes in Children
- Challenges Facing Children with Diabetes and Their Families
- Issues Facing Adolescents with Diabetes
- Transition to Adult Care
- Conclusion
- Resources
- References
INTRODUCTION
While diabetes affects children of all ages, impacts of diabetes vary among different age groups. For instance, parents of toddlers with diabetes may have to address erratic eating habits of their children when trying to dose insulin. Parents of grade schoolers may be worried about managing diabetes in their children who want to play sports. Many adolescents find it difficult to adjust to a diagnosis of a chronic condition they see as curtailing their freedom and choices—one that sets them apart from their peers during a time when peer acceptance is essential to their well-being.
Type 2 diabetes prevalence among youth ages 10–19 years has doubled in the United States over the past two decades. Significantly higher rates have been reported in Black and Native American adolescents. Upward trends in the incidence of type 1 diabetes have also been found. A primary factor in the rise of type 2 diabetes is the increasing rates of youth obesity. However, this is not the only predisposing factor, since the incidence of prediabetes in youth has demonstrated a much higher increase than the rate of obesity. Other factors to be studied include the role of genomic factors in the development of type 2 diabetes (Bloomgarden, 2023).
With these increases in diabetes among youth, clinicians must be equipped with a wide range of knowledge in order to provide care to children with diabetes and their families. Clinicians can be pivotal in fostering the development of positive skills to manage this disease.
DIAGNOSIS FOR DIABETES IN CHILDREN AND YOUTH
The most frequent period of onset of type 1 diabetes (T1D) is during childhood. T1D can be diagnosed at any age, but for children, the two peak periods are from the ages of 5–6 years and 11–13 years. There also appears to be a seasonal disparity, with a higher number of cases being diagnosed in the fall and winter months. In contrast to other autoimmune conditions, T1D is marginally more prevalent in boys and men. Some of the most rapid increases in T1D prevalence have been in young children (Los & Wilt, 2023).
The initial signs and symptoms of T1D can include:
- Thirst
- Increased urination
- Onset of bedwetting in children who have already gained continence
- Increased appetite
- Weight loss
(AAP, 2020; Children’s Health Care of Atlanta, 2022)
In around one third of children, the first presenting sign of T1D is diabetic ketoacidosis (see also “Diabetic Ketoacidosis” later in this course) (El-Mohandes, 2023).
Missed diagnosis for T1D in children is common. Many times, when a child is brought to the pediatrician’s office with listlessness, weight loss, increased thirst, nausea, and possible vomiting, the initial diagnosis may be stomach flu. It is important to be aware that these flu-like symptoms are also the symptoms of T1D.
Approximately 40% of children with type 2 diabetes (T2D) have no obvious symptoms, and the condition is often diagnosed during routine physical examinations. The ADA recommends screening for prediabetes and T2D in children and adolescents who:
- Are overweight or obese, with severe obesity recognized as the most important danger for the development of T2D in children (Pinhas-Hamiel, 2023)
- Have a first- or second-degree relative with T2D
- Identify as Native American, African American, Latino, Asian American, or Pacific Islander
- Exhibit signs of insulin resistance or have disorders related to insulin resistance, such as acanthosis nigricans (dark discoloration and thickness of skin in skin folds and creases), hypertension, dyslipidemia, or polycystic ovary syndrome
(ADA, 2024a)
Blood tests are used to diagnose diabetes as well as to monitor diabetes management in children:
- A random blood glucose level of 200 mg/dL (11.1 mmol/L) or higher or a fasting blood sugar level of 126 mg/dL (7.0 mmol/L) or higher, along with symptoms, suggests diabetes.
- A glycated hemoglobin (A1C) test indicates the average blood sugar level for the past three months; an A1C level of 6.5% or higher on two separate tests indicates diabetes.
Additional tests are given to distinguish between type 1 and type 2 diabetes (Mayo Clinic, 2023a).
DIABETES MANAGEMENT IN CHILDREN AND ADOLESCENTS
The overarching goal for treating and managing diabetes in children is centered around maintaining normal physical growth and positive psychosocial development by establishing good glycemic control and preventing acute and chronic complications, as far as possible (March et al., 2023). Managing and treating diabetes is lifelong and may include:
- Pharmacotherapy
- Monitoring blood glucose
- Preventing hypoglycemia
- Nutritional therapy
- Physical activity
- Sick-day planning
- Exercise
Pharmacotherapy
Insulin therapy is the primary treatment for type 1 diabetes and is also often implemented for type 2 diabetes. Insulin needs for children will fluctuate significantly as the child grows.
Pharmacotherapy for patients with type 2 diabetes is described below:
- For youths with type 2 diabetes with an A1C <8.5% and normal renal function, Metformin is the primary medication of choice.
- Those with significant hyperglycemia and an A1C >8.5% and who do not present with acidosis at the time of diagnosis are started on long-acting insulin while Metformin is begun and titrated.
- Patients who present with acidosis require subcutaneous or intravenous insulin to correct the acidosis. Once this problem has been cleared, the patient is started on a titrated dose of Metformin.
- If Metformin is not successful in meeting the glycemic goals set for the patient, with or without the use of long-acting insulin, glucagon-like peptide 1 (GLP-1) receptor agonist treatment and/or empagliflozin is contemplated for children ages 10 years and above.
- In children who are meeting their glycemic goals with the use of Metformin and adjunctive insulin therapy, insulin therapy can be decreased over a two- to six-week period by reducing the insulin dosage at a rate of 10%–30% every few days.
(ADA, 2024a)
Metformin has been found to be a safe and efficient medication in diabetic management. The most common side-effects are gastrointestinal upset with diarrhea and abdominal discomfort; this can usually be alleviated by slow dose titration (ADA, 2024a).
GLP-1 receptor agonists are highly effective therapies used in the treatment of type 2 diabetes and attaining weight loss (Wang et al., 2024). They are given via injection, with the frequency varying from once a day to once a week. The most common side effects are loss of appetite, nausea, vomiting, and diarrhea (Cleveland Clinic, 2023).
Empagliflozin is a sodium-glucose co-transporter 2 (SGLT2) inhibitor. It decreases blood glucose levels by triggering the kidneys to excrete more glucose in urine. It comes in tablet form and is normally taken once daily in the morning. It is FDA approved for use in adults and children 10 years of age and older who have type 2 diabetes. Hypoglycemia and ketoacidosis are serious side effects of this medication. Other side effects include increased urination at night, dehydration, bladder infections, and vaginal infections in females (Medline Plus, 2024; Drugs.com, 2024).
HONEYMOON PERIOD
Approximately 62% of children with T1D may experience partial remission, sometimes referred to as a honeymoon period. The duration of the remission varies from six weeks to two years. During remission, the pancreas continues to produce some insulin, decreasing and sometimes eliminating the need for treatment. However, once the honeymoon period ends, there is an increased need for insulin therapy. Family education on what is happening during this period is important so that families are aware that diabetes has not gone away and they are prepared for the time when insulin treatment will need to be increased (ADA, 2023b).
Monitoring Blood Glucose
The recommendation for children with T1D is for blood glucose checks before meals and at bedtime. This necessitates some blood glucose checks to be done while the child is at school or daycare. Children with T2D will also require several blood glucose checks daily, especially if they have begun insulin therapy (Mayo Clinic, 2023a, 2023b).
The ADA recommends continuous glucose monitoring (CGM) for children and youth with T1D. CGM can be used for children as young as 2 years. Research has also shown that CGM improves the quality of life for adolescents with T1D and decreases levels of diabetes distress. While strong evidence exists for the use of CGM in those with T1D, less evidence exists for its use in T2D (ADA, 2024a; Rubelj et al., 2021; Lin et al., 2021).
A continuous glucose monitor will automatically screen blood glucose levels. Fingersticks are still required to calibrate the device and to confirm an out-of-range glucose reading before instigating treatment.
The monitor may be a stand-alone device or part of an insulin pump. Some monitors transmit information directly to a smartphone. The sensor performs glucose testing every few minutes, making it possible for the patient or caretaker to see the blood glucose level at a glance at any time of day. Apart from reducing the number of fingersticks, continuous glucose monitoring allows for more accurate decision-making regarding balancing food, exercise, and medications (Rubelj et al., 2021).
