End-of-Life, Palliative, and Hospice Care
Online Continuing Education Course

Course Description
7-contact-hour end-of-life, palliative care, and hospice care nursing CEU. This palliative care continuing education course includes information on hospice, postmortem care, and bereavement. Guide and support your terminal patient and their family; covers pain management and ethical, legal, and psychosocial issues.
Course Price: $42.00
Contact Hours: 7
Pharmacotherapeutic Hours: 0.25
Course updated on
December 2, 2025
"Excellent program. Every section was interesting to read, with just enough stats to emphasize certain points." - Renee, RN in Indiana
"This is an exceptional program." - Javier, RN in New York
"Effective tables and bullet-point presentations. Flowed well from one subject to the next. Easy to follow." - Mary, RN in Michigan
"As always, great CE with reasonable prices. I will keep coming back to Wild Iris." - Cordell, NP in New York
End-of-Life, Palliative, and Hospice Care
Copyright © 2025 Wild Iris Medical Education, Inc. All Rights Reserved.
LEARNING OUTCOME AND OBJECTIVES: Upon completion of this continuing education course, you will have increased your knowledge of end-of-life care. Specific learning objectives to address potential learning gaps include:
- Discuss the need for end-of-life care in the United States.
- Differentiate between palliative care and hospice care.
- Explain legal and ethical principles in end-of-life care.
- Discuss the essential elements of effective communication with patient and family.
- List pain management interventions for the dying patient.
- Identify the psychosocial and support needs of the patient and family.
- Describe the end-of-life care needs of special populations.
- Explain the care of the patient just prior to and following their death.
TABLE OF CONTENTS
- The Need for End-of-Life Care
- Palliative Care and Hospice
- Legal and Ethical Factors in End-of-Life Care
- Effective Communication with Patients and Families
- Management of Pain and Other Symptoms
- Psychosocial Support Issues
- End-of-Life Care for Special Populations
- Death of the Patient
- The Family’s Bereavement
- Conclusion
- Resources
- References
THE NEED FOR END-OF-LIFE CARE
The Burden of Chronic Illness
Seventy percent of all deaths among Americans are from chronic diseases. Chronic diseases are those that last one or more years, require continuous medical treatment, and limit activities of daily living. In the United States, 60% of adults have a chronic illness, and 40% have more than one chronic illness. The most common chronic diseases include heart disease, cancer, lung disease, diabetes, cardiovascular accident, Alzheimer’s disease, arthritis, and chronic kidney disease. The most common causes for chronic disease include smoking (including secondhand smoke), alcohol consumed in excess, poor nutritional intake, and lack of physical activity.
In health center or clinic visits, the main reason patients 65 or older needed to be seen was due to circulatory disorders. Chronic cardiovascular disease symptom exacerbations were the cause of 34.2% of clinic visits in this age group (Santo et al., 2025).
The vast majority of all healthcare funding ($4.9 trillion) pays for the treatment of chronic medical and mental illnesses (CDC, 2024a). On average, Americans with chronic illness will also need help with routine activities of daily living for two or more of their final years of life.
Increasing Population of Older Adults
The graying of the baby boom generation (born 1946 to 1964) threatens to intensify this burden of chronic illness. The first baby boomers turned 65 in 2011, and the last will turn 65 in 2029. In 2022, 17.3% (57.8 million) of the U.S. population was older than 65, and by 2030 it will be 20% (71.2 million). By 2100 the population of 65-year-olds is expected to increase to 29.1% (106.3 million) (Agingstats.gov, 2024).
Research has also shown that baby boomers are living longer than people roughly 20 years older but that they are not healthier. While they are less likely to smoke or have emphysema, they are more likely to be obese or have diabetes or hypertension than the previous generation due to the link between advanced age and obesity as risk factors for diabetes. They are also more likely to have Alzheimer’s disease or dementia. High cholesterol and heart disease are also more likely due to obesity as a comorbidity. Vision and hearing losses are prevalent (Scripps, 2025).
Healthcare Workforce Shortage
Together, the burdens of chronic illness and cancer point to an exponential escalation in the demand for palliative care over the next several decades. Experts are concerned that there will be too few physicians and nurses certified in palliative care to meet the needs of this aging cohort. Baby boomers also make up a significant part of the healthcare workforce, and when they retire, the existing nursing shortage will worsen. In 2024, a national shortage of 78,610 full-time RNs was projected for 2025 and 63,720 was projected for 2030 (AACN, 2024).
Lack of Knowledge About End-of-Life Care
In general, Americans are reluctant to talk about death or to express their wishes about end-of-life care. Less than one third of Americans express in writing their wishes about how they want to be cared for at the end of life. Fewer still have not thought about end-of-life care at all, while some have thought about it but not told anyone else what they want. Avoiding the subject of death has created woeful ignorance about end-of-life issues, resulting in less than optimum care and diminished quality of life for the dying and their families.
High-quality end-of-life care is important to both patients and families. For some this may mean dying in the hospital, where the patient can be made comfortable and cared for around the clock by specially trained healthcare personnel. For others this may mean the benefits that come from privacy, comfort, quiet, and being surrounded by loved ones. Often, however, the family members who are in a position to make end-of-life decisions may not be aware of the preferences of their dying loved one if there is no formal advance directive in place.
Among Medicare patients in hospice, their location when dying varies greatly. In 2023, by far the largest group were those dying at home (51%), followed by those dying in an assisted living facility (24%), long-term nursing facility (14.7%), skilled nursing facility (5%), inpatient hospice facility (2.4%), and inpatient hospital (1.4%) (Statista, 2025).
Dying in hospitals not only increases the cost of care but often subjects patients to uncomfortable and unnecessary procedures. For example, increasing numbers of older patients are being admitted to intensive care units (ICUs), where they require ventilator assistance, tracheostomies, aggressive treatment for sepsis, suctioning, catheterization, more frequent monitoring and interventions, and an upsurge in diagnostic tests.
PALLIATIVE CARE AND HOSPICE
Both palliative care and hospice in the United States originally focused on the care of cancer patients, but now both encompass care of patients with other severe illnesses such as kidney disease or heart disease. Palliative care and hospice care are not the same (Vossel, 2025). (See also “Palliative Care vs. Hospice Care” below).
What Is Palliative Care?
Palliative care is a recognized subspecialty by the American Board of Medical Specialties. The word palliative comes from the Latin word palliare, which means “to cloak” or “to disguise.” The purpose of palliative care is to reduce the symptoms of a medical condition in order to provide the patient with comfort (Merriam-Webster Dictionary, 2025).
Palliative care is not limited to end-of-life care. As people are living longer with formerly fatal illnesses, palliative care may be used to give patients comfort in conjunction with more aggressive, lifesaving measures. It includes:
- Relieving symptoms that negatively affect a patient’s quality of life, such as pain, anxiety, dyspnea, confusion, hunger, thirst, nausea and vomiting, diarrhea, agitation, and sleep disturbances
- Alternative nursing comfort measures that do not require a physician’s order, such as massage, repositioning, heat, cold, a peaceful environment, distraction, guided imagery, and good hygiene
In patients with life-limiting illnesses, palliative care can be used to provide comfort, reduce hospital stays, and reduce the use of healthcare resources. Palliative care is provided in a number of settings such as physician practices, hospitals, cancer centers, dialysis units, homes, hospices, and long-term care facilities. Palliative care workers provide social and spiritual support for both the patient and the family in a team-based approach to care delivery.
Palliative care’s focus on communication in addition to pain and symptom management occurs long before the end of life. Primary care providers explore their patients’ values, cultures, and goals in deciding how aggressive to be in treating diseases such as cancer and caring for the patient during treatment (Cleveland Clinic, 2025a).
Palliative care for those with life-limiting illness ideally begins at the time of diagnosis. Unfortunately, however, referrals to palliative care tend to occur late in the trajectory of illness. This may be related to the misperception of palliative care as “giving up.” Some patients, families, and healthcare professionals may believe that trading aggressive treatment of potentially fatal conditions for improved quality of life will shorten survival and decrease the patient’s lifespan. However, studies into the effects of early palliative care show that early introduction of such care leads to improved quality of life and mood and may even extend life as the patient feels better (Cleveland Clinic, 2025a).
Initially, the introduction of palliative care to ICU patients helped to facilitate the patient’s progression to a medical–surgical unit and possibly discharge to home on hospice care. This sort of care has morphed into the use of palliative care for resident ICU patients for comfort measures and family support. The symptoms that are treated by palliative care include targeted analgesia, terminal sedation (to the point of unconsciousness for end-stage patients), management of dyspnea, and determination of do-not-resuscitate (DNR) status or choice of extraordinary measures. The American College of Critical Care Medicine recommends early palliative care to reduce the cost of care and shorten the ICU length of stay (Pan et al., 2022).
An assessment of the patient and family’s needs for palliative care and support is an important part of planning the best care for the end of life.
SUPPORTIVE CARE
As an alternative to the term palliative care, the National Cancer Institute defines supportive care as care given to improve the quality of life of patients with a serious or life-threatening disease. The goal of supportive care is to prevent or treat as early as possible the physical symptoms of the disease; treatment side effects; and psychological, social, and spiritual problems related to the disease or its treatment (NCI, n.d.). Supportive, or palliative, care also includes an assessment of the patient’s goals for care. Deciding when to stop treatment can be difficult and should involve the patient, family, and the healthcare team. However, ending treatment does not mean ending care.
What Is Hospice Care?
Hospice is considered the gold standard for end-of-life care. The central paradigm of hospice is that each person is entitled to a high quality of life using a holistic approach and that families are entitled to the support necessary to allow that to happen.
In part, hospice care provides a delivery system for the palliative care services described above. However, hospice also requires determination from a physician that an individual’s life expectancy is less than six months. (Or if the patient lives beyond six months, they may remain in hospice unless they choose to no longer participate.)
Hospice care is based on an interdisciplinary approach that includes physicians, nurses, spiritual counselors, social workers, home health aides, bereavement counselors, trained volunteers, and speech, physical, and occupational therapists, if needed. The team develops an individualized care plan with family caregivers as shared decision makers to meet each patient’s needs for pain management and symptom control. When the patient is cared for at home, hospice staff is on call 24 hours a day, 7 days a week (AGAPE Hospice NW, 2025).
The services delivered by a hospice multidisciplinary team typically include:
- Managing the patient’s pain and symptoms
- Assisting the patient and family with the emotional, psychosocial, and spiritual aspects of dying
- Providing needed drugs, medical supplies, and equipment
- Instructing the family on how to care for the patient
- Delivering special services like speech and physical therapy when needed
- Making short-term inpatient care available when pain or symptoms become too difficult to treat at home or the caregiver needs respite
- Providing bereavement care and counseling to surviving family and friends
(AGAPE Hospice NW, 2025)
Many people mistakenly think the term hospice refers to a place. Although there are some residential hospice facilities, most hospice care takes place in the patient’s home or the home of a loved one and less frequently in hospitals and nursing homes.
HOSPICE FACTS AND FIGURES
- The number of Medicare-certified hospice programs has grown to approximately 5,200. Hospice care is increasingly available in long-term care facilities and hospitals.
- In 2024, the amount of Medicare dollars spent on hospice was $27.5 billion.
- Hospice care is available in all 50 states, the District of Columbia, Puerto Rico, Guam, and the U.S. Virgin Islands.
- More people are choosing hospice care; in 2024, 1.84 million people in the United States received services from hospice.
- In 2024, the number of patient-days of hospice by location were 145,951,139 in the home, 1,185,893 in the hospital, and 453,303 in respite care (CMS, 2025).
- Military personnel and their dependents are covered for hospice care where there is a terminal condition with an expectation of less than six months to live. All U.S. veterans have hospice benefits through the Veterans Administration (U.S. DVA, 2025).
Despite some encouraging changes, other significant challenges remain. Hospice services are still not as widely used as they could be. Fewer than half of patients eligible for hospice choose that option. In 2024, 235,248 dying patients received hospice care for only five to ten days, which is far less than the 60 days considered necessary for people to gain maximum benefit (CMS, 2025).
Hospice is not just for people with cancer. Hospice recipients in 2024 had the following diagnoses:
- Alzheimer’s, dementia, or Parkinson’s, 21.6%
- Cancers, 22.1%
- Respiratory conditions (e.g., COPD), 9.9%
- Circulatory/heart conditions (e.g., heart failure), 19.2%
- Stroke, 10.7%
- End-stage kidney disease, 2.0%
- Other, 14.5%
(CMS, 2025)
Participating in hospice care allows dying patients more time to spend with family and loved ones rather than focusing on medical care. It is far less expensive than other types of end-of-life care (e.g., aggressive chemotherapy, intensive care), and hospice patients are more often able to die at home (CMS, 2025).
The Medicare hospice benefit, instituted in 1983, guarantees comprehensive, high-quality hospice care at little or no cost to terminally ill Medicare beneficiaries and their families (see also “Medicare Coverage for Hospice Services” below).
PALLIATIVE CARE VS. HOSPICE CARE
The terms palliative care and hospice care are often confused or mistakenly used interchangeably, but they have different meanings. Both palliative and hospice care aim to improve a patient’s quality of life and comfort by preventing and relieving symptoms. However palliative care can be provided at any stage of illness and concurrent with curative treatments, whereas hospice care is provided only at the end of life when curative treatments have been stopped.
For instance, a patient with curable cancer may receive palliative care to address pain, stress, and other symptoms alongside their curative treatments of radiation therapy. And a patient whose end-stage cancer is no longer responding to treatment may receive hospice care once they have received a terminal diagnosis of six months or less and ended all curative treatments for the remaining weeks or months of life.
“Open-Access” Care
Programs called open-access hospice, bridge hospice, concurrent care, or outpatient palliative care offer terminal patients both disease-modifying and comfort-focused hospice care in their home, nursing home, or assisted-living facility. Patients may be on hospice and continue to receive curative medical treatments such as IV antibiotics, IV nutrition, IV cardiac medications, ventilators, chest tubes, hemo- or peritoneal-dialysis, palliative radiation, or biological response modifiers such as Epogen, Neupogen, or Procrit. Patients also have access to an interdisciplinary team of experts to address psychosocial and special care needs. The hope is that these new programs will encourage more patients and their families to enter hospice earlier and avoid the costly final weeks of hospitalization that so many Americans experience at the end of life (AccentCare, 2022).
Open-access programs are available to those without the ability to pay and are usually available through larger hospice facilities. Smaller agencies, various visiting nurse associations, or home health agencies may provide a program of palliative care for terminal patients and their families that is not restricted by the expectation of death within six months or the requirement to forego life-prolonging treatments.
The Medicare hospice benefit (MHB) is the main method of payment for hospice care. Since the MHB per diem payment structure does not allow some costly palliative treatments, open-access programs can “bridge” the period between hospitalization and aggressive treatment and hospice care at the end of life. Approximately 29% of hospices have open-access care (CMS, 2025).
HOSPICE CARE AND CURATIVE TREATMENTS
Medicare beneficiaries are required to forgo curative care such as chemotherapy and radiation therapy in order to receive hospice services, although the patient may discontinue hospice services and return to more aggressive treatment at any time. This requirement is one reason some people avoid hospice until the last days or weeks of life and continue with aggressive, expensive treatment, which may make little or no difference in survival time and may diminish the quality of life in the process.
Paying for Hospice Care
Medicare, Medicaid (in most states), the Department of Veterans Affairs, most private insurance plans, HMOs, and other managed care organizations pay for hospice care. Community contributions, memorial donations, and gifts allow many hospices to provide free services to patients who cannot afford payment. Some programs charge patients according to their ability to pay on a sliding scale (ACS, 2025).
According to the Patient Protection and Affordable Care Act of 2010, the majority of patients in hospice care are covered by Medicare. To qualify for the first 180 days of hospice care, the patient’s physician and the hospice medical director (also a physician) must see the patient and certify that the patient has less than six months to live if the disease runs its normal course. A hospice doctor or nurse practitioner must recertify the patient in a face-to-face visit before each benefit period after that. Medicare offers a one-time-only hospice consultation with a hospice medical director or hospice doctor to discuss care options (ACS, 2025).
Hospice agencies receive per diem payments that vary according to the site where services are received and any other insurance coverage the patient may have. The payment varies according to state and county. For example, in 2025 in the San Francisco–Redwood City–South San Francisco area in California, the payment for routine home hospice care was $344.33/day for the first 60 days of care and $271.21/day after that. Continuous home care was $108.39/hour. Payments are used to manage all care related to a patient. The benefits continue, provided that physicians certify that the patient continues to meet the eligibility requirements (after the initial six months). Medicare enforces an aggregate cap for agencies, effectively limiting the total amount they can receive per patient (CGS, 2025).
Hospice services covered by Medicare are listed below. In addition, many private healthcare plans and Medicaid cover hospice services.