Parents and caregivers must be made aware of the learning curve involved in switching to CGM from fingerstick, and the patient’s diabetes management team must assess the family’s willingness and motivation to invest the time and effort needed to successfully use CGM.
Preventing Hypoglycemia
Hypoglycemia is a major concern for children with diabetes, especially hypoglycemia occurring during the night. Symptoms of hypoglycemia include:
- Shakiness, which may manifest as slight shaking or trembling
- Sweating on the face and over the body, comparable to the sweating that occurs with exercising
- Feeling of hunger, often developing suddenly and felt more intensely the lower the blood glucose levels
- Fast heartbeat
- Inability to concentrate
- Dizziness or lightheadedness
- Irritability or moodiness
- Anxiety or nervousness
- Headache
- Paleness, clammy feeling
(Mayo Clinic, 2023a; Diabetes Care Community, 2021)
Young children are not always able to express in words what they are feeling, and a child refusing to sleep, showing signs of irritability, or crying may be experiencing hypoglycemia. A blood glucose check can determine if hypoglycemia is the cause of such behaviors (Rocky Mountain Diabetes Center, 2024).
Preventing episodes of hypoglycemia is best achieved by monitoring blood glucose levels before meals and at bedtime. Additionally, checking blood glucose before, during, and after exercise or sports indicates how these activities affect a child’s blood glucose levels and may indicate the need for a snack before or after exercise or playing sports. Changes in insulin dosing may also be required on days when the child is more active (ADA, 2023c).
Children under the age of 6 years who are diagnosed with diabetes are highly susceptible to serious side effects from episodes of severe hypoglycemia, including cognitive deficits and brain abnormalities (Faradji et al., 2023).
NOCTURNAL HYPOGLYCEMIA
Nocturnal hypoglycemia is frequent in children with diabetes, usually occurring in the earlier part of the night. It correlates with bedtime blood glucose values of <150 mg/dL (Childs et al., 2017).
For children with nocturnal hypoglycemia, middle-of-the-night blood glucose monitoring is advisable. A middle-of-the-night blood glucose test is also recommended after a child has participated in strenuous exercise or sports activities because a child with diabetes can develop hypoglycemia several hours after the activity or exercise. Testing at midnight and again at around 3 a.m. on a weekly basis can help identify a pattern in a child’s nocturnal blood glucose levels and assess whether changes to diabetes management are successful or not (Nye, 2024).
TREATING HYPOGLYCEMIA IN CHILDREN
Consuming Carbohydrates
Hypoglycemia in children is treated by consuming 15 grams of carbohydrates. Good carbohydrate sources for children are 4-ounce juice boxes, regular soda, nonfat milk, and raisins. Parents are instructed to wait for 15 minutes and then recheck the child’s blood sugar. If it is still low (<70 mg/dL), the child is treated with a second 15 grams of carbohydrates.
Foods containing fats, such as chocolate, should not be used to treat hypoglycemia, since the fat content can hinder the action of the carbohydrates and thus extend the acute hypoglycemic episode.
Glucagon Administration
A glucagon injection is indicated when the individual is exhibiting signs and symptoms of hypoglycemia and cannot safely swallow food or fluids, is unconscious, or is having seizure activity. A nasal powder form (Baqsimi) can be administered even to a patient who is unconscious since it does not need to be actively inhaled but is absorbed through the nasal tissue. Side effects can include vomiting, headache, flushing, and a rapid heartbeat. Once the child is alert and can safely swallow, oral carbohydrates can be provided (NCH, 2024; Children with Diabetes, 2024).
HYPOGLYCEMIA UNAWARENESS
Hypoglycemic unawareness happens when a person fails to recognize the warning symptoms that precede an episode of hypoglycemia. This can result from frequent episodes of severe hypoglycemia. Many children with T1D experience hypoglycemic unawareness. Very young children are more profoundly affected by repeated episodes of hypoglycemia since their central nervous system is still in the process of maturing, putting them at greater risk for cognitive deficits and behavioral problems.
Hypoglycemic unawareness in children is usually treated by changing the child’s blood glucose range to a higher level for several weeks. This is achieved by performing at least four blood glucose checks during the day. Blood glucose checks at night may also be recommended. The goal is to help the child recover an awareness of their typical sensations of low blood glucose levels (Abraham et al., 2022).
Medical Nutritional Therapy
At the time of diagnosis with diabetes, the child is referred for individualized medical nutritional therapy to a registered dietitian with experience in managing children with diabetes. Yearly follow-up visits are included in the child’s comprehensive plan of care (ADA, 2024a).
Nutritional therapy is geared toward the child’s age and stage of development. The goal is to help the child reach and maintain a healthy weight, and meal planning is based on the number of calories a child needs for growth. Strategies may include:
- Teaching parents and children about portion control
- Aiming for three meals and three snacks daily
- Planning each meal to contain the same amount of carbohydrates
- Including healthy fats in the diet
- Not regarding a particular food as “off-limits,” while teaching how different foods affect blood glucose and how and when certain foods, especially treats, should be included into the meal plan
- Working with parents to set a goal for the whole family to gradually replace soda and other sugary drinks (e.g., juices, sports drinks) with plain water or low-fat milk
- Teaching parents and children about the importance of reading food labels and how to understand what they mean
(NIH, 2021)
Toddlers and preschoolers require morning, afternoon, and bedtime snacks to ensure a ready source of glycogen. However, very young children may not complete a meal or snack, which makes it extremely difficult to safely dose insulin prior to meal times. In these instances, rapid-acting insulin analogs given after a meal are recommended, with the insulin dose based on what the child actually ate (Childs et al., 2017).
For school-age children, medical nutritional therapy must take into account meals at school, afterschool events, sporting activities, parties, eating out, sleepovers at friends’ houses, the child’s changing food tastes, and so forth (Childs et al., 2017). Parents and school-age children are encouraged to develop meal plans together, in part to help children acquire the skills to become more independent by learning about carbohydrate counting and planning their own food choices and portion sizes.
Adolescents can be more involved in their own care by monitoring their carbohydrate intake and individualizing their meal plan based on greater awareness of their food preferences (ADA, 2024a).
Nutritional therapy takes into account the child and family’s dietary habits, cultural or religious considerations, financial resources, and mathematical ability to successfully count carbohydrates (ADA, 2020a). For many children with diabetes, it is important to ensure they are not singled out as needing “special foods” or missing out on the treats enjoyed by siblings or peers. For example, the dietitian may suggest limiting dessert to once a week or adopting certain foods for the entire family.
Physical Activity
Exercise is recommended for children with diabetes. Participating in sports promotes physical and psychological well-being and helps to maintain blood glucose control. Children with diabetes indicate that being involved in sports and other extracurricular activities helps them to cope with having a chronic condition and allows them to “feel normal,” but fewer children with diabetes participate in sporting activities and other extracurricular activities compared to those without diabetes (UC Davis Health, 2024; Davis et al., 2023).
Fear of hypoglycemia is the main deterrent to participating in sports. Therefore, a diabetes management plan includes recommendations for physical activities and ways to prevent, detect, and treat episodes of hypoglycemia, such as more frequent blood glucose checks and adjusting insulin doses, meals, and snacks on days when the child participates in physical activities and sports (Childs et al., 2017; Davis et al., 2023).
The ADA and the American Academy of Pediatrics recommendations for children with diabetes include at least 60 minutes of moderate to strenuous physical activities every day. Further ADA physical activity recommendations include:
- A pre-exercise glucose level of 90–250 mg/dL
- Access to sources of carbohydrates before beginning physical activity or participation in sports
- A kit for the child to take to physical activity (e.g., team practices and games) that has snacks, glucose tablets, fruit juices, water, and medications recommended by the diabetes management team
- For organized sports activities, coaches who are aware that the child has diabetes
- Medical identification bracelets during all physical activities and sports events
- Education on the importance of taking a break from activities if something starts to feel wrong, even in the middle or near the end of a game
- Reducing the insulin dosage for the meal prior to the physical activity
- A bedtime snack after physical activity
- Frequently monitoring blood glucose levels before, during, and after physical activity regardless of whether or not CGM is employed, to identify out-of-range blood glucose levels occurring with physical activity
(ADA, 2024a; Davis et al., 2023)
Sick-Day Planning
Having a practical and workable plan for sick-day management is essential and must be put in place as soon as diabetes is diagnosed (Childs et al., 2017).