MEDICARE COVERAGE FOR HOSPICE SERVICES
Depending on the terminal illness and related conditions, a hospice plan of care might include any or all of these services:
- Aide and homemaker services
- Dietary counseling
- Doctors’ services
- Drugs for pain and symptom management
- Durable medical equipment for pain relief and symptom management
- Inpatient respite care for up to five days
- Medical supplies, like bandages or catheters
- Nursing and medical services
- Occupational therapy services
- Physical therapy services
- Short-term inpatient care for pain and symptom management
- Social services
- Speech-language pathology services
- Spiritual and grief counseling for you and your family
- Any other services Medicare covers to manage pain and other symptoms related to the terminal illness and related conditions, as the hospice team recommends
Medicare will not cover the following once the patient’s hospice benefit starts:
- Treatment intended to cure a terminal illness or related conditions
- Prescription drugs to cure an illness rather than for symptom control or pain relief
- Care from any hospice provider that wasn’t set up by the hospice medical team
- Room and board for hospice care at the patient’s home, nursing home, or hospice inpatient facility (except short-term inpatient or respite care)
- Care as a hospital outpatient (e.g., in an emergency room), hospital inpatient, or ambulance transportation, unless arranged by the hospice team or unrelated to the terminal illness and related conditions
(Medicare, n.d.)
All Medicare-certified hospices are required to employ physicians and nurses with special expertise in pain management and symptom relief. Nonpain symptoms include (but are not limited to) constipation, dyspnea, nausea and vomiting, dry eyes, and dry mouth. Bereavement and spiritual counselors are also available to help the dying and their families explore their needs and preferences as they come to terms with death.
Disparities in Palliative and Hospice Care
Variation in sociodemographic factors, clinical factors, physicians’ beliefs, and the availability of services all contribute to a wide variation in hospice services received by end-of-life patients. Hospice is a less costly means of treatment for terminally ill patients, which may also explain its prevalence as a method of treatment.
GEOGRAPHIC DISPARITIES
Access to palliative care and hospice programs varies from state to state and between rural and urban populations. States with more concentrated population centers have a greater number of clinical settings other than patient’s homes in which hospice care can be provided (Sengupta et al., 2022).
A wide geographic variation exists in the prevalence of Medicare-certified hospice programs in the United States. Medicare patients in rural areas are much less likely than those in metropolitan areas to use hospice care. Discrepancies exist in the provision of palliative care as well (see box below).
|
States were evaluated using publicly available information across five domains:
|
|
| Rating
(5 to 1 stars) |
States |
|---|---|
| (CAPC/NPCRC, 2024) | |
| 4.5 | Massachusetts, Oregon |
| 4.0 | California, Connecticut, Illinois, Maryland, New Jersey, Ohio |
| 3.5 | Alaska, Colorado, Delaware, Kentucky, Maine, Minnesota, New Mexico, New York, Pennsylvania, Vermont, Virginia |
| 3.0 | Florida, Hawaii, Michigan, Montana, Nebraska, New Hampshire, Rhode Island, Washington, Wisconsin |
| 2.5 | Alabama, Arizona, Indiana, Iowa, Kansas, Nevada, North Carolina, North Dakota, Texas, West Virginia |
| 2.0 | District of Columbia, Georgia, Louisiana, Mississippi, South Carolina, South Dakota, Tennessee, Utah |
| 1.5 | Idaho, Missouri, Oklahoma |
| 1.0 | Arkansas, Wyoming |
RACIAL/ETHNIC DISPARITIES
Most patients express a wish to die at home in the event of a terminal illness and not to receive life-prolonging drugs or mechanical ventilation. However, disparities between White and non-White populations exist across the spectrum of healthcare, including end-of-life care.
Black families have been found to be less likely than White families to receive information about what to expect during end-of-life care. Black patients are also 17% less likely to receive palliative care and more likely than White patients to be admitted to the emergency department, to be admitted to the hospital, and to prefer spending their last days in the hospital (Shryer, 2024).
Racial and ethnic minority patients are less likely than White patients to request hospice services prior to death. Both African Americans and Asian/Pacific Islanders are underrepresented and are less likely to die at home or under hospice care (Rhodes et al., 2022).
A cohort study of 2,407 of Connecticut’s Medicaid program patients and those with dual Medicare/Medicaid eligibility who died between 2017 and 2020 found the percentage of decedents using hospice by race to be non-Hispanic White (53.3%), Hispanic (18.5%), Black (16.2%), and Asian American (3.8%). White patients are also much more likely than African American patients to have admissions to hospice in counties with more physician specialists and more hospital beds (Robison et al., 2023; Rhodes et al., 2022).
Other disparities in end-of-life care include lack of adequate pain care and poor management of pain by healthcare practitioners (Rhodes et al., 2022). Hispanic and non-Hispanic Black patients are more likely to report more pain sites, worse pain intensity, and higher levels of pain. They were also more likely to have concurrent depression and pain self-efficacy than White hospice patients.
Other factors contributing to disparities include lack of knowledge about end-of-life care options, mistrust of the healthcare system, and poor communication between clinicians and patients. Hospice care may be perceived as a luxury in some communities, even though Medicare and Medicaid benefits require little out-of-pocket expenditure.
Language differences can lead to misunderstanding and misinformation that affect medical decision-making. For example, the word hospice may be translated to hospicio in Spanish, meaning “orphanage” or “place for poor people or poorhouse” (Reverso Dictionary, 2025).
Recent studies show minority cultures, such as Latinx and African Americans, use hospice services to a lesser degree than White patients. African American patients may suspect that since hospice care is less costly than more aggressive care, it is being offered for the financial gain of the hospital. They may also feel that hospice care is being offered to deprive them of the more acute care they deserve. African American, Hispanic, and other racial minorities may also believe that the absence of lifesaving treatments is forbidden by their particular religion (Robison et al., 2023).
LEGAL AND ETHICAL FACTORS IN END-OF-LIFE CARE
The Right to Die
The right-to-die concept includes assisted suicide (also called physician aid in dying [PAD]) and voluntary active euthanasia. In assisted suicide, the healthcare practitioner, usually a physician, provides the means to end life—such as a prescription for a lethal amount of drugs, the drugs themselves, or other measures—by a patient or a person who has knowledge of the patient’s intention.
However, according to the American Nurses Association Code of Ethics, provision 1.4, “The nurse provides interventions to relieve pain and other symptoms in the dying patient consistent with palliative care practice standards and may not act with the sole intent to end life” even though such action may be motivated by compassion, respect for patient autonomy, and quality of life considerations (ANA, 2025).
Both nurses and physicians are confronted with requests for assistance in dying. However, as of 2025, this practice is legal in only 11 states and Washington, DC.
- In 1994, Oregon became the first state to pass right-to-die laws.
- Washington and Montana (2009) soon followed; while the law in Montana does not allow a specific PAD or right-to-die procedure, it states that assistance does not violate any current state laws.
- In 2013, the Vermont legislature passed a right-to-die law by a 75–65 vote. The guidelines for practice are very stringent.
- In 2015, California became the fifth state to pass a right-to-die law, allowing terminally ill patients the right to end their own lives by using a lethal dose of medications ordered by a physician and self-administered. Two physicians must attest to the patient as being terminal within six months and mentally capable of making the decision. The California law passed after much debate, advertising on both sides, and input from healthcare providers, parents of terminally ill children, and religious leaders.
- Other jurisdictions that have adopted physician-assisted suicide (PAS) or right-to-die laws include Colorado (2016); Washington, DC (2017); Hawaii, Maine, and New Jersey (2019); New Mexico (2021); and Delaware (2025).
(Compassion & Choices, 2025)
Healthcare practitioners acknowledge that there is an “underground” practice of assisted suicide in the United States. Some maintain that the principle of double effect is used to justify what is really assisted suicide. The principle of double effect states that the potential to hasten imminent death is acceptable if it is the unintended consequence of the primary intention to provide comfort and relieve suffering. That is, analgesia and sedation may be given to a terminal patient for the purpose of alleviating pain or suffering and may result in death whether deliberately or inadvertently (Stanford University, 2023). For example, a terminal patient with severe difficulty breathing may be given large doses of narcotic to relieve suffering. As the breathing is eased by the narcotic, there may be a second effect that stops breathing altogether.
Palliative Sedation Therapy
Palliative sedation therapy (PST) is considered a “last-ditch” option in end-of-life care to relieve terminal suffering. It is used when symptoms have proven refractory to other measures or treatments. PST may be used to treat intractable pain and suffering when other measures such as a physician-assisted death is not an option. Narcotic pain medications mixed with sedation for comfort and anti-anxiety medications may have the sometimes unintentional result of terminally sedating the patient (Bhyan et al., 2024).
Palliative sedation therapy is controversial. Some opponents have incorrectly equated it with euthanasia. Euthanasia and PST are different in intention (relief of intolerable suffering in PST versus killing the patient in euthanasia), in procedure (use of a sedative for symptom control in PST versus use of a lethal agent in euthanasia), and in outcome (alleviation of suffering in PST versus immediate death in euthanasia).
As pain escalates and becomes more difficult to control, it may be necessary to consider palliative sedation. Palliative sedation is an appropriate method to consider when symptoms are refractory (not adequately controlled with conventional treatment options). Poorly controlled pain, agitation, refractory dyspnea, nausea, and vomiting are the primary reasons for using palliative sedation (Bhyan et al., 2024).
GENERAL CRITERIA FOR PALLIATIVE SEDATION
Determining the appropriateness of initiating palliative sedation is performed by the clinician and facility staff. The following general criteria are provided as a basis upon which to make such a determination:
- The candidate for palliative sedation must have a terminal illness where death is almost certain.
- The patient’s clinical presentation must be such that conventional therapies are incapable of providing relief despite maximal doses, and symptom relief cannot be obtained without affecting consciousness.
- Alternatively, a scenario can exist when conventional therapies are associated with potential adverse outcomes in patients at high doses or frequent administration of agents and thus warranting the use of palliative sedation.
- Palliative sedation can be considered if traditional therapies cannot provide relief of symptoms in a timely manner.
- Well-documented goals of care discussions with the patient or surrogates must be present to outline the plan of care and potential risks of using palliative sedation.
(Bhyan et al., 2024)
The role of the nurse in palliative sedation includes the administration of medications, recognizing and notifying healthcare practitioners of refractory symptoms, providing psychosocial support and education to the patient and family, and identifying culturally specific needs related to dying and death. Nurses have a responsibility to provide symptom relief and prevent suffering in dying patients (ANA, 2025). It is important to palliative nurses that consent by the patient or family be given before administering potentially lethal doses of sedation to the terminally ill.
TYPES OF PST
Two types of palliative sedation may be used in end-of-life care: proportionate palliative sedation (PPS) and palliative sedation to unconsciousness (PSU), also called gradual continual deep sedation (CDS). In PPS, medications such as benzodiazepines are increased gradually together with other symptom-relieving measures until suffering is relieved during both waking and sleeping hours. Survival following PPS was longest with higher sedative doses, an observation that may help dispel fears concerning the use of PPS to hasten death (Lightner, 2022).
In PSU, unconsciousness is the intended goal of sedation rather than a side effect. Medications are increased rapidly over minutes and hours to achieve unconsciousness and left at that level until death occurs. PSU is usually administered when the imminently dying patient finds severe physical symptoms intolerable despite state-of-the-art palliative care.
However, controversy surrounds the use of PSU to treat psychological, existential (a loss or interruption of meaning, purpose, or hope in life), or spiritual suffering. Some consider these to be outside the realm of a physician’s expertise, and others consider them within the knowledge, tools, and expertise of the interdisciplinary team.
Health professionals must understand the difference between the practice of PPS and PSU and the ethical issues surrounding their use. Palliative sedation used to be referred to as “terminal” sedation, but there was some ambiguity as to whether the term terminal referred to the sedation or the patient. “Palliative” sedation was considered more appropriate, as palliation of the unwanted symptoms was the desired effect. Nurses understand that the timing and appropriateness of palliative sedation is crucial to the patient or family’s comprehension and consent. Patients and families need to understand these last-resort options and make decisions about such end-of-life care before the need arises (Lightner, 2022).
Healthcare practitioners must also recognize that the patient always has the right to stop unwanted medical treatments or procedures while they are in progress—as was the case prior to consenting. These procedures may include CPR, mechanical ventilation, and artificial nutrition and hydration.
CASE
Doris is in the terminal phase of stage IV pancreatic cancer and experiencing severe abdominal pain much of the time. She has been under hospice care and requires proportionate palliative sedation (PPS) to achieve any degree of relief from the pain. It is Doris’s expressed wish that she not be left in intractable pain, and she has named her daughter Sheila in her advance directive to make medical decisions if she is unable to make decisions for herself. Sheila has been estranged from her mother for seven years but is now at her side most of the time.
The PPS has left Doris comfortable, rousable, but barely coherent. When her mother is unable to answer questions, Sheila asks that the PPS be reduced, stating her mother would want to be able to communicate with family. When the PPS is withdrawn, Doris becomes more lucid but complains of severe abdominal pain and asks for more pain medication. This results in periods of unresponsiveness, causing Sheila to again instruct the nurses to decrease the medication.
Donna is the charge nurse on Doris’s unit and has 20-plus years of experience in oncology. She arranges a conference for the following day with the family, including Sheila, the palliative care nurse, the primary physician, and Donna herself. Sheila is encouraged to express her fears of losing her mother and her hope to have time to communicate with her first. The group discusses the severe level of pain caused by pancreatic cancer and Doris’s wish that she not experience intractable pain. A compromise is reached that takes both Doris’s and Sheila’s wishes into consideration.
Removing or Deactivating Cardiovascular Implants
Implanted cardioverter/defibrillators (ICD) are used to correct life-threatening dysrhythmias. An actively dying patient may develop ventricular tachycardia due to hypoxia or electrolyte imbalances. One third of patients with ICDs will experience a shock in the last 24 hours of life unless the device is removed or deactivated. The shocks can potentially cause pain, distress, and anxiety and may prolong the dying process (Oliveira et al., 2024).
A 2010 consensus statement from the Heart Rhythm Society (reaffirmed in 2023) suggests that patients nearing the end of life (or their healthcare proxy) have the right to decide whether to have these pacemakers or other cardiovascular implants removed or deactivated. The statement was developed in collaboration with several organizations, including the American College of Cardiology and the American Heart Association. It explicitly states that removing or deactivating an implanted cardiovascular device near the end of life “is not physician-assisted suicide or euthanasia.” However, it also states that physicians or other caregivers cannot be compelled to carry out a procedure that conflicts with their ethical values. In such cases, the physician cannot abandon the patient but rather should refer the patient to a colleague willing to carry out the task.
An international group of experts from the Heart Rhythm Society (HRS), European Heart Rhythm Association (EHRA), Asia Pacific Heart Rhythm Society (APHRS), and Latin American Heart Rhythm Society (LAHRS) collaborated to issue updated recommendations for remote monitoring of cardiovascular implantable electronic devices (CIEDs) such as pacemakers, implantable defibrillators, and implantable loop recorders. Removal of these devices in end-of-life care was included in these recommendations (HRS, 2023).
ETHICS AND PALLIATIVE CARE
Nonmaleficence and justice are two ethical principles pertinent to healthcare. Nonmaleficence means doing no harm to the patient, and justice refers to the fair distribution of health resources. Nonmaleficence in taking care of patients at the end of life involves making sure they are kept comfortable with palliative care while not being denied the basic care they need. Justice involves distributing this care regardless of a patient’s age, gender, color, ethnicity, personal favor, or social economic status.
Advance Directives (ADs)
Advance medical directives are documents containing patients’ oral and written expressions of their preferences about future medical care if they should become unable to speak for themselves. ADs usually name another person chosen to make healthcare decisions for the individual when they are no longer able to make decisions.
Federal law (the Patient Self-Determination Act) requires hospitals to inform patients that they have the right to complete an advance directive. Advance directives are regulated by state law and therefore differ from state to state.
Such documents usually address the patient’s wishes regarding:
- CPR (cardiopulmonary resuscitation)
- Ventilator use
- Artificial nutrition (tube feeding) and artificial hydration (intravenous [IV] fluids)
- Comfort care
Approximately 45% of Americans have advance directives (ADs) or living wills, which is a considerable increase over previous years. Older patients with chronic disease(s) are especially encouraged to have advance care planning in place (NIA, 2022). The use of ADs varies according to race/ethnicity. According to the American Psychiatric Association, Asian American/Pacific Islander (35.3%) and White (56.1%) patients are more likely to have ADs than Black (34.4%) and Latinx (29.0%) patients. Many patients may feel that ADs are not necessary because family and physicians should already know what their wishes are (Liu et al., 2023).
DISPARITIES IN ADVANCE CARE PLANNING
A large study of 10,220 elderly patients performed in a major Northern California university hospital aimed to improve rates of advance care planning (ACP) for hospitalized patients aged >75. Overall rates of ACP documentation improved from 14% in the preintervention period to 44% in the intervention period, with a 2.47% average improvement each month of the study. However, differences in improvement rates indicated significant disparities across race and ethnicity, with Latinx and Black patients having lower rates of improvement (Dutta et al., 2023).
When a surrogate is making end-of-life decisions for a patient, the surrogate will be expressing the wishes of the patient that they have previously discussed. Particularly in the case of chronic illness in which a slow physical or mental decline takes place, advance directives provide the opportunity to ensure that a person’s own preferences will be followed. Copies of the advance directive may be given to family, care providers, one’s hospital, an attorney, or others. The plan should be reviewed periodically to provide for necessary updates (NIA, 2022).
A video can also be made explaining the patient’s precise wishes, although this is not a legally compelling document.