Important elements of a sick-day plan include:
- Never stopping taking insulin or diabetic medications
- Maintaining fluid intake (since dehydration can lead to diabetic ketoacidosis [DKA])
- When vomiting occurs, considering it to be a sign of insulin deficiency until confirmed differently
- Treating the underlying condition
- Implementing more frequent blood glucose checks (every 2–4 hours)
- Checking for ketones in urine
(Dartmouth Health Children’s, 2024; Cleveland Clinic, 2024)
The intake goal is 15 grams of carbohydrates per hour. Typically, the child is encouraged to drink small amounts of fluids, around 1/2 cup every hour, slowly and without taking large mouthfuls. Some recommended sick-day foods to avoid hypoglycemia include:
- Jello
- Saltine crackers
- Applesauce
- Bananas (or other fruit)
- Toast
- Rice
- Soup
- Graham crackers
(Cleveland Clinic, 2024)
Families are instructed to contact their provider or emergency contact if the child show signs of DKA, including frequent vomiting, deep or rapid respirations, inability to drink or tolerate fluids, moderate or large ketones or ketones that don’t clear after two correction doses (Children’s Health, 2024).
MEDICAL COMPLICATIONS ASSOCIATED WITH DIABETES IN CHILDREN
Children with both types 1 and 2 diabetes are at risk for several complications. Young children diagnosed with diabetes have a potentially greater risk for microvascular complications as they proceed into their adult years compared to their peers without a diagnosis of diabetes. The types of complications are also similar between forms of diabetes, but there is a difference in prevalence rates.
- Retinopathy can occur more frequently in youth with type 1 diabetes.
- Microalbuminuria and hypertension occur more often in youth with type 2 diabetes.
- Diabetes-related complications occur at a younger age in youth with type 2 diabetes compared to those with type 1 diabetes.
The presence of diabetes is a major risk factor for earlier mortality related to cardiac disease. Research shows that the risk of cardiac disease and acute myocardial infarction has a 30-times increase in those who are diagnosed with type 1 diabetes before the age of 10 (Tamborlane, 2021).
Complications and Type 1 Diabetes
Medical complications of type 1 diabetes in youth may include diabetic ketoacidosis, cardiovascular diseases, retinopathy, and diabetic neuropathy.
DIABETIC KETOACIDOSIS (DKA)
One of the most serious complications for children with T1D is diabetic ketoacidosis. The condition can develop slowly, but without treatment it is fatal. DKA is the most pervasive cause of mortality in children with T1D (Childs et al., 2017). DKA has also been proven to result in serious consequences for brain development and function (ADA, 2024a).
Signs of DKA include:
- Excessive thirst
- Dry mouth
- Weakness
- Lethargy
- Fruity breath-smell
- Nausea
- Vomiting
- Abdominal pain
- Difficulty breathing
Once vomiting occurs, the child’s condition can quickly deteriorate to full-blown DKA within a matter of a few hours. A child with DKA requires immediate medical treatment to correct dehydration and bring blood glucose levels back down to normal. Acute kidney injury can occur in children during episodes of DKA; research has found that this can lead to slight cognitive impairment, which includes short-term memory loss and decreased IQ scores (Zolot, 2021; Abraham et al., 2022).
CARDIOVASCULAR DISEASE
Data indicate that 14%–45% of children with T1D develop two or more atherosclerotic cardiovascular diseases (ADA, 2024a). Cardiovascular disease risk factors are highest among minority youth, and girls are at higher risk than boys.
ADA recommendations for screening of cardiovascular disease in children and youth with T1D include:
- Blood pressure measurement at each visit using an appropriate-size cuff for a child
- Lipid evaluation shortly after diagnosis with T1D
Treatment interventions focus primarily on lifestyle modifications, with emphasis on dietary modifications and exercise (ADA, 2024a).
RETINOPATHY
Retinopathy is another major medical complication associated with T1D. Problems with retinopathy most frequently occur after the start of puberty and after the presence of T1D for 5 to 10 years.
ADA recommendations for retinopathy screening include:
- A comprehensive eye examination, along with dilation, for a child who is at least 11 years of age or older or who has reached puberty and is three to five years postdiagnosis with T1D, whichever happens first
- A comprehensive eye exam with dilation every two years, which may be extended to every four years on the advice of an eye care specialist
Parents should seek out an eye specialist with expertise in diabetic retinopathy in youth and who can provide counseling in prevention measures and signs and symptoms to observe for in order to ensure early detection (ADA, 2024a).
NEUROPATHY
Diabetic neuropathy is not commonly found in children with T1D before puberty or within the first one to two years following onset of diabetes. The ADA recommends a yearly foot examination beginning at the onset of puberty or at age 10, whichever occurs first. The ADA also recommends a complete clinical foot inspection during each routine visit as a means to educate the young person on the importance of foot care (ADA, 2024a).
Complications and Type 2 Diabetes
Compared to youth with T1D, medical complications are higher in youth with T2D. Likewise, studies show that T2D is a more severe disease in children than in adults. In children with T2D, complications start developing within a few years of diagnosis.
The rates of T2D are higher in racial/ethnic minorities. Youth with T2D may already have other health conditions present at the time of diagnosis, similar to those discussed above for T1D. Other problems unique to T2D must also be taken into account.
COMPLICATIONS
Kidney disease is a frequent complication of T2D in children (Sun et al., 2022). There is a faster ongoing deterioration in beta-cell function in youth with T2D than in adults with T2D.
The development of vascular defects, including ischemic heart disease and stroke, seems to be more prominent in youth with T2D compared to youth with T1D with a similar duration since diagnosis. Micro- and macrovascular changes are among the most serious medical complications of T2D in this population, which heightens their risk of cardiovascular disease and death at a younger age when compared to those diagnosed with T2D at later stage in life. It is believed that this increased susceptibility to adverse cardiovascular events is due to the greater lifetime exposure to hyperglycemia and other variants associated with T2D, such as insulin resistance, dyslipidemia, high blood pressure, and chronic inflammation (ADA, 2024a).
Other complications include:
- Polycystic ovary disease
- Hyperandrogenism
- Sleep apnea
- Hepatic steatosis
(ADA, 2024a)
SCREENING RECOMMENDATIONS
ADA recommendations for screening youth who are newly diagnosed with T2D include:
- Screening for retinopathy at the time of diagnosis or shortly thereafter
- Evaluation for nonalcoholic fatty liver disease at the time of diagnosis, using AST and ALT measurements, and follow-up testing yearly
- Screening for symptoms of sleep apnea, snoring, restless sleep, and morning headache at each visit and, if necessary, referral to a pediatric specialist for further evaluation
- For adolescent girls with T2D, assessing for menstrual problems and, if warranted, polycystic ovary disease
- Lipid screening once glycemic control has been established, repeated yearly
- Baseline foot exam at the time of diagnosis and on a yearly basis to monitor for neuropathy
(ADA, 2024a)
CHALLENGES FACING CHILDREN WITH DIABETES AND THEIR FAMILIES
There are many challenges facing children with diabetes and their families, and the clinician must be ready to address these challenges when caring for pediatric patients.
Managing Diabetes in School Settings
Several particular challenges and concerns must be addressed and overcome during a child’s transition into daycare and then school.
DAYCARE AND DIABETES
A primary concern with very young children with diabetes is whether the child can attend daycare. Before doing so, the child’s healthcare team and parents must develop a written plan of care for the child, and the parents then review the plan with the daycare administration and staff. It is essential that there is always at least one daycare staff member present who has been trained to perform blood glucose checks and to administer insulin if needed. It is the responsibility of the parents to provide the daycare facility with all the diabetes supplies that their child will need, as well as the prescribed insulin and snacks (March et al., 2023).
DIABETES AND DISCRIMINATION LAWS
Federal and state laws protect against discrimination against children with diabetes. The legal protections against discrimination for children with diabetes are covered under the Americans with Disabilities Act of 1990 and section 504 of the Rehabilitation Act of 1973 (see below). Clinicians can provide parents with related resources, such as contact information for the American Diabetes Association, which can provide specific details of the laws in their state (ADA, 2023a).
DIABETES CARE AT SCHOOL
During the school day, students must perform blood glucose checks, follow a healthy diet, and self-administer insulin or manage an insulin pump. These activities are carried out with assistance and supervision from the school nurse, who develops an emergency care plan (ECP) based on the primary healthcare provider’s orders. The nurse ensures that all school personnel interacting with the child are provided with copies of the ECP and know how to act upon its instructions (NIDDK, 2020).
Likewise, a “504 Plan” (which refers to section 504 of the Rehabilitation Act of 1973) may be put in place for students with diabetes to ensure that they are medically safe while having the same educational opportunities as other students. A 504 Plan is individualized to meet the needs of each child with diabetes and can stipulate requirements such as permission to eat whenever and wherever necessary, added trips to the restroom, and alternate provisions for class time missed due to medical appointments.
Parent interventions include meeting with the child’s teachers and discussing with them the specific signs and symptoms their child may exhibit when their blood glucose level is dropping, such as becoming irritable or nervous or complaining of feeling hungry or dizzy (CDC, 2024).
DIABETES SUMMER CAMPS
The American Diabetes Association offers camps in most states for children with diabetes. Physicians, nurses, and counselors experienced in treating diabetes are on staff and provide 24-hour supervision. These camps provide physical and emotional benefits to children with diabetes as well as improve their skills in diabetes self-management. Post-camp assessments have indicated that at least 99% of children were able to perform a minimum of one diabetes management skill independently and that 36% of parents and caregivers reported a considerable increase in family teamwork after attending camp (ADA, 2023a).
Children with diabetes also attend “regular” summer camps, which are legally required to make “reasonable modifications” to ensure that all children can safely participate in the activities offered. Reasonable modifications may include training staff to perform or assist with blood glucose monitoring, to recognize the signs of hypoglycemia, and to administer glucagon. However, camps are not compelled to provide modifications if it would entail a change to the basic nature of their program. For instance, a camp is not required to employ a full-time staff member to provide diabetes care if health-related care is not normally a feature of the program (ADA, 2024c).
Addressing Emotional and Psychosocial Issues
Diabetes management places an emotional burden on both the family and the child with diabetes. Quality of life can be compromised, and mental health issues can develop. In addition to dealing with the day-to-day burden of managing the condition, the physiology of diabetes can directly affect emotions. The ADA recommends including mental health professionals skilled in the area of childhood diabetes as part of the diabetes management team.
CHILDREN’S COMMON EMOTIONAL REACTIONS
Young children may express “magical thinking,” such as a belief that insulin shots will make their diabetes go away. Some may believe that the shots are a punishment for misbehaving or express fear of needles and injections (Better Health Channel, 2021).
School-age children (7–8 years) struggle with the reality of requiring insulin shots for the rest of their lives. Children at this age may ask themselves, “What bad thing did I do to cause this, and what can I do to make it right?” Children may not vocalize these thoughts to their parents or the diabetes care team (Kenowitz, 2022).
Another common concern is feeling different from other children, leading to social isolation. Children may then deny that they have diabetes or believe that it will go away. Left unaddressed, such thinking may lead to serious consequences, such as the child not taking their insulin or refusing to follow dietary recommendations (Kenowitz, 2022).
Research findings suggest that youth with diabetes have higher rates of anxiety, depression, and psychological distress compared to those who do not have diabetes. Depression is the most frequently occurring mental health condition in children and adolescents with diabetes. Research shows that suicidal thoughts are common among adolescents with type 1 diabetes (Tamborlane, 2021). Children with poorly controlled diabetes and recurring episodes of DKA are also at a higher risk for underlying psychosocial problems or psychiatric illness.
The ADA recommends screening for symptoms of depression and diabetes distress beginning at ages 7–8 years for children with diabetes (ADA, 2024a). Symptoms of depression in children can include:
- Poor performance in school
- Reluctance to go to school
- Complaints of body pains and hurting not related to injury
- Irritability
- Clinginess
(CDC, 2023)
PARENT AND FAMILY STRESS
Diabetes care requires a round-the-clock, full-time commitment, and a diagnosis of diabetes in a child can be devastating for parents. Reactions may include fear, concern, and guilt. Examples of parents’ questions include:
- “What will happen to our child, and will they be okay?”
- “Is our child’s diagnosis a result of something we did or didn’t do?”
- “How will this affect the other children in our family?”
- “Will we be able to manage our child’s care?”
The healthcare team must address these and other concerns initially and on an ongoing basis (Childs et al., 2017; Theofilou & Vlastos, 2023).
Studies show that parents of children with T1D are at high risk for depression and anxiety. Parents of children with a chronic health condition such as diabetes often focus their energy and attention on the child’s healthcare needs to the detriment of their own well-being, which can lead to caregiver burnout. Caregivers can help parents understand that maintaining their own physical and emotional health is essential for their child’s well-being (Marker, 2021).
Family conflict over management of diabetes is another source of emotional distress for children and parents, which may include a child who is uncooperative with diabetes care. Older children may rebel against treatment and insist on making their own decisions. This can be physically and emotionally exhausting for parents. In these instances, the child and parents are referred to a mental health professional.
The needs of other children in the family must also be addressed, such as the fear that they too will develop diabetes, resentment about the extra time and attention given to the child with diabetes, protectiveness of their sibling with diabetes, and a desire to be involved in the care of the child with diabetes. As far as possible, all children in the family are included in diabetes education and a family treatment plan (Childs et al., 2017).
(See also “Issues Facing Adolescents with Diabetes” and “Transition to Adult Care” later in this course.)
CASE
Demetrius is 8 years old and was diagnosed with T1D when he was 4. He lives with his mother, Margot, who is a single parent, and his 9-year-old sister. Margot was devastated when he was diagnosed but was determined to learn how to manage her son’s care.
At his scheduled appointment today, Demetrius is quiet and clearly unhappy, and his mother looks anxious and exhausted. The clinician notices that Margot snaps several times at her son. Based on their trusting relationship, the clinician asks Margot if she may speak with Demetrius alone. His mother agrees, and once she leaves the room, the clinician asks the boy if he has anything he wants to tell her. “I want to play soccer, but my mom won’t let me. I hate this stupid diabetes!” he responds.
The clinician then asks Demetrius to wait in the playroom while she speaks with his mother: “Are you having a difficult time at the moment? What can I do to help?” Margot bursts into tears, sobbing, “Demetrius wants to play soccer, but no matter how often I tell him it’s too dangerous, he won’t listen.”
The clinician discusses with Demetrius and Margot the positive benefits of exercise and that participating in team sports is possible for children with diabetes. Also acknowledging Margot’s fears and hesitation, they prepare a list of her questions and concerns so that Margot can meet with the soccer coach and discuss the possibility of Demetrius joining the team.
When they meet a few days later, the coach tells Margot that he has had several children with diabetes on his teams over the years and that he understands her fears. Although she is still concerned about the risk of hypoglycemia, Margot agrees to let Demetrius start soccer practice twice a week. She and the coach review all the pertinent details of her son’s condition and management plan. Demetrius is overjoyed and excitedly tells his mother, “I’m going to be like all the other kids!”
Developing Patient Independence in Diabetes Self-Management
As children get older, it is important that they learn to actively participate in their own diabetes care and that the parents’ role evolves from that of caretaker to coach (Childs et al., 2017). This can be a challenging time, and some parents can become overprotective, leading to a strained relationship with the child or the entire family (Marker et al., 2021).
How quickly a child will become independent in most or all of their diabetes self-management differs from child to child. Transfer of care to the child is best achieved in small, manageable steps, with the clinician closely monitoring and assessing the child’s readiness to learn new skills and their proficiency in performing each skill, such as drawing up and administering their own insulin (Childs et al., 2017).
Advice for parents and families includes:
- Maintain open communication, allow the child to express their concerns, and avoid telling the child how they should feel.
- Ensure that the child knows they can reach out to their parents regardless of any problem, whether at home or at school, without fear of the parent’s anger or censure.