Healthcare professionals have an obligation to work with patients and their families to reach decisions that balance autonomy and beneficence. However, healthcare professionals are legally constrained from witnessing an AD if they are an employee of the organization in which the patient’s wishes will be enacted.
LIVING WILL AND MEDICAL POWER OF ATTORNEY
In most states, an advance directive can be either a living will or a medical power of attorney, also called a durable power of attorney for healthcare, a healthcare proxy, or declaration or appointment of a healthcare agent. Living wills and medical or durable powers of attorney predate ADs but may still be in use among older patients, and healthcare workers should be able to distinguish among the various forms.
A living will is a document written while alive to dictate preferences for healthcare decisions. It addresses personal preferences regarding the above-mentioned life-sustaining measures and under what circumstances the patient would prefer those measures be performed or withheld.
A medical or durable power of attorney (DPOA) is a legal document that names one or more people to make decisions for the person who is unable to make their own wishes known (Jain, 2025). Referred to as a healthcare proxy (representative, agent, or surrogate), this person(s) is named on the advance directive form. It is essential that a very specific conversation take place between the patient and the person named in the DPOA to ensure that there is clear understanding about the patient’s final wishes.
PHYSICIAN ORDERS FOR LIFE-SUSTAINING TREATMENT (POLST)
Several states have adopted an advance directive form developed in Oregon and known as POLST (or physician orders for life-sustaining treatment) (WSDOH, 2025). This simple form, to be completed and signed by both patient and a physician or nurse practitioner, specifies the patient’s preferences concerning measures such as antibiotics, artificial nutrition (including tube feeding) and hydration, CPR, comfort measures, and mechanical ventilation/respiration.
The form is printed on brightly colored paper and stays with the patient during transfers from one care setting to another. Patients at home often keep the POLST form on the refrigerator, where emergency responders can find it. Long-term care facilities retain POLST forms in residents’ charts.
In other states, the medical orders for life-sustaining treatment (MOLST) form is used instead of the POLST form. The two forms are very similar. The main differences are in the wording related to intubation or nonintubation (NI), the degree to which resuscitation measures will be carried out, and the position on the use of comfort measures (AANP, 2025; Burtka, 2025).
(See also “Resources” at the end of this course.)
DO-NOT-ATTEMPT-RESUSCITATION (DNAR) ORDERS
Do-not-attempt-resuscitation orders (formerly known as do-not-resuscitate [DNR] orders) have been renamed to emphasize the minimal likelihood of successful cardiopulmonary resuscitation (CPR). Additionally, a specific order to refrain from intubation is referred to as do not intubate (DNI).
Patients and families must understand not only the unlikely success of resuscitation but also the risks involved, which include fractured ribs, damaged internal organs, and neurologic impairment. Although the patient (or family) must ultimately decide about whether to attempt CPR, healthcare professionals explain that withholding CPR does not equate with letting someone die. Rather, a DNAR order can be considered an “allow natural death” (AND) order (Cleveland Clinic, 2025d).
The primary care provider should discuss the possibility of a DNAR order as soon as it is reasonable and while the patient is still able to make decisions. A delay in putting a DNAR order in place may result in treatment unwanted by the patient and in distress for the healthcare team.
The DNAR order should be readily available in the event of an emergency to ensure that the patient’s wishes will be honored. It should be posted prominently, either on the head or foot of the bed, or if the patient is at home, on the refrigerator. In the facility where the patient is admitted or resides, specifics of the order are also carefully documented in the patient’s chart.
If the patient’s preferences are not known at the time of a cardiopulmonary arrest, then resuscitation must be initiated. The resuscitation may then be stopped if it is learned that it is not in keeping with the patient’s wishes (AMA, 2025).
MECHANICAL VENTILATION (MV)
Mechanical ventilation is achieved by the introduction of an endotracheal or tracheostomy tube into the patient’s trachea. This provides an artificial airway through which air under pressure and oxygen can be used to simulate breathing. If the cause of a patient’s inability to breath adequately is temporary, such as pneumonia, use of MV can prolong life long enough for the needed treatment, such as antibiotics, to be provided.
Decisions about mechanical ventilation may be spelled out in a patient’s advance directive. Some patients choose to forgo MV, believing that it merely prolongs the dying process. Others choose to have MV when they can no longer breathe on their own (Bryan et al., 2024). Choosing MV may reflect the erroneous belief that this life-sustaining treatment can improve the patient’s prognosis.
Depending on the physician, choosing MV may affect the physician’s certification of the patient as terminal and, therefore, the patient’s eligibility for hospice benefits. Use of MV requires that the patient lie in bed or sit in a chair with restricted movement. If an endotracheal tube is used, the patient will not be able to speak or swallow. Mechanical ventilation also increases the risk of pneumonia because it prevents patients from coughing effectively and allows fluid to build up in the lungs.
Once MV is started, the decision to withdraw it may present a legal and ethical controversy for the physician and the family. In some cases, withdrawal of this life support may require a court order.
ARTIFICIAL NUTRITION AND HYDRATION (ANH)
Patients who receive hospice care have food and drink as they wish or need. Some individuals make their own choice, often as part of an advance directive, to stop or limit eating or drinking at a certain point in their dying process. When oral nutrition is no longer safe for a patient, ANH using enteral feeding tubes is sometimes used to deliver nutrition.
Decisions about whether to have ANH involve weighing the potential benefit against the burden to the patient. The decision needs to be individualized and reviewed regularly. In the case of a terminally ill patient, a decision must be made whether or not to initiate clinically assisted hydration (CAH) or nutrition (CAN). These require separate determinations by the patient or loved ones to decide how much care is the appropriate amount to continue (Davies, 2025).
Giving fluids at the end of life may have spiritual or emotional meaning, particularly to the family, beyond the physical effects for the patients. Giving fluids may be perceived as relieving thirst even when oral care with a minimal amount of fluid may have the same effect. Immediately before death the patient won’t feel thirsty. At the same time, giving fluids could cause fluid retention and discomfort. Fluid retention may also be exacerbated by renal shutdown at the end of life (Angela Hospice, 2023). Making decisions about giving food and fluids at the end of life have more to do with providing comfort than with gaining weight or hydration.
Although ANH may extend the patient’s life a few days or weeks, there is considerable physical and emotional trauma in inserting a nasogastric tube or undergoing surgery to place a gastrostomy (feeding) tube. There is also the increased risk of infection, increased risk of aspiration, erosion of nasal tissue, and increased diarrhea, all of which can prolong suffering. NG tubes are not recommended for patients at the end of life (AAHPC, 2025).
The potential burdens of ANH depend on the route of administration and may include sepsis (with total parenteral nutrition), aspiration (especially with tube feedings), diarrhea (also with tube feedings), pressure sores and skin breakdown, and complications due to fluid overload. Demented or confused patients receiving ANH may need to be physically restrained to prevent them from removing a gastrostomy tube, nasogastric tube, or central intravenous line. Pain, epistaxis (with a nasal feeding tube), pharyngitis, esophagitis, and airway obstruction may also occur. Phlebitis, bacteremia, or septicemia may occur with a central line. Many health professionals believe that hospice care with cessation of feeding and fluids is a more humane alternative to ANH (AAHPC, 2025).
There is widespread use of feeding tubes at the end of life, particularly in patients with Alzheimer’s disease or other cognitive impairment, even though there is not sufficient evidence to prove enteral tube feeding is beneficial in patients with advanced dementia. (See also “The Patient Who Has Dementia” later in this course.)
Research suggests that people who choose not to have ANH do not suffer due to hunger or thirst. Without ANH, in fact, patients are less likely to experience bloating or to develop pleural effusions (fluid around the lungs), which can cause shortness of breath, or fluid in the throat, which requires suctioning. Studies also indicate that forgoing artificial hydration increases the body’s production of endorphins (natural pain-relieving hormones), making the patient more comfortable and less likely to experience pain. The only side effect of dehydration at the end of life is dry mouth, which can be relieved by good mouth care or ice chips.
Clinicians can help families understand that forgoing ANH is not “killing” or “starving” the patient. Communication among the nurses and physician writing orders and taking care of the patient and those making decisions about care should guide the decisions made regarding AHN. Communication with family or surrogates with these fears can help assuage worries that the patient is “starving to death.” It is significant for them to know that inability to eat and drink is a natural part of dying (AAHPC, 2025).
CASE
Kathy, a hospice nurse, was questioned by the family of an older patient on hospice care in the nursing home where she worked. When the discussion turned to a decision about providing artificial nutrition and hydration for their loved one, a few of the family members expressed concern that withholding nourishment and liquids would cause unnecessary suffering by “starving her to death.”
Kathy gently explained to the family that studies have shown no benefit in giving tube feedings or intravenous therapy to dying patients and that these measures could, in fact, cause additional pain and other burdens, such as aspiration or diarrhea, on their loved one. Kathy assured the family that the nursing staff would continue to keep the patient comfortable, give her pain medication when needed, and provide mouth care and moisten her mouth with ice chips to keep it from feeling dry.
EFFECTIVE COMMUNICATION WITH PATIENTS AND FAMILIES
Although talking about illness and death can be difficult for both health professionals and patients, studies show that most patients want to discuss these issues. Sharing bad news while maintaining hope is a delicate balance that takes practice to achieve. The patient is encouraged to discuss these matters with those who are closest to them, especially with any person who is named as a healthcare proxy in an advance directive.
The definition of family may include more than those people with a common heritage, such as those with whom the patient has a very close relationship. It may incorporate unmarried life partners, family friends, roommates, and close friends (Makic & Morata, 2024).
Many people who do not fear death do fear the process of dying, the prospect of pain and suffering, and being a burden to their families.
The healthcare professional must demonstrate nonjudgmental acceptance of the patient and family’s composition, values, and personal feelings. This includes supporting the patient’s and family’s hopes for prolonging life as well as their hopes for peace and dignity throughout illness, dying, and death. Effective management of pain and other symptoms as well as emotional and psychological support of the patient and family are always possible (NIA, 2023).
Effective communication by hospice nurses and all of the members of the multidisciplinary team enhances symptom management for the patient, reduces family caregiver burnout and distress, and potentially improves bereavement adjustment.
Preparing for Death
Preparation for impending death is one of the most crucial experiences that a person can have. In addition to selecting a healthcare proxy, making decisions about lifesaving or extraordinary measures, and financial planning, a person must face their own feelings about death. The conversations with family, loved ones, the healthcare proxy, clergy, and healthcare professionals must be open and honest about the patient’s wishes. This may also lead to discussions about beliefs and values around death.
Coming to the end of life includes tying up loose ends, saying goodbye, and giving thanks, whether or not a patient is religious. Loose ends usually include financial arrangements, typically in the form of a will or a trust. Saying goodbye includes those closest to the patient, favorite activities or locations, and possessions. Giving thanks may include working with a spiritual advisor or simply reflecting on one’s life. If they are able, patients at the end of life often spend time contemplating significant events and turning points in their lives. A patient’s own spiritual beliefs, or lack thereof, will influence this reflection and contemplation (Kang et al., 2023).
Elements of Good Communication
There are certain factors that promote better communication between clinicians and patients and loved ones during end-of-life care and others that interfere with communication. Recognition of these factors will enable healthcare workers to improve communication between both sides of the care partnership and provide opportunities for greater comfort for the patient.
Some factors that may improve communication include:
- Including family, friends, and caregivers in communication
- Providing a quiet place with no distractions
- Explaining things to the patient in a way they can understand, including using writing, pictures, and objects
- Speaking clearly and ensuring understanding, particularly if there is a potential language barrier
- Listening attentively and assuring one has understood
- Using plain language instead of medical jargon
- Asking open-ended questions
Factors that may hinder communication include:
- Asking “yes/no” questions, which typically elicit a one-word answer
- Speaking a foreign language
- One party not clearly understanding what the other is saying
- Illnesses that can affect communication (e.g., motor neuron disease [MND], Parkinson’s disease, multiple sclerosis [MS], head or neck cancer, stroke, brain tumor, severe dementia, severe head injury)
- Lack of access to a speech and language therapist
- Sensory impairment (e.g., deafness, sight loss)
- Learning disabilities
- Emotional distress
- Drowsiness or unconsciousness
- Attempting to communicate while wearing personal protective equipment (PPE)
(Marie Curie, 2022)
FAMILY CONFERENCES FOR PATIENTS DYING IN THE ICU
Families are intricately involved in the end-of-life decision-making process for a family member with a serious illness who is in the ICU setting. However, families are not always as involved and as informed as they would like to be. Therefore, end-of-life family conferences are an important part of ICU practice in many hospitals because they help relieve stress and anxiety for those with loved ones dying in the ICU. These conferences may also reduce the length of stay in the ICU and improve communication between the clinical staff and the patient’s family.
Ideally, these conferences are held in a quiet room once the family has been given sufficient time to gather. They allow for discussion of the patient’s situation and an opportunity for the family to ask questions, express concerns, and confront painful emotions with the help of caring, compassionate professionals. Those included in these discussions are typically the attending physician, the nurse most familiar with the patient, and possibly a member of the clergy.
Guidelines for these conferences are based on the VALUE mnemonic:
| V | Value what the family members say |
|---|---|
| A | Acknowledge their emotions |
| L | Listen |
| U | Understand the patient as a person through asking questions |
| E | Elicit questions from family members |
(Hwang et al., 2025)
Cultural Sensitivity
Culture is often defined as the set of attitudes, beliefs, and values that people and societies pass down between generations. Cultural competency requires that healthcare professionals understand cultural differences in order to be effective and respectful in their delivery of care. This involves acquiring specific knowledge about the beliefs and practices of different cultures as related to healthcare and end of life. Thus, it is important that clinicians ask open-ended questions rather than make assumptions based on appearances. Cultural sensitivity also includes the avoidance of stereotyping and the recognizing of one’s own implicit biases.
DIVERSE PREFERENCES
Cultural beliefs about healthcare, especially end-of-life issues, are as diverse as the different cultures that seek healthcare. Some examples of this diversity are discussed below.
African Americans may value personal autonomy and often mistrust the healthcare system because of observations of disparate treatment of their community in the delivery of care. A desire for aggressive interventions results in a low percentage of terminal African Americans agreeing to hospice care. African Americans may fear that acceptance of palliative or hospice care will prevent them from receiving the care they desire, and prior difficulties with access to healthcare may color their acceptance of less aggressive care. Trust must be established for a therapeutic relationship to work well.
Close families are evident in African American culture. Health decisions are commonly made with input from family members. Whether a patient’s own literacy is high or low, their health literacy may be low. It is necessary to perform a “teachback” when educating patients and their families by having them repeat and explain what they have just learned. An example of this would be to explain how traditional dishes could be modified to make them healthier after some nutritional teaching (BDO, 2025).
Because hospice care is considerably less expensive than care that would occur in an acute care hospital, particularly in the ICU, non-White patients and families may question solutions that may have the appearance of not including the best care possible. Again, this may be based on prior difficulties with access to care.
When a loved one is dying in the hospital, Latinx patients and families often express preferences for care through a male spokesperson. Often the request is made that a priest or chaplain be present when healthcare professionals are discussing end-of-life issues. The interconnectedness of close-knit Hispanic families often leads to group decisions to enlist professional help after trying more traditional remedies such as herbal preparations and homeopathies. It is felt that there is a burden placed on the family to understand much of the healthcare procedures and that the paperwork handed out to aid in comprehension is not helpful. Healthcare access and language barriers can make obtaining adequate care a significant challenge. Latinx patients and family often communicate that having caregivers of a similar race/ethnicity is more comfortable (Well-Wisp, 2025).
Latinx families who are strongly Catholic often request that the patient’s rosary beads be placed in the dying patient’s hands or taped to the frame of the bed. The patient and family may feel comforted if a priest performs the Sacraments of the Sick (no longer called Last Rites) for the patient. Language barriers can be a significant challenge in cases where patients or family members do not speak English. Older Latinx patients are less likely to have advance directives and prefer comfort care at the end of life.
In Latinx communities, promotores may prove helpful in implementing patient education and communication strategies. Promotores are community members who promote health in their own communities and help alleviate access-to-care barriers. As members of minority and underserved populations, they are in a unique position to build on strengths and to address unmet health needs in their communities (MHP Salud, 2022).
Asian Americans are the fastest-growing ethnic population in the United States. Asian Americans make up 7% of the total U.S. population at present and are expected to reach 10% of the population by 2050 (Pew Research Center, 2025). There is a wide variety of Asian backgrounds, which includes those from the Far East, Southeast Asia, and the Indian subcontinent.
Certain aspects of cultural competence are considered when caring for Chinese patients. Traditional Chinese Medicine (TCM) practices, including acupuncture, herbal medicine, and dietary therapy, are based on the concepts of qi (vital energy) and the interplay of yin and yang (the dual forces of nature). These may be used in conjunction with Western medical practices. Blood also holds symbolic meaning in Chinese culture and is associated with vitality and life force, which may introduce certain taboos or beliefs about practices such as blood donation. Health is a family affair and includes involving family members in making medical decisions. Elders are highly revered and consulted for their wisdom (SOHO, 2024).
Pakikisama is a Filipino trait of comfortableness and getting along with others that may increase the level of trust in a healthcare clinician. Younger family members often act as healthcare navigators. Filipinos have a higher prevalence of cardiovascular comorbidities such as hypertension, diabetes, and dyslipidemia (Jose et al., 2024). Dietary traditions include an emphasis on carbohydrates, fruit, vegetables, and sweets.
Healthcare practices are very different in the Southeast Asian Hmong community when compared to Western medicine. A traditional Hmong belief is that illness is caused by spirits and soul loss. The decision to seek Western medicine versus a traditional shaman may therefore depend on whether the illness is believed to be spiritual in nature. The fundamental conviction about death in this culture is that it is a journey from the physical to the spiritual world. Elaborate religious ceremonies are undertaken during dying, including an altar built by the eldest son. The family must be involved in all decision-making. Withholding lifesaving procedures is considered disrespectful. The preferred scenario is for the patient to die at home, as this is believed to bring good fortune to those in the household (Fadiman, 1997).
White people tend to receive more healthcare services and spend more money on those services than Hispanic and African American patients. White Americans are less likely to seek aggressive treatment at the end of life and are less likely to die in a hospital than their Hispanic or African American counterparts (Dutta et al., 2023).
BENEFICENCE VS. TRUTH-TELLING
Whereas the mainstream U.S. model of end-of-life care values autonomy (i.e., right to self-determination) and truth-telling, healthcare models in other cultures may place a greater value on beneficence, which may include protecting the patient from bad news about their serious illness. In such cultures, disclosure of serious illness may be considered disrespectful, impolite, or even harmful to the patient.
Learning about the patient’s and family’s cultural values can begin with a simple statement followed by an open-ended question: “Some people want to know about their illness and others do not. Some patients would prefer that I talk with a family member instead. How do you feel about it?” This gives the patient the option to refuse or accept information about diagnosis or prognosis and to designate a family member to act as a surrogate. This also helps to determine the patient’s or family’s wishes regarding who is given information about a patient’s prognosis or progress.
Researchers suggest three strategies for addressing the “secrecy” dilemma and other cultural differences in end-of-life care:
- Detailed information to increase the knowledge about palliative and hospice care
- Use of case assessment tools to determine communication preferences and the family’s role in decision-making
- Providing culturally sensitive end-of-life navigation
(Akdeniz et al., 2021)
MANAGEMENT OF PAIN AND OTHER SYMPTOMS
Many people who have come to terms with their own mortality still fear the possibility of a painful death. Almost all pain can be controlled to some extent with the wide range of available treatments. When properly treated, most patients gain significant relief from pain.
Pain is frequently multidimensional, with psychosocial, emotional, and spiritual components. Other symptoms, distress, or psychosocial or spiritual concerns can interact with and exacerbate physical pain or impact the effectiveness of pain treatment (Harding et al., 2023). Pain not only hurts, but it is also physically and emotionally debilitating. Severe chronic pain can cause depression, anxiety, fear, diminished appetite, impaired sleep, irritability, inability to focus, and sometimes thoughts of suicide. When pain is relieved, many of these symptoms may disappear. The patient then can focus on other end-of-life issues, such as important decisions, unfinished business with family and friends, or spiritual or religious concerns.
The patient’s preferences should define the goal of pain management. Some patients will choose to be completely pain-free, even if it means sedation. Others will choose to control pain only enough so that they can continue to function with alertness. If pain becomes severe at any time, but particularly in the last days or hours of life, it may be treated around the clock (Harding et al., 2023).
Patients have a right to appropriate assessment, management, and relief from pain. The Joint Commission requires that hospitals and other healthcare facilities regularly assess, monitor, manage, and document pain and response to treatments in all patients. Those facilities that fail to do so risk losing accreditation. Until all health professionals learn the principles of pain management explicit to palliative care, however, patients will continue to suffer needlessly.
Inadequate education of health professionals in pain management is only one reason why patients suffer. Another is general mistrust about the use of narcotic analgesics and worry about addiction or overdosing on these medications. Patients may also consider requests for pain medication as “giving up” or “giving in” to their disease. Clinicians can correct these myths and misinformation and reassure patients that managing their pain is fundamental to improving their quality of life.
Although addiction is not a concern when treating dying patients, tolerance to and a chemical dependence on opioids may develop over time. If tolerance to particular drugs occurs, it will be necessary to increase the dosage or change medications to gain relief. If dependence develops and the patient needs to be taken off the drug, it should be done gradually in order to avoid withdrawal symptoms.
Assessing Pain
Effective pain management begins with assessment of the patient’s pain, and reassessment at appropriate intervals is crucial.
Because pain is a subjective experience, it is important to ask the patient to describe the pain in terms of location, intensity, and character. There are a number of pain assessment tools available; healthcare practitioners should consult their agency/facility protocols.
A thorough pain assessment includes:
- Onset (gradual or sudden, which may be difficult to determine with chronic pain)
- Mechanism of injury or etiology of pain (if identifiable, but may not be determined)
- Location/distribution
- Duration (unrelieved pain can cause physical changes or result in chronic pain)
- Course or temporal pattern (decreases with time and may end with recovery)
- Character and quality of the pain
- Aggravating/provoking factors
- Alleviating factors
- Associated symptoms (although objective signs of pain such as grimacing or tachycardia may not indicate pain unless the patient concurs)
- Severity/intensity (varies in response to the same stimuli)
- Impact on function, sleep, mood
- Barriers to pain assessment
(Harding et al., 2023)
Pain perception varies from person to person and is subjective. It may depend on age, culture, emotional status, past experiences with pain, and the source and meaning of the pain. Some cultures dictate stoicism when experiencing pain, which may cause people not to admit pain or request medication. Men are more likely to “tough it out” because of cultural and gender attitudes.
Older adults may have a higher pain threshold than younger people or children due to normal age-related changes in neurophysiology. Because of their higher pain threshold, however, older patients are at risk for undertreatment of pain. They may also have multiple chronic diseases and sources of pain as well as complex medication regimens that increase the risk of drug-drug and drug-disease interactions.
Visual, hearing, motor, and cognitive impairments as well as language differences can impede communication about patients’ pain. Anxiety and depression can exacerbate the pain experience, as can fatigue and sleeplessness. Untreated pain can then cause further sleeplessness, which leads to more fatigue, setting up a cycle of suffering.
Knowing the source of pain can be a relief in itself, particularly if the patient has imagined a worst-case scenario and the source of the pain turns out to be a minor, correctable condition. The meaning of pain also affects the patient’s perception of it.
Pain should be reassessed at least as often as the vital signs are taken and management efficacy reassessed when patients are transferred from home to any new healthcare facility (Harding et al., 2023).
Pain Medications
A team may be assembled to make determinations about the best pharmacological treatment for patients in pain. This team may include pain management nurses, nurse practitioners, clinical nurse specialists, anesthesiologists, and clinical pharmacists.
Medications can make a drastic difference in the lives of those suffering with pain, and they comprise an important aspect to end-of-life care in many instances. (A detailed description of pain medications is beyond the scope of this course, but the following provides basic information.)
The World Health Organization (WHO) initially developed a three-step analgesic “ladder” for cancer pain relief in adults, and this approach was also used in palliative and end-of-life pain management. If pain occurred, there would be prompt oral administration of drugs in the following order:
- Nonopioids (aspirin and acetaminophen)
- Then, as necessary, mild opioids (codeine)
- Then strong opioids (e.g., morphine) until the patient is free of pain
To calm fears and anxiety, additional drugs (adjuvants) could be used. To maintain freedom from pain, drugs would be given “by the clock” (i.e., every 3 to 6 hours) rather than on demand or prn. This three-step approach of administering the right drug in the right dose at the right time was inexpensive and 80% to 90% effective (Anekar et al., 2023).
This three-step analgesic ladder later became the subject of multiple studies, and some perceived flaws resulted in the creation of a fourth step that added invasive and minimally invasive treatments for pain. Examples include epidural analgesia, intrathecal administration of analgesic and local anesthetic drugs with or without pumps, neurosurgical procedures (e.g., lumbar percutaneous adhesiolysis, cordotomy), neuromodulation strategies (e.g., brain stimulators, spinal cord stimulation), nerve blocks, ablative procedures (e.g., alcoholization, radiofrequency, microwave, cryoablation ablations, laser-induced thermotherapy, irreversible electroporation, electrochemotherapy), cementoplasty, and palliation radiotherapy.
Some studies further suggested that the second step (use of moderate opiates) be eliminated. Others showed that the long-term treatment of severe cancer pain should be uniquely treated (Anekar et al., 2023).
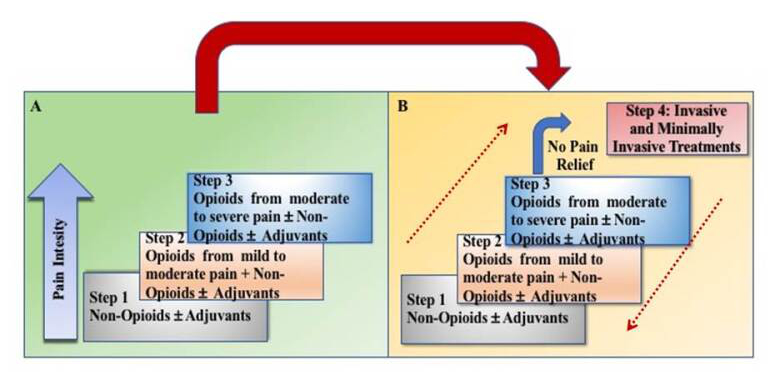
Revised WHO analgesic ladder, with an additional Step 4 and a bidirectional approach. (Source: Marco Cascella, MD. Public domain image.)
DRUG ADMINISTRATION
When a patient is unable to swallow an oral medication, less invasive routes (rectal, sublingual, or transdermal) should be offered first. Parenteral methods should be used only when simpler, less-demanding, and less-costly methods are inappropriate, ineffective, or unacceptable to the patient. Intravenous (IV) or subcutaneous doses should be chosen over intramuscular (IM) injections, as they are less painful and absorb at a comparable rate. In general, assessing the patient’s response to several different oral opioids is advisable before abandoning the oral route in favor of anesthetic, neurosurgical, or other invasive approaches (Harding et al., 2023).
Oral transmucosal fentanyl citrate is used for the relief of breakthrough pain. The lipid solubility of fentanyl allows rapid onset of pain relief. Fentanyl can also be given in the form of an intranasal spray, topical skin patch, or a buccal tablet for patients who are unable to swallow pills.
End-of-life patients may experience agitation. Lorazepam (Ativan) is an anxiolytic/sedative that may be taken as an injection, intravenously, orally, or sublingually (McCuistion et al., 2023).
PROPER SAFEGUARDING OF NARCOTICS
Many end-of-life patients receiving palliative care or hospice at home possess large amounts of narcotics and other controlled substances to alleviate pain and control anxiety. While these are essential to keep the patient comfortable, abuse and disposal of such medications may pose problems. Improper disposal of these substances by flushing them down the toilet or into sinks may introduce them into the groundwater, drinking water supplies, or eventually the tissue of aquatic organisms.
Instead, unused drugs may be given to collectors who are registered with the Drug Enforcement Administration. Authorized collection sites may be retail pharmacies, hospitals, clinic pharmacies, and law enforcement locations. Some may offer mail-back programs or collection receptacles (drop boxes).
Equally important is the need to safeguard against the use of controlled substances in the home by anyone other than the patient for whom the medications were ordered, including children and pets (U.S. FDA, 2024).
(See also “Resources” at the end of this course.)
CASE
Isabella is a 76-year-old widow with an inoperable astrocytoma in the parietal lobe of her brain. She has undergone palliative radiation treatments in the hospital and has been discharged to home to be cared for by her 54-year-old daughter, Eileen, and a home health aide who comes every other day. Her physician has determined that she likely has less than six months to live and has designated that she is to be cared for as a home hospice patient.
Although her tumor has shrunk in size since the radiation therapy, Isabella still complains of severe headaches, up to 7 or 8 on the 0–10 pain scale. Her doctor has ordered ibuprofen with fentanyl patches for the pain. Isabella and Eileen are instructed to keep a log indicating when patches are applied and removed and how disposal of used patches is managed. Isabella is forgetful and occasionally neglects to remove the previous patch when she puts on the new one, every 72 hours. When this happens, she becomes confused, agitated, and even more forgetful. Also, she does not consistently maintain the log.
Eileen’s 28-year-old son, Paul, has a history of substance abuse and has been in rehab twice for narcotic addiction. Lately he has been secretly taking his grandmother’s fentanyl patches when he visits, telling himself they’re not good for Isabella. The home health aide notes that the count is off and notifies Eileen. She also notifies her agency supervisor. After reviewing all the circumstances (Isabella’s forgetfulness, the incomplete log, the presence in the house of a person with a known history of substance abuse), the supervisor instructs Eileen to lock up the supply of patches, remove and apply them to Isabella herself in order to prevent overdosing, and lock up the used patches as well.
ADDRESSING SIDE EFFECTS
The use of opioids affords effective pain relief to most patients. Like all drugs, however, they have side effects, some of which can be uncomfortable or even painful in themselves. They include drowsiness, confusion, nausea and vomiting, dyspnea, dry mouth, and constipation. Some side effects ameliorate after a few days, and most can be prevented or treated successfully.
Drowsiness
Drowsiness frequently occurs at the beginning of opioid therapy, not only from drug action on the brain but also because the patient may have been sleep-deprived due to unrelieved pain. Once normal sleep patterns resume, the drowsiness generally lessens.
Confusion
Confusion may occur at higher doses of opioids or an intolerance for the medication. The patient may be more sensitive to opioids or may be having a paradoxical reaction.
Nausea and Vomiting
Nausea and vomiting can usually be controlled once the source of the problem is identified. For patients who cannot tolerate morphine or NSAIDs, substitution of a different opioid or a sustained-release formulation may relieve these symptoms. Vomiting related to chemotherapy can be treated with serotonin receptor antagonists such as ondansetron, granisetron, or dolasetron.
If nausea and vomiting are related to disturbances of the labyrinth—such as motion sickness, vertigo, or migraine—use of antihistamines and anticholinergics (meclizine, dimenhydrinate, or transdermal scopolamine) may offer relief.
In some patients, nausea and vomiting can be triggered by smells, sights, or sounds; this is referred to as psychogenic or anticipatory vomiting. For these patients, benzodiazepines (anti-anxiety drugs such as lorazepam and buspar of the azapirone chemical class) may provide relief. Benzodiazepines can interfere with short-term memory, especially in older patients, or cause confusion in those who are already cognitively impaired.
Vomiting may also be related to increased intracranial pressure (e.g., from central nervous system tumors). These patients may benefit from a combination of corticosteroids and serotonin receptor antagonists.
Constipation may trigger nausea and vomiting in patients with advanced disease. Stimulant laxatives such as senna derivatives can promote gut emptying and offer relief.
Dyspnea
Dyspnea (shortness of breath, difficult breathing) is common among dying patients, who may report feelings of tightness in the chest or suffocation. Dyspnea may be an initial effect of opioid therapy or may result from other causes, including pneumonia, pulmonary embolism, pleural effusion, bronchospasm, tracheal obstruction, neuromuscular disease, restricted movement of the chest or abdominal walls, cardiac ischemia, congestive heart failure, superior vena cava syndrome, or severe anemia. Treatment is determined by the diagnosis.
Three basic approaches are used to treat dyspnea in the dying patient: oxygen, opioids, and anti-anxiety medications. Nonpharmacologic methods such as meditation or guided imagery may also be effective. Although most patients are not hypoxic, supplemental oxygen may be helpful unless the cannula or face mask cannot be tolerated. Fresh outdoor air or a breeze from a fan may also afford relief. Low-dose immediate-release morphine, in either oral or buccal formulations, also can be effective.
Constipation
Preventive measures against constipation should begin at the same time as opioid therapy. Normal bowel function varies from person to person, so it is essential to establish what the patient considers normal and whether they are having any difficulty with bowel movements. Preventive or treatment measures can then be tailored accordingly. Untreated constipation can cause bloating, abdominal pain, nausea and vomiting, overflow incontinence, fecal impaction, or bowel obstruction.
First-line therapy for constipation includes stool softeners and stimulant laxatives such as prune juice or senna derivatives. If these prove insufficient to maintain or restore normal bowel function, osmotic laxatives such as magnesium salts, sorbitol, or lactulose may be added.
A lubricant stimulant such as mineral oil may be used if the patient is able to swallow. However, mineral oil should not be given to patients who have difficulty swallowing, because aspirating mineral oil can cause pneumonia. Mixing the oil with orange juice or root beer makes it more palatable. It is given when the patient’s stomach is empty to avoid interference with fat-soluble vitamins.
If the patient is ambulatory, increased activity can help promote bowel function. Simple measures such as increased fluid intake, more dietary fiber (if tolerated), a regular toileting schedule, privacy, and if the patient is bedfast, use of a bedside commode rather than a bedpan can be helpful. Peristalsis is generally strongest after eating, especially in the early morning.