- Nurture the child’s self-confidence while providing them with emotional and practical support.
- Strive for balance between taking care of the child and allowing them to take care of themselves. For example, when traveling, parents can carry a backup blood-testing kit and insulin supplies in case the child forgets to bring them.
- Listen to the child’s needs and make adjustments where possible while maintaining the rules that are in place to keep the child safe.
- Continue to advocate for their child, while teaching the child the skills and knowledge needed to advocate for themselves.
- Continue to do fun things with the child on a regular basis, individually and as a family.
- Do not allow the responsibility of managing diabetes to become the dominant force in the child’s life; make time for hobbies, laughter, and a balanced life.
Addressing Medical Neglect
A clinician may encounter a child in which parental involvement is less than optimal for diabetes care. Type 1 diabetes is one of the most common conditions related to medical neglect of children reported to Child Protective Services. One “red flag” is recurrent admissions for DKA together with the claim that the child has been sneaking food as the cause. Such an explanation points to the possibility of medical neglect or, at the minimum, substandard attention to or poor understanding of diabetes management. It is critical for clinicians to understand the high risk of poor outcomes for children with diabetes who are victims of medical neglect (Fox et al., 2020).
Clinicians must learn to identify children at risk for medical neglect. A social history during the initial assessment and inquiring about any new problems during follow-up visits are crucial in getting to know families and their circumstances. Interventions that can be put in place to help families include contact with social and community services and more frequent clinical visits with the child and family.
The reasons for medical neglect can be complex. Obstacles to ensuring adequate care may include difficulty obtaining insurance, lack of transportation, lack of a caretaker for other children in the family, financial problems, difficulty understanding the complexity of care, difficulty managing care, and lack of caretaker motivation.. Parents may also face issues with psychiatric illness, substance abuse, and domestic violence (Riviello & Rozzi, 2023; Levitt & Altman, 2023).
Leaving a child with diabetes in the care of a person who has not received diabetes education or who is not provided with the supplies and medications to care for the child is considered medical neglect. The diabetes management team must emphasize to the parents that it is the parent’s responsibility to ensure that everyone who provides care for the child is educated in diabetes management. Clinicians supply education materials that parents can use to train babysitters and other caretakers in providing safe care. They can also role-play teaching sessions between parents and other caretakers.
ISSUES FACING ADOLESCENTS WITH DIABETES
During adolescence, issues can arise related to independence, the hormonal and maturational changes that occur at puberty, and peer relationships. Worries about the perception of friends can lead to diminished adherence to diabetes management, resulting in erratic metabolic control and diabetic complications (Davis, 2020). Young adults may also come to realize what a chronic, lifelong condition means, and these patients are at high risk for diabetes burnout and depression.
Clinicians can support parents in meeting the challenges of relinquishing responsibility for care to their adolescent child and evolving into the role of “coach” (Childs et al., 2017). Adolescents can be educated in ways to “vent” their anger and frustration and assisted in developing a plan to better manage their condition.
Being Diagnosed with Diabetes during Adolescence
The reaction to a diabetes diagnosis is highly individualized. A 15-year-old who was first diagnosed with diabetes as a 4-year-old will likely have a much different mindset about the condition than a 14-year-old who was diagnosed three months ago. The former may think that “diabetes is a bummer,” but they are accustomed to it as part of their day-to-day existence.
The newly diagnosed adolescent may experience an acute sense of loss as their independence becomes restricted. Research has shown that such a diagnosis can produce emotions akin to grief, negatively impact the individual’s self-concept, and evoke a significant feeling of being different from one’s peers. The strong desire for acceptance can cause adolescents with diabetes to deny their condition, neglect diabetes management, and skip insulin injections. The consequences of this behavior can be serious, such as recurring hospital admissions with diabetic ketoacidosis (Davis, 2020).
An important goal of care is to help such an adolescent accept a new normal in their lives and develop the belief that it is possible for them to manage diabetes. Parental participation and support of family and friends are a primary source of positive adjustment to diabetes among adolescents (Yamaguchi et al., 2023). Conversely, a lack of or limited parental involvement correlates with poorly controlled diabetes. Participation in support groups for young adults with diabetes is also linked to positive outcomes.
Sensitivity, caring, and a patient-centered approach by the healthcare team are key factors in how well a young adult begins to process what is happening. Adolescents with diabetes have reported a positive impact of having choices in setting treatment goals and of regular appointments with the same members of the diabetes healthcare team (ADA, 2024a).
Puberty and Diabetes
The physiologic changes of puberty may be impacted by diabetes. Uncontrolled diabetes can delay the onset of puberty. During puberty, insulin resistance will increase, and more frequent blood glucose checks are required. This can be a further source of frustration for the adolescent and a source of worry for the parents (Childs et al., 2017).
Girls with diabetes have a higher prevalence of weight gain during puberty than their peers who do not have diabetes. They are also at a higher risk for polycystic ovary disease (Adone & Fulmali, 2023; Ciona, 2022). Patient and parent education includes a discussion of how blood glucose levels may increase in the days preceding menses and decrease in the days immediately after menses. This requires more frequent blood glucose checks, adjustments in insulin dosage, and possible changes to the meal plan. Hormone fluctuations in the early stages of puberty can also make it more difficult for adolescent girls to maintain optimum glucose control (CDEC, 2024).
For adolescent boys, blood glucose control is more difficult in the later stages of puberty. One fourth of adolescent males with T1D have diminished levels of testosterone. Poorly controlled diabetes can also result in lower-than-normal weight, height, and BMI in young males (Dansinger, 2023).
Sexual Counseling
Sexual activity, contraception, and pregnancy should be discussed openly and nonjudgmentally, assuring the young person that their privacy will be respected. Since this is a conversation that most young people will not initiate, the clinician includes these topics as part of the overall education plan for the patient. It may also be an opportune time for a clinician to introduce to parents the need for private conversations between their adolescent child and healthcare providers without parents being present.
Similar to all other physical activities, sexual activities can impact a patient with diabetes. Lower blood glucose levels may occur during and following, and so preventing hypoglycemia associated with sex is part of an adolescent’s self-management plan (ADA, 2024a).
PRECONCEPTION COUNSELING
Many young people may have concerns that diabetes will prevent them from having a normal pregnancy and a healthy baby. The clinician can also assure young adults that once they are ready to have a baby, a healthy pregnancy is possible and that the key to this is preconception counseling (UPMC, 2021).
The consistent and correct use of contraception in the prevention of unwanted pregnancies must be reinforced with adolescents who have diabetes. Recommendations for contraceptives include the use of long-acting reversible contraception (LARC) such as intrauterine devices and subdermal hormonal implants. However, studies find that healthcare providers infrequently provide counseling on LARC use (Disney et al., 2020).
Preconception counseling begins as soon as a youth starts menstruation and continues as an ongoing conversation at every visit with the diabetes management team. Girls with diabetes are educated that pregnancy during their teen years can result in serious health problems related to their age and to diabetes. Preconception counseling focuses on ensuring the patient has attained optimal glycemic control and overall good health prior to becoming pregnant in order to decrease the risk of adverse outcomes for the mother and baby. Blood glucose levels that are not well controlled can put the expectant mother at risk for several complications, including preeclampsia (Disney et al., 2020).
Driving with Diabetes
Driving with low blood sugar increases the possibility of a motor vehicle crash, and so responsible behavior for an adolescent with diabetes includes ensuring that their blood glucose level is within a set target range prior to driving. While having diabetes does not preclude an adolescent from obtaining a driver’s license, under the law all drivers can be held accountable for keeping their blood glucose at safe levels (Childs et al., 2017; ADA, 2024a; UCSF, 2024b).
Driving education for an adolescent with diabetes includes the following:
- Check blood sugar levels prior to driving, every time.
- Treat a low blood glucose level even if it means being late to one’s destination.
- Do not start driving until blood glucose is within the target range. (It is okay to call a friend for a ride or to tell others that one is going to be late.)
- Keep a supply of nonperishable snacks and fast-acting sugars in the vehicle or carry some along if traveling in a friend’s vehicle.
- Never leave insulin and test strips in the vehicle; hot and cold temperatures damage them.