Dry Mouth
Pain medications and many other pharmaceuticals (e.g., antidepressants, anticholinergics) can dry the lips and oral mucous membranes, leading to cracking, ulceration, and bleeding. Patients on oxygen therapy and those who have chosen to forgo artificial hydration and nutrition may also experience dry mouth. When increasing fluid intake is not an option, lubricants such as liquid vitamin E or petroleum jelly applied to the lips can help prevent cracking. Mouth swabs moistened with water or alcohol-free mouthwash can be used to relieve discomfort and to clean teeth, gums, and tongue. Products containing alcohol are avoided or limited because they can further dry the mouth (McCuistion et al., 2023).
Nonpharmacologic Pain-Relief Measures
Not all pain relief comes through medications. Other methods, some of them simple, may increase patient comfort and well-being and augment the pain-relieving effects of drugs. For example, massage or application of heat or cold may reduce musculoskeletal pain. Repositioning the patient can sometimes relieve pain. Physical therapy may also be beneficial.
Adjuvant therapies for intractable pain include radiation therapy (to shrink tumors or relieve bone pain), radiofrequency ablation for bone pain, surgery to debulk a tumor, nerve blocks, or intrathecal pumps to deliver large doses of opioids without systemic sedative effects.
Complementary therapies such as acupuncture, guided imagery, biofeedback, hypnosis, progressive muscle relaxation (e.g., listening to audiotapes of relaxation techniques), meditation, distraction, hot and cold application, and music therapy can also be helpful, not only in relieving pain but also in relieving emotional and psychological distress. Psychotherapy, particularly for patients suffering from depression, can have a positive effect on patients’ perception of pain and response to pain medications. Support groups and pastoral counseling may also be helpful to some patients by reducing psychological distress (Harding et al., 2023).
Treating Other End-of-Life Symptoms
DELIRIUM
Delirium is a condition marked by changes in clinical and mental status caused by illness, changes in the environment, or cranial stress. It is defined as a disorder of global cerebral dysfunction characterized by disordered awareness, attention, and cognition. Delirium has been understood as prevalent and dangerous, particularly among adults over age 65 or frail patients, and is the most common neuropsychiatric disorder at the end of life
Disturbances in sleep–wake cycles and psychomotor activity, delusions or hallucinations, insomnia, and emotional lability may all occur. The agitation, moaning, and grimacing of delirium may be misinterpreted as signs of pain. The person may also exhibit mood swings, disorientation to time and place, and uncharacteristic speech. The most significant elements of delirium are inattention and broad fluctuations of symptoms. These are not major components of any other psychiatric illness of late life.
Delirium can create distress for both patient and caregivers, interfering with patient comfort and meaningful interaction with family members.
Many episodes of delirium can be effectively treated and, in some cases, prevented. Delayed treatment may result in terminal restlessness. Risk factors for delirium include cognitive impairment, sleep deprivation, medications such as narcotics or anti-anxiety drugs, hypoxia, fever, brain tumors or swelling, immobility, visual impairment, hearing impairment, and dehydration. Early identification and interventions to address these risk factors can significantly reduce the number and duration of episodes of delirium in older patients (Cleveland Clinic, 2025b; Harding et al., 2023). For example, the patient who normally wears glasses or a hearing aid may become confused without these appliances.
The principle of treatment of delirium is to determine and treat the reversible causes of delirium and to mitigate other causes. Determining one cause may be difficult and delay treatment. Delirium may be related to use of medications such as opioids, and changing to a slightly less potent opioid may be effective. Neuroleptic medications (antipsychotics) such as haloperidol are recommended to reduce agitation in patients with hyperactive delirium; however, they may cause drug-induced Parkinsonism and motor restlessness. Evaluating the clinical need for opiates, anticholinergics, benzodiazepines, and dopaminergics is critical to identify whether any CNS active medications can be discontinued (Harding et al., 2023).
FEVER
Some patients experience a significant fever, which may be evidence of an infection or the body’s response to chemotherapy or radiation therapy. At the very end of life, no effort is made to discover the source of the fever, as it will not be treated and obtaining cultures may be painful for the patient. However, a fever is expected to cause the patient discomfort. Acetaminophen may be ordered for the patient as an antipyretic. If the patient is unable to swallow pills, the acetaminophen may be given via suppository.
DRY EYES
Patients in a comatose or obtunded state may not fully close their eyes, allowing the uncomfortable possibility of dried corneas. Artificial tears (polyvinyl alcohol 1.4%) may be ordered to be administered every hour around the clock to lubricate the eyes, particularly when the eyes are not fully closed.
CASE
Mr. Willoughby is an 83-year-old hospice patient admitted to the hospital since his family is no longer able to care for him at home. He is unresponsive to all stimuli and unable to swallow. His respirations are 10 to 12 per minute; no other vital signs are being taken. The physician’s orders are as follows:
- DNAR
- Comfort care
- Turn every 2 hours
- Mouth care every 4 hours
- Lip balm every 8 hours
- Family may visit at all hours
Ordered medications include:
- Roxanol (immediate-release oral morphine sulfate solution) 20 mg/mL concentration, with a dosage of 0.5–1 mL every hour sublingually as needed for signs of pain
- Dulcolax suppository per rectum every day for constipation
- Artificial tears, 1 drop in each eye every hour
- Tylenol suppository, 650 mg per rectum every 4 hours as needed for fever or “hot skin”
- Ativan, 1 mg SL every 4 hours as needed for agitation
Luanne, his nurse, explains to the family that comfort care status doesn’t mean Mr. Willoughby will not be cared for. She explains that every usual nursing care activity in the hospital, such as collecting vital signs, is considered in terms of the discomfort it may cause the patient and the possible benefits that may be derived. Luanne explains the reasons for each of the physician’s orders and how they help keep the patient comfortable.
Family members express their wish to help and are encouraged to participate in Mr. Willoughby’s care. Luanne demonstrates how to turn the patient and support him with pillows. She tells them that gentle massage to the extremities and frequent application of lip balm to the patient’s mouth will help to keep him comfortable. However, family members are not allowed to administer medications in the hospital, not even over-the-counter remedies.
PSYCHOSOCIAL SUPPORT ISSUES
Coming to terms with one’s own mortality is different for each individual and is related to the way they handle other life challenges. Compassionate care and support from health professionals and loved ones are essential during this crisis. Adjusting to palliative care involves shifting the patient’s and family’s expectations from curing to healing. Even when cure is no longer possible, healing is.
In the landmark work Choices in Healing, Lerner (1996) defines healing as “an inner process through which a person becomes whole,” a process of transforming one’s life in a variety of ways in the face of death. This shift in expectations can help maintain hope, seen as crucial in overall adaptation to crisis. For example, the patient who has confidence that pain and suffering can be controlled will have hope for future quality of life. Patients who believe they are loved and cared for will have hope in their relationships.
Common End-of-Life Emotions
The person diagnosed with a terminal illness experiences a host of emotions, including those famously described by Dr. Elisabeth Kübler-Ross in her classic
These and other emotions described below are all normal reactions and deserve equal emphasis with physical care at the end of life. Effective coping with these reactions can improve the quality of life remaining and help the patient resolve important issues with family and friends.
DENIAL
Denial of a terminal diagnosis occurs when an individual is unable to believe the eventual outcome of death. This may take the form of disbelief in diagnostic test results, questioning whether an error has been made, or maligning the person who has made the diagnosis. Denial usually gives way gradually to an understanding that the diagnosis is, in fact, an accurate one, although denial may evolve to other stages in the process before acceptance of the diagnosis occurs, if at all (Fisher, 2023).
ANGER
Anger is common during terminal illness. Patients may express anger at the illness, the side effects (or failure) of medications and other treatments, disruption in life plans, changes in social roles and lifestyle, and the prospect of death. Validating a patient’s anger as a normal reaction to terminal illness can open a discussion of how to deal with the anger and make the most of their remaining time.
BARGAINING
Bargaining in response to a terminal illness means that an individual promises to change or enact certain behaviors in exchange for continued life. The bargaining may be proposed with one’s physician, the bearer of bad news, or even God. The idea is that the eventual outcome of death may be changed if the bargain is carried out (Fisher, 2023; Morrow, 2022). For example, someone with a diagnosis of terminal lung cancer may promise to quit smoking to extend life. Another person may promise to attend church.
DEPRESSION
Health professionals must distinguish between normal sadness and possible depression in each patient facing a terminal illness. Depression is commonly underdiagnosed in the general population; consequently, depression in dying patients may be a preexisting condition. Just as patients require ongoing evaluation for depression and anxiety throughout their course of treatment, so do family caregivers (Fisher, 2023).
An untreated diagnosis of depression may lead to an impaired quality of life. Severe depression may cause a shortened survival rate, increased pain, and suicide. Recognizing the symptoms in people with terminal illness and referring them for appropriate treatment can greatly improve their quality of life.
The patient who appears depressed should first be assessed for pain. Untreated or undertreated pain can cause depression and other symptoms.
SYMPTOMS OF DEPRESSION
- Feeling sad, anxious, or “empty” most of the day, almost every day
- Decreased interest or pleasure in almost all activities, including sex
- Decreased or increased appetite and/or weight changes
- Disturbed sleep patterns, sleeping more or less than normal
- Fatigue or agitation
- Feelings of worthlessness or excessive guilt
- Inability to concentrate or make decisions
- Recurrent thoughts of death or suicide, or suicide attempts
The following factors may suggest the need for early intervention to treat depression as part of end-of-life care.
- History of depression
- Feelings of disbelief, denial, or despair
- Weak support system (few or no family members, few friends, solitary work environment)
- Evidence of persistent irrational beliefs or negative thinking regarding the diagnosis
- Greater dysfunction related to the illness, such as pain, shortness of breath, appetite and sleep dysfunction, and decreased mobility
(NCI, 2024)
Patients with mild depression may be helped by supportive individual or group counseling with a mental health professional. More intense depression will likely require pharmacologic management in addition to counseling. Family and close friends of dying patients may also require counseling and temporary pharmacologic management (NCI, 2024).
Although depression in dying patients is not markedly different from depression in other medical conditions, treatment may be modified because of other factors, particularly other medications. Antidepressants such as tricyclics and selective serotonin reuptake inhibitors (SSRIs) have a delayed onset of action of up to eight weeks, and patients undergoing end-of-life care may not live a sufficient length of time to benefit from the antidepressant therapy (McCuistion et al., 2023).
ACCEPTANCE
Acceptance is the final stage of the grief process, in which the subject becomes able to reconcile oneself to the loss. While the other stages of the grief process don’t disappear, acceptance means that the person is close to being able to move forward from the loss.
FEAR
The most common fears are those of death itself, pain, dying alone, and being a burden. People with strong spiritual beliefs may not fear death but still fear the possibility of pain and suffering at the end of life. Fear can heighten the expectancy of pain and lead to symptoms such as distress, sleep disturbances, or anticipatory nausea and vomiting. Fear can substantially interfere with the quality of life. Health professionals with expertise in palliative care can reassure patients that pain and suffering will be relieved and that patients will not die alone.
Most people also have fears and concerns about loss of dignity and control. Caregivers can provide comfort by allowing the person to express any fears and concerns about dying and by reassuring the person that they will honor advance directives. They include patients in discussions about issues that concern them. They listen to patients reminisce about their lives. They encourage friends and family members to visit and talk to the patient as well, even when they progress to unresponsiveness or sedation. They may simply keep the person company; talking, reading, or just “being there” also can be comforting (Harding et al., 2023).
LOSS
Life is filled with losses, some minor (lost car keys), some major (job loss), some physical and tangible (losing hair during chemotherapy), others psychological and intangible (losing social contacts). Loss may be sudden and unexpected or anticipated and predicted. The meaning or value of what is lost to the individual determines the feelings that result.
Aging and the end of life involve a succession of losses, concluding with the ultimate loss: loss of self. Other losses may include:
- Loss of physical strength and abilities
- Loss of mental abilities (confusion/dementia)
- Loss of relationships
- Loss of self-esteem
- Loss of body image
- Loss of independence
- Loss of control over life plans and lifestyle
Experiencing multiple losses often leaves insufficient time to grieve those losses and creates feelings such as hopelessness, withdrawal, isolation, and anger. Physical weakness or pain can also diminish the ability to cope with loss (Harding et al., 2023).
GRIEF
Grief is a normal human response to loss, and it is universal, individual, and unpredictable. Researchers have proposed different models to describe the various stages of grief, but people do not always move through such stages sequentially or predictably. Each person progresses at their own pace and may move forward and backward through one or more stages, which can include:
- Shock and numbness
- Yearning and searching
- Disorganization and despair
- Some degree of reorganization
Patients’ experiences of grief are determined by their values, cultural norms, physical and emotional coping resources, current life stresses, personality, and circumstances. In uncomplicated grief, an individual is able to move through the stages and emerge from the grieving process. Complicated grief (also called chronic grief or dysfunctional grief) is an exaggeration of the normal process of grieving, often resulting from multiple losses and making it difficult for an individual to reorganize and move on.
The dying patient and the family may also experience anticipatory grief, a process of working through their intellectual, behavioral, and emotional responses to what the expected death will mean when it happens. During this process, families often try to resolve personal and family issues, offer love and support, involve the dying person in plans for a memorial service, and determine any last wishes not yet spelled out in a legal document. Adaptive grief is when the reality of death is starting to be accepted (Harding et al., 2023).
(See also “The Family’s Bereavement” later in this course.)
Religion and Spirituality in End-of-Life Care
National and international palliative care guidelines acknowledge the importance of religion and spirituality in illness, particularly at the end of life, and support care that attends to the spiritual needs of patients. Spirituality may be part of an established religious belief or a more personal practice.
Spiritual well-being has been shown to affect the coping mechanisms and quality of life of dying patients. Strong spiritual well-being significantly reduces depression and hopelessness at the end of life. The greater their self-reported religious beliefs, the more optimistic individuals are in their perceptions of outcomes, including greater confidence in treatment efficacy.
It is vital that all members of the healthcare team learn culturally competent practices regarding religion and spirituality in end-of-life care and elicit the patient’s expectations and preferences for the end of their life. Many healthcare decisions, such as whether to withdraw or withhold life-sustaining treatment, to palliate symptoms, or to initiate terminal sedation, require consideration of a patient’s religion and beliefs.
Perceived or real, barriers to performing end-of-life rituals of religious significance can have negative and enduring repercussions that are significant when such spiritual needs go unrecognized by health professionals. Research has found that patients may believe their faith helps them cope with impending death and that practices such as prayer, both alone and with others, are meaningful.
People’s spiritual beliefs may change at the end of life as they consider unresolved issues that may cause spiritual distress. They may believe that the trajectory of their lives is the plan of a supreme creator. They may feel that their religion/spirituality transforms how they experience their illness and the end of life, and they often depend on support from their faith community.
EXAMPLES OF SPIRITUAL NEEDS
The spiritual needs of patients receiving hospice or palliative care can include:
- Connecting with the faith and practices of their religion
- Understanding what gives their life meaning
- Exploring how they wish to be remembered
- Asking for forgiveness for themselves
- Offering forgiveness to others
- Sharing their life story
(Crossroads, 2025)
Religious and spiritual beliefs and practices are highly individual, although research shows some similarities among those of particular racial/ethnic groups.
- Black people are more likely to consider religion/spirituality as important compared to White people.
- Some South Asian religious faiths believe that prolonging the dying process and interfering with clarity of consciousness should be avoided.
- Chinese death rituals honor elders, and the spiritual practice will depend on the age of the deceased.
- Native American death rituals help the spirit leave the body.
- Muslims believe that death marks the transition from one life to another and that the treatment of terminal pain is permissible under the distinction of intended actions.
- Burials are intended to occur very soon after death in the Muslim and Jewish communities.
(Applebury, 2022)
Family Caregiver Burdens
Family caregivers, partners, and close friends make up a “shadow workforce” that bears an enormous burden during end-of-life care of a loved one. They play a major role in actual patient care and in decision-making about care provided by others. Wider informal caregiver networks also help ease the multiple burdens placed on primary caregivers. This may include other family members, church groups, neighbors, or volunteer respite workers.
Access to support services for family caregivers may improve the quality of life for the patient, but despite the multitude of available resources, family caregivers of those with chronic disease continually underutilize such services to cope with the demands of caregiving. Therefore, healthcare professionals should be aware of some common burdens of family caregiving when communicating and interacting with the family.
One in five family caregivers at the end of life undergo a significant burden, usually exacerbated by the duration of care needed or the degree of the patient’s level of dependence. Many organizations and online resources are available for dying patients and their families that can provide information and support. It is imperative for healthcare workers to familiarize themselves with these resources and direct patients and families on how to access them (Bijnsdorp et al., 2022). (See also “Resources” at the end of this course.)
TIME AND LOGISTICS
Caring for a spouse or other family member with serious chronic illness or disability is time-consuming and demanding. Whether caregiving takes a few hours per week or 24 hours a day, the responsibility is continuous. Coordinating medications, treatments, and social services and possibly tending to the needs of other family members can be overwhelming and exhausting, causing caregiver burnout.
There are a multitude of support services available to family caregivers that are underutilized likely because they do not self-identify as caregivers and do not recognize the need for respite care or other services. Conversely, when an individual recognizes that they are experiencing burnout, they are more apt to determine what services may help them and to practice self-care (Bijnsdorp et al., 2022).