- If beginning to feel unwell or noticing that blood sugar is dropping, pull over immediately. Do not tell yourself, “I’m nearly there; I can make it.”
- Once pulled over, check blood glucose, treat a low level, wait 15 minutes, and then recheck.
- Never leave home without a medical alert ID bracelet or necklace.
(Childs et al., 2017; ADA, 2020a)
Alcohol, Smoking, and Recreational Drug Use
A conversation about alcohol, smoking, and drug use must begin during adolescence. Using alcohol and drugs can have an instantaneous effect on blood glucose levels. These substances can also adversely impact an individual’s awareness of and capacity to treat a low blood glucose level.
ALCOHOL AND DIABETES
Knowledge that drinking alcohol can be dangerous to those with diabetes may not prevent an adolescent from this activity, particularly in the presence of peers who are drinking. It takes the liver between one to one-and-a-half hours to process a single drink, and during this time those with diabetes are most at risk for developing low blood glucose levels. Consuming two alcoholic drinks prolongs the risk of hypoglycemia for two to three hours, and the more alcoholic drinks consumed, the greater the amount of time one is at risk for hypoglycemia (UCSF, 2024a).
Actions to keep safe when drinking include:
- Eat before taking the first drink and eat carbohydrate snacks such as chips while drinking.
- Remain in the company of a reliable friend who is aware of one’s diabetes and who knows how to treat hypoglycemia if it occurs.
- Between alcoholic drinks, consume water or a sugar-free drink to prevent dehydration.
- Test blood sugar at least every hour, or have a friend test it. If the blood sugar level drops and one starts vomiting and cannot keep anything down, have someone call 911. Ensure that there is at least one friend with you who knows what to do in these circumstances because it is an emergency.
- After an evening of drinking, eat a meal that contains both fat and protein. Since alcohol remains in the body for a period of time after one stops drinking, it is possible that hypoglycemia can occur while sleeping.
- Since the symptoms of hypoglycemia mimic those of being drunk, always wear a diabetes ID necklace or bracelet so that, in the event of a hypoglycemic episode, others will not presume the individual is merely drunk.
(Mount Sinai, 2024)
SMOKING AND DIABETES
Smoking rates are considerably higher among youth with diabetes than among their peers without diabetes. Diabetes education regarding smoking includes the fact that nicotine damages small blood vessels and can result in kidney and nerve disease. Smoking also heightens the risk for albuminuria. Advising against cigarette smoking also includes advising against the use of e-cigarettes (ADA, 2024a).
RECREATIONAL DRUGS AND DIABETES
Substance abuse and nonprescription drug use can lead to impaired judgment, irregular diabetes management, infrequent blood glucose checks, and erratic insulin administration. This puts the adolescent at risk for short- and long-term complications. Adolescents with diabetes are taught that this is a dangerous and possibly lethal practice.
Different types of illicit drugs can affect people with diabetes in the following ways:
- Marijuana is the most commonly used illicit substance among those 12 years and older in the United States (SAMHSA, 2023). Negative effects of marijuana on cognitive and physical function on individuals with diabetes may include:
- Short-term memory problems, which can lead the individual to forget to take insulin or diabetes medications
- Impaired hand-eye coordination, which can lead to incorrect administration of insulin or diabetes medications
- Symptoms of depression with regular use
- Severe damage to the kidneys and heart when combined with alcohol However, recent studies have also shown that medical marijuana may help with diabetes control. This is an area of ongoing research, and patients and their families are advised to consult with their healthcare provider (Braun, 2023).
- Serious side effects of ecstasy use include kidney damage leading to kidney failure and an irregular heartbeat, which can prove fatal.
- Cocaine can cause hypertension and a subsequent heightened risk for strokes and heart attacks. Those who use cocaine on a regular basis are predisposed to eating fewer balanced meals and an increase in the intake of fatty foods, which can be damaging to those with diabetes.
- Methamphetamines interfere with the activity of insulin and hormone production, causing the release of excessive glucose and subsequent high blood glucose levels.
Since some adolescents will experiment with illicit drugs, those with diabetes must be educated about their safer use and the dangerous outcomes that can result. Important points to emphasize include:
- Check blood glucose levels every 2–3 hours.
- Check for ketones if the blood glucose level is >300 mg/dL.
- Implement a sick-day plan when needed.
- Work with the healthcare team to eliminate problematic drug use.
- Only take an illicit or new drug in the presence of someone else who knows what the drug is and who knows about one’s diabetes; this will help ensure that necessary care will be sought if serious complications occur.
- Do not stop taking insulin or other diabetes medications, since this can lead to high blood glucose levels and organ damage.
- Have readily available sources of quick-acting carbohydrates in case symptoms of hypoglycemia develop after taking an illicit drug.
- Avoid mixing illicit drugs or combining them with alcohol, since this can be a deadly combination.
- Always wear a diabetes identification bracelet.
- Develop friendships in which peer pressure to engage in high-risk activities is not present.
(Vieira, 2020; NDSS, 2020)
Privacy and Diabetes Diagnosis
Frequently, parents want everyone, or nearly everyone, their child is friends with to know about their condition. The clinician explains to parents that it is up to their adolescent child to decide when and whom to tell about their condition. Regardless of whom an adolescent decides to tell about their diagnosis, it is important that they wear a medical alert bracelet at all times and to think ahead about how to manage an out-of-range blood glucose level.
Confiding in close friends usually is not a problem, but sharing one’s diagnosis with others, such as when starting to date someone, may not be so easy. The clinician may be asked, “How do I tell someone new that I have diabetes?” Advice should be simple and use language that is most comfortable for the adolescent. It is usually wiser to tell a new partner about diabetes early on in the relationship, since a caring person will be supportive and someone who does not want to be in a relationship with a person with diabetes is probably someone the youth may rather not be around in the end.
The clinician can also discuss the potential awkwardness shown by a new or existing partner, who may be concerned about saying something that sounds foolish or ignorant. The youth with diabetes should not take silence as a lack of caring; they can instead talk to others about what they experience living with diabetes, what it feels like to have a hypo- or hyperglycemic episode, and what a partner can do to help in these situations (Almekinder, 2020).
Diabetes and Disordered Eating Behaviors
The constant emphasis on regulating food intake in diabetes management closely links those with diabetes to disordered eating behaviors. Current data indicate a pervasive occurrence of nutrition-associated disorders in those with type 1 diabetes compared to peers who do not have diabetes. Bulimia is the most common eating disorder in women with type 1 diabetes, and binge eating is more common among women with type 2 diabetes (ADA, 2024b; Dziewa, 2023).
Diabulimia is form of bulimia in which insulin use is intentionally restricted to lose weight. It is estimated that 30%–40% of young females with T1D reduce insulin therapy to lose weight, with the highest incidence of this behavior in those between the ages of 15–30 years. Adverse side effects associated with diabulimia include:
- Dehydration
- Loss of lean body mass
- In severe cases, development of DKA
(ADA, 2024b)
Warning signs of eating disorders may include:
- Unexplained increase in A1C levels
- Repeated episodes of diabetic ketoacidosis
- Extreme concerns of body size or shape
- Excessive exercise and related hypoglycemia
- Very low-calorie meals
- An absence of menstruation
(ADA, 2024b)
Adolescents may have a hard time acknowledging problems with eating to a clinician, including whether they are skipping insulin doses. Clinicians must maintain a nonjudgmental, supportive attitude. Patients with an eating disorder will most likely be referred to a mental health professional with experience in eating disorders (NEDA, 2023).
TRANSITION TO ADULT CARE
Pediatric clinicians can help prepare an adolescent and their family for differences they may encounter when they transition to adult care providers, such as a faster pace and less interaction time in adult services. Likewise, clinicians working in adult diabetes management must be aware that young people transitioning from pediatric services may require greater attention to integrate successfully into the practice.
The shift from pediatric to adult healthcare presents a high risk for loss of cohesion in the delivery of services and is a period when many young people no longer receive adequate healthcare. Others may never take ownership of their diabetes management and remain over-reliant on their parents. This transition phase is linked with worsening glycemic stability, higher rates of acute complications, and the beginning of chronic complications associated with poor diabetes control (ADA, 2024a).