PHYSICAL TASKS
The majority of family caregivers are middle-aged or older women who may not have the training or physical stamina necessary to lift, move, or turn terminally ill loved ones. Without professional help, they risk physical injury. Caregivers experience more physical injury than noncaregivers. The most common physical complaints of caregivers are pain, particularly headaches and back pain. Clinicians should anticipate this risk and offer assistance with physically strenuous aspects of care (Bijnsdorp et al., 2022).
FINANCIAL COSTS
The financial burden caused by the cost of terminal care is problematic for many patients and families at the end of life. Although the majority of costs typically relate to medical expenses, other costs may include legal services, transportation, insurance payments, financial planning, and funeral expenses. Even though the Medicare hospice benefit may relieve some of the financial burden of serious illness, families can still face severe economic consequences. Many caregivers must give up their paying job and lose wages and benefits or make major life changes in order to care for their loved one. In our society, a large number of caregivers are African Americans and Hispanic Americans, who generally face greater economic hardship from caregiving.
To address this, in some states, cities, and counties, family caregivers are able to apply for some payment for providing in-home supportive services (CDSS, 2025). Other possible means to help include reducing out-of-pocket costs by applying to drug companies for assistance with the cost of prescriptions, using legal aid services, seeking debt management counseling, and obtaining help from charitable organizations (Bijnsdorp et al., 2022).
MENTAL AND PHYSICAL HEALTH RISKS
Caregivers experience many emotions, ranging from sadness, resentment, anger, and a sense of inadequacy to deep gratitude for being able to care for the loved one. Physical exhaustion, economic worries, disrupted routines, and seemingly endless responsibilities can lead to mental health problems such as anxiety and depression. Inadequate or interrupted sleep is also common among caregivers, as is loss of social and leisure time.
Caregiver physical deterioration may also be exacerbated by caregivers failing to take the time to have their own medical issues treated. Health problems related to caregiving are most pronounced among women and those with limited education and can include increased risk of cancer as well as increased mortality, particularly among older adults. Increased stress in caregivers can be overwhelming and may result in abusive behavior toward an older patient. Referring the patient for respite care can offer caregivers much needed relief and time to take care of themselves (Bijnsdorp et al., 2022).
SUPPORT AND EDUCATION FOR CAREGIVERS
Various programs and interventions have been developed to assist family caregivers to cope with the demands of caregiving. These support services include assistance with caregiving or related tasks and emotional or educational support for family caregivers by health professionals and community service providers. Some examples of support services include information and referral, education, support groups, counseling, crisis intervention hotlines, and problem-solving training. One such educational program is the Resources Enhancing All Caregivers Health (REACH) in the Veterans Administration (VA) (Bijnsdorp et al., 2022; U.S. DVA, 2024).
The negative health effects of caregiving can be at least partially alleviated by thorough assessment of caregiver needs, leading to a care plan with support services. Respite care, caregiver support groups, and skills-training interventions can further reduce caregiver burden.
END-OF-LIFE CARE FOR SPECIAL POPULATIONS
Patients in need of end-of-life care present a diverse group in terms of concurrent illnesses, age, and social attributes.
- Those with cancer comprise a large percentage of the dying patient population. Some of their greatest concerns at the end of life are loss of systemic function, abnormal hematological measurement, anorexia, cachexia, hypercalcemia, and pleural effusion.
- Patients with dementia may experience problems with pain management and the continued need for nutrition and hydration.
- Dying children and their families face unique challenges related to pain management, the need for therapeutic communication with family members, legal and financial issues, and support around bereavement.
- Patients with HIV/AIDS, veterans, and people with homelessness are other groups with special end-of-life care considerations.
The Patient Who Has Cancer
When it has been determined that a patient’s cancer is no longer treatable by members of the healthcare team, the priority becomes improving their quality of life and that of their loved ones and making them comfortable.
Deaths due to cancer in the United States were estimated to be 618,120 in 2025. Deaths due to cancer are highest among those with cancer of the lung (20%), colon and rectum (9%), pancreas (8%), breast (7%), and other types (56%) (NCI, 2025).
Aggressive end-of-life care is considered to be chemotherapy within the last two weeks of life, an emergency room visit or hospital or ICU admission within 30 days of death, or admission to hospice only within the last few days of life. Approximately 45% of terminal patients experience some form of aggressive therapy, especially emergency department visits that then result in admission to the hospital. Although hospice use is increasing, most cancer patients are still entering hospice care just days before death (Friedman, 2025).
Aggressive end-of-life care may not be in keeping with a patient’s stated preferences. Earlier enactment of palliative care and better communication with patients are considered essential to improving end-of-life care. Therefore, education for healthcare practitioners about the end-of-life care options for patients and their families is needed so that providers can offer information about possible alternatives to aggressive treatment.
Early enactment of palliative care per physician’s orders varies according to diagnosis. One study showed that early enactment of palliative care for patients with prostate cancer (5.32%) is less than in patients with pancreatic cancer (17.26%). And despite increasing rates of early enactment, it is still considered underutilized (Friedman, 2025).
People with terminal cancer have the same physical and emotional needs as any dying person, not the least of which is pain management and its side effects. Not every person with terminal cancer experiences excruciating pain, but it is common. Other physical needs arise as the disease progresses, affecting all major body systems, and should be managed based on the goals of patient comfort and quality of life.
The person with advanced cancer also faces special problems. They may be suffering the effects of chemotherapy and radiation therapy. A recent study showed that people with very late chemotherapy use, very short hospice enrollment, and repeated hospitalization were considered to have poor end-of-life experiences by oncologists. More recently, cancer patients have been offered the opportunity to receive palliative care and still undergo treatment, which had not been possible in the past. This may be true for Medicare patients as well. The palliative care can be conducted via Telehealth (Friedman, 2025).
Healthcare professionals must discuss these issues with the patient and family so they are prepared for the time ahead.
DISRUPTION OF FUNCTION
As cancer metastasizes to liver, lungs, bone marrow, brain, bowel, or adrenal glands, it disrupts the function of those organs. For example:
- Liver metastases can impair digestion and cause nausea and vomiting.
- Metastases to the bowel can interfere with elimination, even to the point of fecal impaction.
- Brain tumors increase intracranial pressure as they grow and can cause changes in mental status, vomiting, headache, dizziness, and seizures.
- Growth of metastatic breast, lung, or prostate cancer may compress the spinal cord and lead to irreversible paraplegia if not treated by radiation to shrink the tumor.
Decisions concerning whether and how to treat these complications should involve the patient and the family as well as clinicians.
ANEMIA
Most people with cancer are at least mildly anemic, but chemotherapy and radiation therapy can exacerbate the problem.
Erythropoietin (Epogen) has been used to treat anemia by stimulating the bone marrow to produce more red blood cells; however in 2010, the Food and Drug Administration issued a safety announcement indicating that the use of Epogen and other erythropoiesis-stimulating agents (ESAs) such as Procrit, Retacrit, and Aranesp can increase the risk of cancerous tumor growth and shorten life expectancy in patients with cancer. Therefore, blood transfusions may be used to treat anemia in patients with cancer.
ESAs may be offered to patients with chemotherapy-associated anemia whose cancer treatment is not curative in intent and whose hemoglobin (HgB) has declined to <10 g/dL. The most common side effects of ESAs are hypertension (24%), headache (17%), joint or muscle pain (16%), mild fever (10%), nausea (9%), cough (6%), and edema (5%). More severe and potentially fatal side effects may occur, such as blood clots, MI, or CVA (Kingsly Clinic, 2025).
In patients with myeloma, non-Hodgkin lymphoma, or chronic lymphocytic leukemia, clinicians should observe the hematologic response to cancer treatment before considering an ESA. Before offering an ESA, clinicians should conduct an appropriate history, physical examination, and diagnostic tests to identify alternative causes of anemia aside from chemotherapy or an underlying hematopoietic malignancy (Schoener & Borger, 2024).
A medication guide explaining the risks and benefits of ESAs must be provided to all patients receiving ESAs. Only hospitals and healthcare professionals who have enrolled in and completed a special training program on ESAs are permitted to prescribe and dispense ESAs to patients with cancer.
ANOREXIA-CACHEXIA
Anorexia is loss of appetite, which may be related to both physiologic and psychological factors. Cachexia is a malnutrition syndrome that includes anorexia; early satiety (feeling of fullness after only a few mouthfuls of food); weight loss; anemia; weakness; and alterations in taste and in metabolism of proteins, lipids, and carbohydrates. Cachexia results in wasting and emaciation and is one of the leading causes of death in cancer patients.
HYPERCALCEMIA
Hypercalcemia is an elevated level of serum calcium and the most common life-threatening metabolic disorder associated with cancer; it occurs in 10% to 20% of cancer patients at any stage of the malignancy.
Some types of cancerous tumors (particularly lung and breast tumors and multiple myeloma) as well as bone metastases produce a protein that acts as excess amounts of parathyroid hormone. When serum calcium levels exceed the kidneys’ ability to excrete the excess calcium, nausea and vomiting, constipation, muscle weakness, and dysrhythmias result. Diagnosis and timely interventions can be lifesaving in the short term and may improve the patient’s compliance with primary and supportive treatments as well as improve quality of life.
Untreated hypercalcemia leads to loss of consciousness, coma, and death. Depending on the therapeutic goals determined by the patient, the family, and the responsible clinicians, this course of events may represent a preferred timing or mode of death when compared with a more prolonged death from advancing metastatic disease. It is important to consider this option long before the onset of hypercalcemia or other metabolic abnormalities that impair cognition so that the patient is involved in the decision-making (Canadian Cancer Society, 2025).
PLEURAL EFFUSION
Pleural effusion is the accumulation of fluid in the pleural space, which can cause pain and difficult breathing. Thoracentesis (needle aspiration) to drain the fluid, which may be a liter or more, relieves the pain and facilitates breathing.
The Patient Who Has Dementia
The requirements for dementia patients to be admitted to hospice are the same as for other patients: a physician’s signed opinion that the patient has less than six months to live.
Near the end of life, dementia patients may experience agitation, eating problems, breathlessness, psychosis, depression, and delirium that may require judicious use of psychopharmacology. Psychiatric management for such patients fits well with palliative care. Cross-training mental health with palliative care nurses improves the delivery of care and outcomes for dementia patients. The palliative care approach emphasizes relieving suffering. Applying this philosophy to advanced dementia acknowledges that the patient has a limited life expectancy and is not likely to benefit from an aggressive approach to comorbid conditions.
Decisions about end-of-life care for people with Alzheimer’s disease or other dementias should be made as soon as possible after diagnosis while the patient is able to express personal wishes and participate in decisions.
Referral to the local chapter of the Alzheimer’s Association can help families find attorneys who specialize in elder law or estate planning. This referral should not be made abruptly but as a suggestion, emphasizing that every adult, regardless of health status, should make such a plan. This helps ensure that an individual’s wishes are respected in end-of-life care and in the disposition of property after death. Otherwise, families will need to make difficult decisions without knowing the patient’s wishes. Care must be taken to ensure that those involved in elder law and estate planning are well-informed and honest (Alzheimer’s Association, 2025).
SELECTING A HOSPICE PROVIDER FOR PATIENTS WITH ALZHEIMER’S
When selecting a hospice provider, patients can be counseled to ask these questions:
- Does the provider have a 24/7 call line for unscheduled visits?
- Has the staff provided hospice care to other patients with Alzheimer's?
- What is the program’s (1–5) star rating?
- Does the hospice offer specialized services to improve the patient's comfort?
- Is this hospice program Medicare certified?
(Wolters, 2024)
PAIN MANAGEMENT
Chronic pain is as prevalent among people with dementia (almost half) as among older adults in general. Patients often experience pain but may only be able to communicate this through behavioral changes such as uncharacteristic irritability or withdrawal, increased vital signs, and pained facial expressions. Failure to detect pain is especially apparent among those with severe cognitive impairment. Patients with dementia may not always be able to verbally communicate their pain. Verbal and visual self-report scales; face pictures; and bedside observation of posture, guarding, facial expressions, and behavior during usual activities may indicate an increase in the pain level (Harding et al., 2023).
NUTRITION AND HYDRATION
In the late stages of dementia, patients may become unable to consume enough orally to prevent weight loss. This may be related to poor swallowing (dysphagia), pain, lack of appetite, and a choking cough after eating. Late-stage dementia patients lose significant amounts of body weight. When the patient loses the ability to swallow, they are considered terminal. This is a normal occurrence in the final stages of Alzheimer’s disease. Most patients with advanced dementia have a low metabolic rate due to physical inactivity. If they are maintaining a constant body weight, this rules out starvation and any medical indication for tube feeding. Weight loss can affect the immune system and make it more difficult for the patient to fight disease (Alzheimer’s Society, 2022).
If the patient’s advance directive indicates that they do not want artificial nutrition and hydration (ANH), caregivers and health professionals must respect that decision. However, if the decision was not made earlier, the patient’s surrogate or proxy decision maker, together with the physician and other members of the healthcare team, must decide whether to initiate tube feedings. When nurses and other healthcare practitioners are well-informed about ANH issues, they are able to guide family members who have to make decisions for their older relative with dementia.
Families of people with advanced dementia are counseled that their loved ones are unlikely to benefit from tube feeding, either in terms of survival or quality of life. Based on multiple studies in patients with advanced dementia, tube feeding has not been found to improve survival time, reduce mortality risk, or reduce the incidence of pressure ulcers. Additionally, aspiration pneumonia is a risk for patients at the end of life with poor swallow reflexes and a nasal gastric tube (Estrada et al., 2025).
Dying Children and Their Families
Learning that their child has a life-threatening illness and preparing a child for death is one of the most unnatural and difficult events in any parent’s life. Yet each year parents across the United States confront this tragedy, as 50,000 children die from life-threatening conditions: extreme prematurity, severe birth defects and congenital anomalies, cancer, HIV/AIDS, progressive metabolic disorders, and other diseases and disorders.
The overall U.S. infant mortality rate (death occurring before the first birthday, generally from conditions existing at birth) was 5.6 in 1,000 in 2022, and the African American infant mortality rate was nearly double that, at 10.86 per 1,000 in 2022. The reasons for this discrepancy are considered to be access to and utilization of pre- and postnatal care, prenatal screenings, insurance types, nutrition, and more (USA Facts, 2023).
The remarkable resilience of children can make it difficult to predict whether treatment of life-threatening conditions will end in cure or death. More than half a million children in the United States are coping with complex chronic and life-threatening conditions. These children and their families need and deserve palliative care beginning at the time of diagnosis so that treatment is not limited to the disease process itself. This gives families more time to cope with the possibility that their child will die even as they hope for a cure.
If it becomes clear that cure is no longer possible, the child may be able to receive hospice care at home rather than in the hospital. Conveying to the child that they will not be alone as they near the end and that parental support and love will continue even afterward can be most helpful to a dying child (LLS, 2025).
COMFORT CARE AND PAIN MANAGEMENT
Physical care of the child at end of life is focused on comfort, using the least invasive procedures while protecting privacy and dignity. A child with terminal illness has the same physical needs as any seriously ill child, including pain management, regular sleep and rest, nutrition, maintenance of bowel and bladder function, good respiratory function, and skin care. Additionally, several studies have shown a high degree of symptom burden in children with terminal illness in the last few weeks of life. These symptoms include pain, dyspnea, fatigue, lack of appetite, nausea and vomiting, constipation, and changes in sleep patterns (Vitas Healthcare, n.d.).
Children who are dying share the same fear of pain as adults with terminal illness. Infants are believed to be even more sensitive to pain due to underdeveloped inhibitory pain tracts (Vitas Healthcare, n.d.). Care providers must talk with the family about pain management before the need becomes severe.
For most children, pain control can be achieved using standard dosing with medications such as opioids and benzodiazepines (Vitas Healthcare, n.d.). Families who express concerns about addiction from narcotic pain medication need to be reassured that there is no evidence to support the idea. Like adults, children may develop a tolerance to sedatives and opioid medications, so the dosage or the choice of drugs may need to be changed.
Parents are also greatly concerned that their child does not suffer at the end of life. When pain or other symptoms are not treated or are treated unsuccessfully in their dying child, parents are likely to experience long-term distress.
COMMUNICATION WITH PARENTS
Parents of children who have life-threatening conditions want to be kept informed about their child’s condition and what to expect throughout the course of the illness. They may also want information about caring for their child at home and about how to support siblings of the ill child.
Effective, timely, understandable, and sensitive communication is essential in all aspects of children’s palliative care. Effective communication leads to improved trust among the patient, their family, and healthcare professionals. Linguistic, religious, economic, and cultural differences may prove especially challenging in pediatric palliative care. Limitations in time and staffing as well as inadequate education can also be barriers to good communication. These issues can interfere with parents’ ability to participate fully in their child’s care and contribute to frustration, anger, and sadness for parents long after their child’s death.
Therefore, healthcare practitioners need to ensure that all parents receive clear, factual information and that the family can understand and respond to questions and emotional concerns. This fosters trust in the relationship and reduces distress and anxiety in the parents and family. Shared decision-making with healthcare providers relieves the burden on children and families who may not understand all of the choices available. Shared decision-making includes attention to cultural and community norms, religious beliefs, impact on siblings and extended family, and prior experience with death (Linebarger et al., 2022).
END-OF-LIFE ISSUES FOR INFANTS
Advances in medicine, surgery, technology, and skilled nursing care have improved the survival of premature and other high-risk infants in the United States. However, sometimes the very best care and the strongest hopes and prayers are not enough to save these lives.
The child who dies before the age of 1 year will likely have been hospitalized for much of their life. The challenge for healthcare professionals is to make that time as comfortable and meaningful as possible for the infant and the family, supporting their need to be together, to touch each other, to create shared memories, and to prepare for the loss ahead. For instance, taking photographs of the infant with family members is important, particularly for those parents whose infant will never get to go home with them.
Parents generally seek a healthcare provider who can provide an overview on the infant’s condition every day. This helps avoid misunderstandings from fragmentary information. Parents need to know that it is okay to ask questions and expect honest, understandable answers about what is going on. Other children in the family as well as the grandparents and extended family members also need to be involved.
COMMUNICATING WITH CHILDREN
It is essential to be honest when discussing end-of-life issues with a child but also to refrain from scaring the child (LLS, 2025). The first consideration is to determine the appropriate developmental level of the child for ideal communication. Successful communication with a child may increase cooperation, decrease anxiety, and normalize discussions. Independence and control are an important part of what is communicated to the child, at an appropriate level. Effective communication with the dying child and the family recognizes interpersonal boundaries and is demonstrated as competent, thoughtful, and caring (Nationwide Children’s, 2025).
It is important for the dying child and the family to talk about death with each other, although it can be difficult and painful. Parents may worry that talking about death will cause the child to lose hope and thus the will to live. But keeping the diagnosis secret denies the child’s right to express feelings, fears, and questions. Children pick up cues from parental and sibling behavior that something bad is going to happen, and they need to express their feelings.
There is documented evidence that all patients, even very young children, know they are dying and that they are able to recognize the exceptional distress among family and caregivers around them when death becomes close. By age 6, children begin to recognize the fact of death and what it means. By age 10, children know that death is final. References to its imminence can be quite direct and explicit. Most pediatric patients can tell when adults are having difficulty talking to them about end-of-life issues, death, and dying, and they begin to feel isolated and alienated. If an open and honest dialogue has been established from the beginning, it will be reflected in the willingness of the child or adolescent to talk about fears regarding death (LLS, 2025).
Keeping the diagnosis secret also risks having someone else reveal the information, eroding the child’s trust in the parents. Healthcare professionals can offer support and guidance to the parents by asking, “How will you tell your child the diagnosis?” and then suggesting how and what to say based on the child’s age. Naming the illness helps explain what to expect in terms of procedures and possible outcomes. Once the child learns the diagnosis, they may choose not to talk about death. Parents and healthcare professionals must respect that wish.
Communicating with children about death involves more than just words. It is important to ask the child questions about what they understand and what they are feeling. Reassurances are given that all their feelings are acceptable, even sadness, anger, and tears (LLS, 2025). Healthcare professionals can assess the child’s body language and encourage expressive outlets for feelings, such as drawing; play with dolls, puppets, or stuffed animals; writing stories; or working with modeling clay.
Children with a terminal illness also still enjoy age-appropriate play activities—games, drawing, coloring, video games, texting, and seeing friends. School-age children who are able to attend classes can be encouraged to do so, using remote-learning platforms, to maintain a sense of normalcy and stay connected with their peer group. Frequent absences are common, but some children want to continue their studies at home as long as possible.
Both the child and the family generally fear what the actual death will be like, particularly whether it will be painful. The child fears dying alone; the family fears not being with the child when death occurs. Having family members nearby enhances the child’s feelings of security and safety. Physical contact—touching, hugging, and holding hands—is comforting and helps the child feel more secure. When parents or siblings need to leave, it helps to tell the child when they will be back.
| Age | Concepts |
|---|---|
| (Stanford School of Medicine, 2025) | |
| Infant |
|
| Older infant |
|
| Toddler/preschool |
|
| School-age |
|
| Teen |
|
CASE
Ryan is a 6-year-old boy with terminal cancer who has been undergoing chemotherapy off and on for the past three years. He is now considered end-stage and is being discharged from the children’s hospital pediatric hematology/oncology (Hem/Onc) unit to go home for hospice care. His oncologist, Hem/Onc nurse, and parents have explained the situation honestly and at a level he can understand, creating an open climate where he feels able to ask any questions or express any concerns.
Ryan is happy to be going home and in knowing that he will not have to come back to the hospital or undergo chemotherapy again. He understands that he will soon die and believes he will go to heaven and be able to “look down” on his family and friends. He tells his primary nurse good-bye and thanks her. He has told his parents he is afraid of being alone when “dead comes,” and they have reassured him that someone from his family will be with him at all times. A nonprofit organization in his hometown that provides funds to families with catastrophic illnesses offers his family support so at least one of Ryan’s parents can stay home from work each day to be with him.
DECISION-MAKING
The legal responsibility for decisions about a child’s treatment rests with parents. However, clinicians should encourage parents to involve the child in decisions about continuing treatment aimed either at cure or at moving to palliative care. Adolescents may have very definite ideas about the course their treatment should take.
Both the child and the family must understand what palliative care means, for example, the risks as well as the potential benefit of CPR. Clinicians should explain that palliative care does not mean “no care” but a kind of care aimed at comfort, pain management (if indicated), and maximum enjoyment of the time they have left together.
FINANCIAL ISSUES
Children may qualify for payments for hospice if they meet the eligibility requirements for Medicaid under the Affordable Care Act (ACA) or for the Children’s Health Insurance Program (CHIP). They must also have a physician certify that they have less than six months to live, just as with dying adult patients (Stone et al., 2022).
Medicaid, a jointly funded federal–state health insurance program for people who need financial assistance for medical expenses, must also provide home care services to people who receive federal income assistance such as Temporary Assistance to Needy Families (U.S. DHHS, 2024). Medicaid coverage includes part-time nursing, home care aide services, and medical supplies and equipment. Information about coverage is available from local or state welfare offices, state health departments, state social services agencies, or the state Medicaid office.
BEREAVEMENT
Bereavement begins in the period before the child dies in the form of anticipatory grief and extends well beyond the time of death. Care of the family should extend into the bereavement period. Hospice generally offers support to bereaved family members for a year after the death of the patient. However, if the child dies in the hospital, there may not be a formal bereavement care program available.
(See also “Grief” earlier in this course and “The Family’s Bereavement” later in this course.)
Veterans
Most veterans die either at home, in a nursing home or assisted-living facility, or in a residential hospice. Veterans may receive hospice care through the Veterans Administration (VA). The VA may purchase hospice services from community providers to provide care in the home, a hospital, or a long-term care facility.
Veterans benefits include palliative care and hospice care, but some veterans may not know about or understand these benefits. All VA facilities have a palliative care consult team (PCCT) as a resource for hospice and palliative care provided in the VA facility and coordinated in the community. Although local VA medical centers have the flexibility to address end-of-life care according to veterans’ needs, national policy and standards stipulate that each VA facility have the following resources and services:
- A designated hospice contact person who is part of an integrated network for local and national communications and information dissemination
- Provision of needed hospice services in all settings
- Inpatient hospice beds or access to them in the community
- An interdisciplinary palliative care consultation team
- Assistance with referrals to community hospices in its service area
- Tracking of hospice and palliative care services provided to veterans in all settings
(CaringInfo, 2025)
Veterans dying in the VA system may have a higher degree of social isolation, lack of family support, or lower income than those outside the system. In addition, military training may have created in them an attitude of stoicism and a barrier to admitting pain or requesting pain medication. On the other hand, being in a hospice with other veterans offers a camaraderie that can be comforting.
Showing respect for a veteran and acknowledging service to the country is a first step in establishing a relationship. Simply asking, “What branch of the service were you in?” can be a key assessment question. Other factors that influence experiences at the end of a veteran’s life include age, whether enlisted or drafted, rank, and combat or POW experience (We Honor Veterans, 2025).
Patients with Homelessness
Providing palliative or hospice care for the homeless population provides special challenges to ensuring comfort and quality of life.
For such patients with cancer, the first place in the healthcare system where they may appear with symptoms is often the emergency department (ED). Their cancer may be in the late stages at this time. Due to the difficulties of homelessness and their less-likely access to healthcare, people who are unhoused for long periods of time have a life expectancy of 10 to 20 years fewer than otherwise would be expected.
Homeless patients with cancer have a large symptom burden at the end of life that includes pain, worry, sadness, and exhaustion. Mistrust of the healthcare system, fear of stigma, discrimination, and perceived healthcare prejudice may exacerbate this burden if it prevents such patients from seeking care. One of the biggest challenges in bringing hospice care to this population is that their homelessness makes it difficult to provide care to them (Coverdale & Murtagh, 2024; Mirasol Health, 2024).
In 2018, the National Health Care for the Homeless (HCH) Clinicians’ Network developed recommendations on providing palliative and hospice care to patients experiencing homelessness. Examples include practicing trauma-informed care; employing a harm-reduction philosophy regarding addiction, placements, and medication adherence; encouraging shelters to permit daytime rest, secure locations for controlled medications, and other special accommodations; considering transfer to inpatient hospice for severe symptom management; and more (NHCHC, 2025).
The Patient Who Has HIV/AIDS
In 2022 in the United States, there were an estimated 38,043 newly diagnosed people ages 13 and older with HIV infection and nearly 19,310 deaths among those with HIV infection (CDC, 2024b).
More effective treatments for HIV/AIDS and for opportunistic infections have made the disease trajectory far less predictable. This has increased the difficulty of making decisions about advance care and end-of-life issues. Although patients with HIV/AIDS agree that advance care planning is important to clarify end-of-life issues, most stated that they have not signed advance directives and that their families were not aware of their wishes.
Older adults with AIDS may develop multiple medical conditions. In advanced AIDS, the patient may experience both the late effects of the disease itself as well as treatment-related toxic effects. The combined effects include fatigue, weakness, memory loss, and continuous diarrhea, which together necessitate around-the-clock care. If family or friends are unavailable to provide care, the services of home health aides are required. These aides must be informed about whether the patient has a DNAR order in effect and whether the patient wishes to be hospitalized.
The person living with advanced AIDS has some of the same psychosocial concerns as patients with any terminal illness, including financial issues, bereavement issues, and fear of death. In addition, the individual may have unique issues related to HIV/AIDS, which can include:
- Stigmatization related to HIV/AIDS
- Fear of contagion
- Fear of social isolation
- Poor quality of treatment due to refusal of care by healthcare providers
- Fear of being judged negatively
- Fear of disclosure of one’s HIV status
- Delayed access to care
(UNAIDS, 2024)
Many lack the traditional support systems of friends and families. Friends may be HIV-infected themselves. Others may be afraid of contagion, based on ignorance about HIV transmission or unresolved homophobia. Families may live far away, since many people with AIDS have migrated to large urban areas that are more tolerant of nontraditional lifestyles, perhaps leaving them without a support system or socially isolated when their disease progresses. Persons may lose their jobs or not be able to obtain other work.
One-on-one counseling or a grief support group can help the bereaved patient and afford an opportunity for caregivers to discuss their own concerns and fears about the death of a friend or loved one.
DEATH OF THE PATIENT
The Final Hours
Care during the last hours of life, called active dying, can have profound effects on the patient, the family, and healthcare practitioners who attend the dying. Any distressing symptoms that the dying patient has been facing may become exacerbated when death is imminent. Therefore, in acute care, multidisciplinary healthcare professionals must transition from curative to comfort care. Comfort care provides symptom management for a patient who is actively dying.
Consideration is given to every aspect of care to determine whether the benefits are enough to outweigh the risks of discomfort. A plan of care is usually established by the patient or family and healthcare personnel to determine when to withdraw or avoid life-sustaining measures such as oxygen, diagnostic tests like painful blood tests, or nutrition and hydration, and which comfort measures to provide (Harding et al., 2023). For example:
- Vital signs may be taken every 24 hours or not at all during comfort care. If an abnormal blood pressure is not to be treated, the risk of causing arm pain outweighs taking the measurement. Conversely, a fever can cause severe discomfort. Hot skin may be sufficient to justify giving the dying patient acetaminophen, by rectum if needed.
- Artificial tears or drops of normal saline given every one to two hours will prevent pain from dry corneas when the eyelids remain open.
- Frequent oral hygiene with swabs prevents the discomfort of a dry mouth.
These comfort measures can be performed by a nursing assistant, except the artificial tears, which may be considered a medication requiring administration by a nurse.
SIGNS ANDS SYMPTOMS WHEN DEATH IS NEAR
Certain signs and symptoms indicate when death is near. Not every patient experiences each of these signs and symptoms, and the presence of one or more of these symptoms does not necessarily indicate that the patient is close to death. The final stage of dying may take from 24 hours to as long as 10 to 14 days.
When it is apparent that death is imminent, health professionals alert the family and confirm the goals of care. This discussion is documented in the patient’s chart, including the observation that the patient is dying.
Pain
Pain is typically the most feared symptom of dying. It can be aggravated by physical or emotional stressors. Care may include:
- Regularly assessing for severity, quality, location, and contributing and relieving factors
- Minimizing irritants such as moisture, pressure, and temperature extremes
- Administering pain medications around the clock (to prevent pain rather than treat it)
- Providing alternative comfort measures (e.g., massage, distraction, heat, repositioning)
- Including family and other visitors in comfort measures
Delirium
Delirium is a state of mind that includes confusion, restlessness, incoherence, anxiety, and often hallucinations. Care may include:
- Assessing for reversible causes
- Reorienting patient to person, place, and time with every encounter
- Providing a patient room that is quiet and well-lighted
- Medicating with benzodiazepines or other sedation as needed
- When working with the patient, staying physically close and speaking in a calm, reassuring voice
Anxiety/Restlessness
Anxiety and restlessness may increase as death becomes imminent, as evidenced by tachycardia, dyspnea, and diaphoresis. Care may include:
- Assessing for possible causes (e.g., spiritual distress, urinary retention, constipation)
- Avoiding use of restraints
- Using soft music, low lights, calm voice, and soft touch
- Limiting visitors at the bedside
Dysphagia
Patients near death may experience difficulty swallowing, with a high risk of aspiration. Care may include:
- Administering medications through routes other than oral (rectal, buccal, transdermal); discontinuing any medications that are not necessary
- Suctioning orally as needed
- Providing a modified diet (e.g., ice chips, thick liquids)
- Elevating the head during hand-fed meals or liquids and for at least 30 minutes after meals
- Considering the possibility of aspiration
Weakness/Fatigue
This may be caused by increased metabolic demands. Care may include:
- Bundling nursing activities to conserve energy
- Limiting activities to those most valued by the patient
- Providing frequent rest periods
Dehydration
This may be caused by decreased thirst and hunger at the end of life. Care may include:
- Assessing mucous membranes for dryness
- Providing frequent oral hygiene via swabs
- Using ice chips and sips of fluid, if able
- Applying lubricant to lips
- Reassuring family that the loss of hunger and thirst are natural and not dangerous at the end of life
Dyspnea
Shortness of breath may be accompanied by subjective feelings of suffocation or anxiety. Care may include:
- Elevating the head of the bed
- Having a fan blowing on the patient to move the air in the room
- Teaching the patient pursed-lip breathing
- Providing oxygen and suction as needed
- Administering medications (e.g., inhalers or expectorants)
Myoclonus
Myoclonus, or mild to severe twitching, may be caused by high opioid dosing. Care may include:
- Reducing opioid dose to alleviate discomfort
- Medicating with muscle relaxants (which may cause sedation)
Pressure Injuries
Pressure injuries may be worse at the end of life due to incontinence and poor nutritional intake. Care may include:
- Turning the patient every 2 hours if the patient is unable to move themself
- Keeping skin dry and clean
- Providing wound care, as appropriate
- Providing blankets for warmth, but avoiding applying heat
- Preventing pressure on the skin due to shearing
Incontinence
Constipation may be caused by immobility and opioids. Diarrhea and urinary incontinence may be caused by relaxation of muscles. Care may include:
- Administering suppositories, stool softeners, laxatives, or enemas, if ordered and appropriate
- Using absorbent pads for urinary incontinence
- Considering the application of a condom catheter for men or an external wicking catheter for women
- Preventing skin irritation or pressure injuries that may result from the presence of stool or urine on the skin for prolonged periods
Anorexia/Nausea/Vomiting
This may be caused by the disease process, medications, or constipation. Care may include:
- Assessing for possible causes
- Medicating appropriately for symptoms
- Providing frequent mouth care, especially after vomiting
(Harding et al., 2023)
SIGNS OF DEATH
Signs that death has occurred include:
- Lack of respiration or pulse
- Eyes open but do not move or blink; pupils dilated
- Jaw relaxed, mouth slightly open
- Bowel and bladder contents expelled
- Patient does not respond to touch or speech
- Skin color becomes pale and waxen in appearance
- Body temperature drops
- Sound of internal fluids trickling or gurgling
(Harding et al., 2023)
When death has occurred, nurses or other clinicians express their sympathy to the family. It is enough to say, “I am sorry for your loss.”