Adolescents are advised to attend medical appointments alone during at least the last six to nine months of their pediatric care. This fosters independence and allows the young person to practice describing their symptoms, answering provider questions, posing their own questions, and planning implementation steps. Initially, parents may not react well to this suggestion, in which case the clinician can provide parents with a summary at the end of the appointment (Ispriantari et al., 2023).
Moving Away from Home
Young people moving away from their family home or leaving to attend college may introduce various issues related to diabetes care. These include:
- Locating new providers who have experience in managing diabetes
- Addressing insurance and financial considerations for healthcare coverage (the Affordable Care Act allows for continued coverage under parents’ healthcare policies until the age of 26 years)
- Adapting to new college or work schedules, making new friends, and socializing, which can all push diabetes care into the background for the young adult
- Lack of parental supervision and support from childhood friends
The diabetes care team works to ensure that diabetes self-management remains a top priority in the patient’s life. This includes reviewing strategies for possible problem scenarios that may occur when living independently or with a new roommate, such as:
- How will you manage low blood sugar during the night?
- What will you do if you run out of insulin late at night?
- Who will be your point of contact for emergencies?
- What will you do if checking your blood sugar and administering insulin conflicts with class time or work shifts?
- What approaches will you use to deal with stress, such as exams?
- What action will you take if you find a cut or sore on your foot that is not healing?
- What will you do if you do not like your new healthcare provider?
If attending college, the student can inquire about care and support groups offered by the college to students with diabetes. College health officials and at least a small group of new acquaintances should be informed about the student’s diabetes, including roommates, dormitory supervisors, and other appropriate college staff members (Hagger et al., 2023).
(See also “Resources” at the end of this course.)
CASE
Kayla is 17 years old and was first diagnosed with type 1 diabetes when she was 6. She’s now a senior in high school and plans to go to college in a few months. During a routine visit, the clinician pays special attention to the pattern of behavior that has typified Kayla’s visits and diabetes management.
Kayla is polite, enjoys talking about school and sports, and keeps her blood glucose readings up to date on her smart phone. She has been independent in administrating insulin since her early teens. However, her parents take responsibility for all other aspects of diabetes management, such as meal preparation, calorie counting, sick-day management, and collecting insulin prescriptions from the pharmacy. When the clinician asks what preparations Kalya and her parents have made for managing her diabetes at college, Kayla looks to her parents, who respond, “We haven’t thought about it yet.”
Although Kayla is independent in checking her blood glucose and administrating insulin, she has not yet taken ownership of full management of her diabetes. Therefore, the clinician makes several recommendations to help Kayla live safely away from home:
- That Kayla start attending appointments for diabetes care on her own. While her parents may be apprehensive about this, it will allow Kayla to develop self-advocacy skills and will allow her to discuss issues that she may not raise in front of her parents.
- That Kayla attend a consultation with the dietitian to review mechanisms for calorie counting and how that can be best accomplished living in a dorm and when selecting a college meal plan.
- That Kayla visit The Diabetes Link website for young adults and list at least three recommendations from their website that she will follow up on.
The clinician also provides Kayla’s parents with time to talk about their fears and concerns and helps them put together a plan that includes the following steps:
- Check with their healthcare carrier to ensure their present policy will continue to cover Kayla when she moves away from home.
- Meet with the social worker to identify providers close to Kayla’s college who have experience working with college students with diabetes.
- Set up a meeting with the college healthcare center for themselves and Kayla in order to learn about available services and programs, such as a diabetes support group for students.
- Help Kayla put together an emergency contact list she can call on once she moves to college.
- Put together sick-day supplies Kayla can keep in her dorm room.
The clinician ends by explaining that preparation for transitioning to college is not a one-time event; it is a process that takes several months to successfully complete.
CONCLUSION
The number of children and youth with diabetes is increasing. Providing care to young patients with diabetes can be a unique and challenging experience in all settings. Clinicians must take into consideration the child’s developmental stage in order to create a holistic approach to diabetes care. In many instances, a clinician will work with pediatric patients with diabetes over the course of several years and build up a close, therapeutic relationship with these children and their families. In this way, the clinician advocates for the patient’s needs and offers support and encouragement to them and their caregivers from childhood through adolescence and as they transition to independent self-management.
RESOURCES
Access and affordability resources (Association of Diabetes Care and Education Specialists)
Childcare, camps, and recreational programs (ADA)
Diabetes (CDC)
The Diabetes Link (support for teens/young adults)
Financial help for diabetes care (NIDDK)
Support groups for children and young adults (Diabetes Foundation)
REFERENCES
NOTE: Complete URLs for references retrieved from online sources are provided in the PDF of this course.
Abraham MB, Karges B, Dovc K, Naranjo D, Arbelaez AM, Mbogo J, Javelikar G, Jones TW, & Mahmud FH. (2022). ISPAD clinical practice consensus guidelines 2022: Assessment and management of hypoglycemia in children and adolescents with diabetes. Pediatr Diabetes, 23(8), 1322–40. https://www.ncbi.nlm.nih.gov
Adone A & Fulmali DG. (2023). Polycystic ovarian syndrome in adolescents. Cureus, 15(1), e34183. https://doi.org/10.7759/cureus.34183
Almekinder E. (2020). Should I tell others about my diabetes, or keep it a secret? The Diabetes Council. https://www.thediabetescouncil.com
American Academy of Pediatrics (AAP). (2020). Diabetes in children. https://www.healthychildren.org
American Diabetes Association (ADA), Professional Practice Committee. (2024a). Introduction and methodology: Standards of care in diabetes—2024. Diabetes Care, 47(Suppl 1), S1–S4. https://doi.org/10.2337/dc24-SINT
American Diabetes Association (ADA). (2024b). Types of eating disorders. https://www.diabetes.org
American Diabetes Association (ADA). (2024c). Fact sheet: The rights of children with diabetes in camp. https://diabetes.org
American Diabetes Association (ADA). (2023a). 2023 camp overview. https://diabetes.org
American Diabetes Association (ADA). (2023b). Understanding type 1 diabetes. https://diabetes.org
American Diabetes Association (ADA). (2023c). Exercise & type 1. https://diabetes.org
Braun A. (2023). Marijuana and diabetes: Benefits and precautions. Verywellhealth. https://www.verywellhealth.com
Better Health Channel. (2021). Diabetes—Issues for children and teenagers. https://www.betterhealth.vic.gov
Bloomgarden Z & Rapaport R. (2023). Diabetes trends in youth. https://www.ncbi.nlm.nih.gov
Center for Diabetes and Endocrine Care (CDEC). (2024). What do I need to know about type 1 diabetes, puberty, and my teenager? https://diabetesendocare.com
Centers for Disease Control and Prevention (CDC). (2023). Anxiety and depression in children. https://www.cdc.gov
Children with Diabetes. (2024). Glucagon for severe hypoglycemia. https://childrenwithdiabetes.com
Children’s Health. (2024). Pediatric type 1 diabetes sick-day guidelines. https://www.childrens.com
Children’s Health Care of Atlanta. (2022). Spotting the signs of type 1 diabetes. https://www.choa.org
Childs BP, Cypress M, & Spollett GR (Eds.). (2017). Complete nurses’ guide to diabetes care: Children with diabetes (3rd ed.). American Diabetes Association. https://doi.org/10.2337/9781580405690
Cleveland Clinic. (2024). Sick day management for children with type 1 diabetes. https://my.clevelandclinic.org
Cleveland Clinic. (2023). GLP-1 agonists. https://my.clevelandclinic.org
Dansinger M. (2023). Puberty and type 1 diabetes. WebMD. https://www.webmd.com
Davis EA, Shetty VB, Teo SYM, Lim RJ, Patton SR, & Taplin CE. (2023). Physical activity management for youth with type 1 diabetes: Supporting active and inactive children. Diabetes Spectr, 36(2), 137–45. https://doi.org/10.2337/dsi22-0020
Davis L. (2020). “Problems with adherence and social stigma in adolescents with type 1 diabetes.” Master’s Theses. 232. https://digitalcommons.bucknell.edu
Dartmouth Health Children’s. (2024). Managing sick days. https://childrens.dartmouth-health.org
Diabetes Care Community. (2021). Hypoglycemia symptoms. https://www.diabetescarecommunity.ca
Disney EA, Sanders JN, Turok DK, & Gawron LM. (2020). Preconception counseling, contraceptive counseling, and long-acting reversible contraception use in women with type 1 diabetes: A retrospective cohort study. Women's Health Reports, 1(1), 334–40. https://www.liebertpub.com
Drugs.com. (2024). Empagliflozin. https://www.drugs.com
Dziewa M, Bańka B, Herbet M, & Piątkowska-Chmiel I. (2023). Eating disorders and diabetes: Facing the dual challenge. Nutrients, 15(18), 3955. https://www.mdpi.com
El-Mohandes N, Yee G, Bhutta BS, & Huecker MR. (2023). Pediatric diabetic ketoacidosis. StatPearls Publishing. https://www.ncbi.nlm.nih.gov
Fallabel C. (2023). Type 1 diabetes in children: The warning signs, symptoms and treatments. Healthline. https://www.healthline.com
Faradji RN, Uribe-Wiechers AC, & de la Maza ES. (2023). Hypoglycemia: Diagnosis, management, and prevention. In J Rodriguez-Saldana (Ed.), The diabetes textbook. Springer. https://doi.org/10.1007/978-3-031-25519-9_45
Fox LA, Pfeffer E, Stockman J, et al. (2020). Medical neglect in children and adolescents with diabetes mellitus. Journal of Child & Adolescent Trauma, 13(3), 259–69. https://www.ncbi.nlm.nih.gov
Hagger V, Lake AJ, Singh T, Hamblin PS, & Rasmussen B. (2023). The experience and support needs of students with diabetes at university: An integrative literature review. Diabetic Medicine: A Journal of the British Diabetic Association, 40(1), e14943. https://doi.org/10.1111/dme.14943
Ispriantari A, Agustina R, Diema Konlan K, & Lee H. (2023) Family-centered interventions for children and adolescents with type 1 diabetes mellitus: An integrative review. Child Health Nurse Res, (29)1, 7–23. https://www.ncbi.nlm.nih.gov
Kenowitz J. (2022). Helping your child adjust to diabetes. Kids Health. https://kidshealth.org
Levitt L & Altman D. (2023). Complexity in the U.S. health care system is the enemy of access and affordability. JAMA Health Forum, 4(10), e234430. https://jamanetwork.com
Lin R, Brown F, James S, et al. (2021). Continuous glucose monitoring: A review of the evidence in type 1 and type 2 diabetes mellitus. Diabet Med, 38(5), e14528. https://pubmed.ncbi.nlm.nih.gov
Los E & Wilt AS. (2023). Type 1 diabetes in children. StatPearls Publishing. https://www.ncbi.nlm.nih.gov
March C, Sherman J, Bannuru RR, Fischer A, Gabbay RA, Rodriguez H, Rodriguez J, et al. (2023). Care of young children with diabetes in the childcare and community setting: A statement of the American Diabetes Association. Diabetes Care, 46(12), 2102–11. https://doi.org/10.2337/dci23-0083
Marker AM, Monzon AD, Goggin K, Clements MA, & Patton SR. (2021). Parent perspectives on educational and psychological intervention for recent-onset diabetes in their school-age child: A qualitative study. Diabetes Spectr, 34(2), 166–74. https://doi.org/10.2337/ds20-0058
Mayo Clinic. (2023a). Type 1 diabetes in children. https://www.mayoclinic.org
Mayo Clinic. (2023b). Type 2 diabetes in children. https://www.mayoclinic.org
Medline Plus. (2024). Empaglifozin. https://medlineplus.gov
Mount Sinai. (2024). Diabetes and alcohol. https://www.mountsinai.org
National Diabetes Services Scheme (NDSS). (2020). Drug use and type 1 diabetes booklet. https://www.ndss.com
National Eating Disorders Association (NEDA). (2023). Eating disorders and diabetes. https://www.nationaleatingdisorders.org
National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). (2020). Helping the student with diabetes succeed. National Institutes of Health. https://www.niddk.nih.gov
National Institutes of Health (NIH). (2021). Diabetes type 2—meal planning. Medline Plus. https://medlineplus.gov
Nationwide Children’s Hospital (NCH). (2024). Glucagon and mini-dose glucagon. https://www.nationwidechildrens.org
Nye J. (2024). Nocturnal hypoglycemia linked to high-activity days among children with T1D. Endocrinology Advisor. https://www.endocrinologyadvisor.com
Pinhas-Hamiel O & Zeitler P. (2023). Type 2 diabetes in children and adolescents: A focus on diagnosis and treatment. In KR Feingold, B Anawalt, MR Blackman, et al. (Eds.), Endotext [Internet], MDText.com. https://www.ncbi.nlm.nih.gov
Polo KM & Cahill SM. (2017). Interprofessional collaboration to support children with diabetes. Open Journal of Occupational Therapy, 5(3), article 3.
Riviello RJ & Rozzi HV. (2023). How to identify and work with neglected children in the ED. ACEPNow. https://www.acepnow.com
Rocky Mountain Diabetes Center. (2024). Pediatric—Low blood sugar. https://rockymountaindiabetes.com
Rubelj K, Stipančić G, La Grasta Sabolić L, & Požžgaj ŠŠepec M. (2021). Continuous glucose monitoring and type 1 diabetes mellitus control in child, adolescent and young adult population–Arguments for its use and effects. Acta Clin Croat, 60(4), 609–16. https://www.ncbi.nlm.nih.gov
Substance Abuse and Mental Health Services Administration (SAMHSA). (2023). 2022 National Survey on Drug Use and Health (NSDUH) releases. https://www.samhsa.gov
Sun J, Wang C, Zhao M., et al. (2022). Childhood diabetes mellitus and early-onset kidney diseases later in life: A nationwide population-based matched cohort study. BMC Med, 20, 428. https://doi.org/10.1186/s12916-022-02634-4
Tamborlane WV. (2021). Diabetes in children and adolescents. Humana Press, Springer Nature Switzerland AG.
Theofilou P & Vlastos DD. (2023). The psychological burden of families with diabetic children: A literature review focusing on quality of life and stress. Children (Basel), 10(6), 937. https://www.ncbi.nlm.nih.gov
UC Davis Health. (2024). Pediatric diabetes: Type 1 diabetes: Nutrition and exercise. https://health.ucdavis.edu
University of California, San Francisco (UCSF). (2024a). Diabetes and alcohol. https://dtc.ucsf.edu
University of California, San Francisco (UCSF). (2024b). Diabetes and teen driving. https://www.ucsfbenioffchildrens.org
University of Pittsburg Medical Center (UPMC). (2021). Preconception counseling starts at puberty for child-bearing women: An essential tool in diabetes care. https://www.upmcphysicianresources.com
Vieira K. (2020). Drug and alcohol abuse with diabetes: Risk and effects. American Addiction Centers. https://drugabuse.com
Wang L, Xu R, Kaelber DC, & Berger NA. (2024). Glucagon-like peptide 1 receptor agonists and 13 obesity-associated cancers in patients with type 2 diabetes. JAMA Netw Open, 7(7), e2421305. https://pubmed.ncbi.nlm.nih.gov
Yamaguchi M, Honda J, & Fukui M. (2023). Effects of parental involvement on glycemic control in adolescents with type 1 diabetes mellitus: A scoping review. Journal of Family Nursing, 29(4), 382–94. https://journals.sagepub.com
Zolot J. (2021). Diabetic ketoacidosis in children may lead to cognitive impairment. American Journal of Nursing, 121(4), 17.
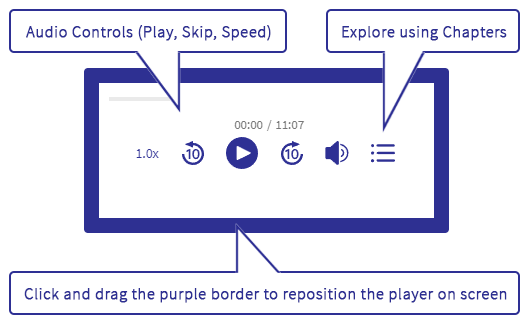





Customer Rating
4.9 / 448 ratings