CASE
Agnes, an older adult, had been discharged from the hospital to her home to spend her last days in comfortable, familiar surroundings, per her written wishes. Her grandson asked the hospice nurse, “How can we be sure that my grandmother has passed?” The nurse explained that the breathing may become slower, shallow, and loud, even sounding like gasping when death is imminent. She showed the grandson where to feel for a radial pulse in the wrist and explained that he would be unable to feel it when the heart stopped beating. The nurse told him that all of the muscles would relax and that this might appear as open eyes, a slack jaw, and incontinence of the bowel and bladder. The skin would become cool, pale, and waxen. When that happened, the grandson was instructed to call the hospice nurse.
Organ Donation
Organ procurement organizations (OPOs) throughout the country facilitate the donor organ recovery process, which increases efficiency and organ yield, reduces costs, and minimizes organ acquisition charges. OPOs have taken on the responsibility of harvesting donor organs and matching them with potential recipients.
In the United States, the growing disparity between organ availability for transplantation and the number of patients in need has challenged the donation and transplantation community. The number of organs available for transplantation has been a relatively fixed national resource over the last decade. By contrast, the national waiting list rises by thousands each year, with only a fraction of those who are waiting receiving lifesaving transplants.
NUMBERS OF TRANSPLANTS
As of 2025, 107,333 people were on the waiting list for a lifesaving organ transplant (total waiting list candidates). In 2024 over 7,000 living people donated a kidney or part of a liver, usually to a relative. Also in 2024, there were more than 17,000 transplants from deceased (formerly termed cadaver) donors. This was the 14th-consecutive record-breaking year (UNOS, 2025).
In 2023, the most commonly transplanted organs were the kidneys (59%), liver (23%), heart (10%), lungs (6%), and dual kidneys/pancreas (2%). The majority of transplants were performed among adults ages 18 through 64 (72%), with a lesser proportion in adults over age 65 (24%) and children under 18 (4%).
| Organ | Cost | Number performed (year) |
|---|---|---|
| (Goodley, 2024) | ||
| Heart | $1.4 mil | 3,817 (2021) |
| Intestines | $1.1 mil | 96 (2021) |
| Bone marrow | $893,000 | 4,276 (2021) |
| Lungs | $862,000 | 2,569 (2021) |
| Liver | $813,000 | 9,234 (2021) |
| Kidney | $415,000 | 42,800 (2022) |
| Pancreas | $408,800 | 962 (2020) |
ORGANS AND TISSUES THAT CAN BE DONATED
One organ donor can save up to eight lives and save or improve an additional 50 lives through tissue donation. Most organ donations come from deceased donors (although a living donor can donate as well). Tissues can also be transplanted. The following table shows what organs and tissues can be donated from deceased donors.
| (Golhar, 2024; HRSA, 2024) | |
| Organs |
|
| Tissues |
|
DISCUSSING ORGAN DONATION
The public has a generally favorable attitude about organ donation for transplants; however, not every clinician broaches the subject with patients out of concern they may be perceived as being more an advocate for the organ recipient than of their patient. Ideally, questions about organ donation are discussed with the patient in the context of advance directives. This relieves the family of making the decision during the stressful time immediately after death. Unless the patient has documented the wish to become an organ donor, the family must decide.
The Anatomical Gift Act was approved by Congress in 1968 following the first heart transplant the previous year. The 2006 United States Revised Anatomical Gift Act compels hospitals and OPOs to pursue donation in cases of brain death in designated donors to stimulate the supply of available organs (USLegal, 2025). Federal law requires that only a “designated requestor” may approach the family about organ donation (see below).
DONATION AFTER BRAIN DEATH
Brain death statutes in the United States differ by state and institution. The Uniform Determination of Death Act (UDDA) of 1981 provides states with whole-brain criterion of death. The UDDA offers two definitions for when an individual may legally be declared dead:
- Irreversible cessation of circulatory and respiratory functions or
- Irreversible cessation of all functions of the entire brain, including the brain stem
When brain death has been confirmed, the hospital notifies the local organ procurement organization. If the patient is a potential donor, an OPO representative immediately goes to the hospital and searches the state’s donor registry for legal consent. If the patient is not registered and there is no other legal consent, consent from the family will be required. When this is obtained, medical evaluation continues (McCall, 2023).
DONATION AFTER CARDIAC DEATH
Anyone who has brain function that has been deemed incompatible with life but who does not meet all criteria for brain death is a potential candidate for donation after cardiac death (DCD). DCD may be discussed as an option with families when they have accepted that their loved one cannot survive and have made the decision to remove that person from life support. There is a 90-minute time frame in which organs can be recovered after extubation to the pronouncement of death. If the patient does not progress to cardiac death within this time, organ donation cannot occur. Tissue donation may still be an option after death.
If the family agrees to DCD, the patient is removed from the ventilator in an operating room. When the heart stops beating, a physician declares death and organs are recovered (Donor Alliance, 2025).
DESIGNATED REQUESTORS
It is a federal regulation that a specially trained, designated hospital staff member, known as a designated requestor, approach the family to discuss the option of organ donation. A designated requestor may be a physician or other healthcare professional who has completed a course approved by an OPO on how to approach potential donor families to request organ or tissue donation. Who this person is varies according to the facility.
The requestor lets the family know the patient is registered to be an organ donor and that those wishes will be carried out after death is pronounced. The family is also given clarification of the definition of brain death and informed that the patient will remain on life support after death is pronounced (Donor Alliance, 2025).
MEDICAL EVALUATION OF POTENTIAL DONORS
Screening of a potential donor is essential to determine whether the donor has an infection that could be transmitted to recipients through transplanted organs or tissues. The Organ Procurement and Transplantation Network (OPTN) policies (for OPOs) and FDA regulations and guidance (for tissue and eye banks) require a medical and social history interview to be conducted with the deceased donor’s next of kin or another knowledgeable person (CDC, 2024c).
Interviews are designed to assess the donor for:
- Risk behaviors that may have exposed the donor to certain diseases
- The donor’s past medical history
- Relevant travel history (which can be important for exposure to certain pathogens)
OPTN policy requires OPOs to perform tests to determine if the donor has certain infections:
- Human immunodeficiency virus (HIV)
- Hepatitis B virus (HBV)
- Hepatitis C virus (HCV)
- Syphilis
- Cytomegalovirus (CMV)
- Epstein Barr virus (EBV)
- Toxoplasmosis
(CDC, 2024c)
Once a potential donor has been evaluated and accepted, additional assessments are done for the donation of specific organs.
MATCHING PROCESS
Following medical evaluation for contraindications, the OPTN is contacted by the OPO in order to begin a search for matching recipients. The OPTN matching process includes:
- Blood type
- Body size
- Severity of patient’s medical condition
- Distance between the donor’s hospital and the patient’s hospital
- Patient’s waiting time
- Whether the patient is available
- Tissue type
(HRSA, 2024)
ORGAN RECOVERY
During the above process, the donor is maintained on artificial support. The condition of every organ is monitored by hospital medical and nursing staff along with the OPO coordinator, who also arranges arrival and departure times of both surgical teams. When the surgical team arrives, the donor is taken to the OR, and under sterile technique, organs and tissues are recovered and all incisions closed. The tissue and organs are then transported rapidly by commercial or contracted airplanes, helicopters, or ambulances to the hospital where the transplant recipient is waiting and may be prepped and ready in the OR (HRSA, 2024).
Postmortem Care
Death must be certified in a formal process called pronouncement and the findings related to cause of death documented in the patient’s medical record. Pronouncement may be done by a physician, nurse practitioner, nursing supervisor, or hospice nurse, depending on state regulations and the policies of the healthcare agency/facility involved. Unless the death occurred under unusual circumstances, an autopsy (postmortem surgical examination) is not usually required.
CARE OF THE BODY
Care of the body after death is often the responsibility of nurses and nursing assistants. How the body is cared for after death is often influenced by religion or culture, so health professionals should be aware of any preferences or limitations and comply with them.
For example, for a Muslim patient, the body is typically washed by family or friends to prepare it for the funeral. The eyes will be closed, the arms will be positioned across the chest, and the body will face Mecca. In the Jewish religion, the eyes are closed and the body is covered, on the floor, and surrounded by lit candles. The body is never left alone. Eating and drinking are not allowed near the body. In Jewish law, being around a dead body causes uncleanliness, so often the washing of the body is carried out by a special group of volunteers (Memory Tree, 2022).
If the family was not present at the time of death, the nurse or other responsible practitioner may make the body and the environment appear as normal as possible for the family to visit. If the patient or family has chosen cremation or if there is no open-casket service planned, this will be the final opportunity for them to see their loved one. All equipment and supplies are removed from the bedside and any soiled linens removed from the room.
Local regulations may differ on actions related to tubes that were in place at the time of death; generally, the coroner must be notified, and no internal tubes can be removed until the patient is cleared by the coroner’s office as not requiring an investigation into the cause of death. Such cases are referred to as a coroner’s clearance. Conversely, coroner’s case refers to instances when an investigation is deemed necessary, as dictated by the county’s policies.
Placing the body in a supine position with a pillow under the head and shoulders avoids discoloration of the face. Eyelids are closed (holding them closed for a few seconds helps them to remain closed). If the person wore dentures, those are inserted to give the face a more natural appearance. Placing a rolled towel under the chin will hold the mouth closed. The arms are positioned either at the sides of the body or across the abdomen. The identifying wristband is left on unless it has become too tight due to fluid retention, in which case it is replaced with a looser one.
Any soiled areas of the body are washed, and absorbent pads are placed under the buttocks. A clean gown is placed on the body, and the hair is brushed or combed. Any jewelry is removed, except for a wedding band, which is taped to the finger. The body is carefully covered up to the shoulders with clean bed linens. All belongings of the deceased are listed and placed in a safe storage area for the family. These measures are usually conducted by a nursing assistant in acute care and always conducted by the nursing assistant in long-term care, as directed by the nurse in charge.
Soft lighting is generally preferred, and chairs and tissues may be made available for family members. Clinicians reassure family members that they may take as much time as they need to say their last good-byes. Only when the family leaves the room should final preparations for removal of the body be initiated.
REMOVING THE BODY
After the family has viewed the body, the care provider attaches additional identification tags, one to the left great toe and one to the patient’s belongings. The entire body is then placed in a white, plastic body bag and another identification tag affixed to the outside zipper. Then the body is either picked up by the responsible mortician (undertaker) or sent to the hospital morgue, if there is one, until arrangements are made with a mortician.
Some hospitals or other agencies close the doors to all other patient rooms before transporting a body through the corridors and require the use of service elevators rather than public elevators during this transfer, if available.
Autopsy
An autopsy is an examination of a body to determine how and why the person died. Autopsies are not performed as frequently as in the past unless the death was suspicious for homicide, suicide, or other questionable circumstances. This is a forensic autopsy done by a forensic pathologist and is ordered by law enforcement, a coroner, or a judge.
A medical autopsy may be performed on someone who died of natural causes when there is a potential benefit such as preventing more deaths, improving medical care, or discovering genetic conditions (Cleveland Clinic, 2025c).
The average number of deaths in U.S. hospitals that result in autopsies is <5%, higher in teaching hospitals. The procedure contributes to medical education, aids in the characterization of newly emerging diseases, and advances the understanding of disease-related changes. In addition, autopsy can reveal errors in clinical diagnosis.
In the event that autopsy is required, health professionals determine whether the family has any religious or cultural concerns about this procedure. Families are also informed that autopsy does not disfigure the body and does not interfere with having an open-casket service.
MEDICAL EXAMINER INQUESTS
Medical examiner inquests are conducted to determine the manner of death, in accordance with state and local laws. For example, the Government Code of the State of California grants the medical examiner of a jurisdiction the authority to hold inquests at their discretion. The code also states that the medical examiner “shall hold an inquest if directed to do so by the Attorney General, district attorney, sheriff, city prosecutor, city attorney, or chief of police of a city in the county of which such coroner has jurisdiction.” These inquests are to be open to the public and, at the discretion of the medical examiner, can be held with or without a jury.
As stipulated by the code, the results of the inquest should yield the name of the deceased; the time and place of death; the medical cause of death; and whether death was the result of natural causes, a suicide, an accident, or a homicide. (A homicide is a death at the hands of another person that is not accidental.) If the chief medical examiner determines that the manner of death is homicide, the medical examiner is required to transmit the written findings to the district attorney, the police in the jurisdiction where the body was recovered, and any other police agency requesting copies of the findings.
Healthcare professionals may wish to research regulations governing medical examiner inquests in their own jurisdiction.
(SFBoS, n.d.)
THE FAMILY’S BEREAVEMENT
A family’s bereavement begins when their loved one is diagnosed with terminal illness, initiating a period of anticipatory grieving for both patient and family. After the patient dies, family members continue to grieve until they become reconciled to life without the deceased. For some, the process may take weeks or months; for others, grieving may take a year or longer. The Medicare hospice benefit includes bereavement care for the family for approximately one year after the patient’s death.
All healthcare practitioners may encounter bereaved persons, and it is important to recognize the signs of grieving and bereavement and offer appropriate support as part of care.
(See also “Grief” earlier in this course.)
Characteristics of Grief and Mourning
How a person grieves depends on their personality, physical and emotional coping patterns, relationship with and attachment to the person who died, cultural beliefs, and the situation surrounding the loss. Grief reactions can be psychological, emotional, physical, or social. Psychological and emotional reactions can include anger, guilt, anxiety, sadness, and despair. Physical reactions can include difficulty sleeping, appetite changes, somatic complaints, or illness. Social reactions can include feelings about taking care of others in the family, the desire to see or not see family or friends, or the desire to return to work (Harding et al., 2023). If the deceased was the primary earner, the family may suffer stress from significant financial loss.
Several authors have given definitions of grief that are now considered classic. For example, DeSpelder and Strickland (1987) identified five characteristics of grief:
- Somatic distress
- Preoccupation with the image of the deceased
- Guilt
- Hostile reactions
- Loss of the usual patterns of conduct
Bowlby (1961) described three phases of mourning:
- Urge to recover the lost person
- Disorganization and despair
- Reorganization
These phases originated from the attachment theory of human behavior, which postulates people’s need to attach to others in order to improve survival and reduce risk of harm.
Lindemann’s classic text (1994) described three tasks of what he called “grief work.” These include:
- Freedom from ties to the deceased
- Readjustment to the environment from which the deceased is missing
- Formation of new relationships
To free oneself from the deceased, a person must change the emotional energy invested in the lost person. This does not mean the deceased was not loved or is forgotten but that the grieving person is able to turn to others for emotional satisfaction. To readjust, the grieving person may need to modify their roles, identity, and skills to live in the world without the deceased. To form new relationships, the person redirects the emotional energy once invested in the deceased to other people and activities.
Grief work requires significant effort, so it is not uncommon for those who grieve also to experience overwhelming fatigue.
When a loved one has experienced a prolonged dying process, some family members not only grieve the loss of that person but also suffer the loss of their role as caregivers. They may experience a sense of relief that the burden of caregiving has lifted as well as guilt for feeling relief. These are natural reactions, and health professionals should encourage their expression.
COMPLICATED GRIEF
Complicated grief (CG) can be experienced after the loss of a loved one and is a prolonged bereavement that interferes with one’s ability to return to the activities undertaken before the death. CG may be diagnosed as a persistent, complex bereavement disorder when it continues indefinitely. The surviving family member or caregiver may show characteristics of shock or being stunned or numb. Extreme symptoms may include extended lack of trust or caring for any other individuals, including other children, and an intense reaction to or avoidance of remembrances of the loved one.
In the United States, approximately 7% to 10% of those experiencing the loss of a loved one suffer CG, and family caregivers of a dying child are the most likely to undergo this. When there is prolonged bereavement after the death of a child, family caregivers, particularly parents, may experience guilt, abandonment, loneliness, and loss of purpose or identity when caregiving ceases (ABCT, 2025).
Grief among Health Professionals
Health professionals who work with dying patients and their families may also grieve when a patient dies even though the death was expected. In the aftermath of the death of a patient, grief counseling in the form of a debriefing may be offered to the involved staff. Attending the funeral or memorial service may allow expression of the grief as well as show respect for the family and their loss.
Bereavement Resources
Bereavement options for families include grief support groups (either self-help or facilitated by professionals) and one-on-one counseling by a psychologist, psychiatrist, clinical social worker, or clergyperson. Many online support groups are also available as an adjunct to in-person therapy rather than as a substitute. If depression occurs in the context of bereavement, medication may be appropriate. No consensus exists among professionals as to the most effective intervention. There are many books and videos available, most of them specifically focused on a particular family role (parents, children, siblings, or spouse).
Hospice professionals who work with the bereaved maintain contact with the family, make home visits, and encourage family members to talk about their feelings, emphasizing that grieving is a painful process that may take years to resolve. It is important to refer to the deceased person by name and to discuss shared memories with the family. Continuing contact with the family offers them an anchor during a difficult time. A good condolence letter offers a tribute to the deceased and comfort to the survivors.
CONCLUSION
The ranks of older adults continue to swell in the United States. Many of them have one or more chronic diseases. Thus, the need for high-quality end-of-life care will only increase. The number of children needing end-of-life care has also risen, causing overtaxed parent caregivers to seek support in the form of bereavement care, respite care, and spiritual guidance.
Americans are beginning to accept that death is inevitable and that planning for end-of-life care is essential to ensuring that one’s preferences are respected when no longer able to care for oneself. More people are drawing up advance directives, appointing a healthcare proxy/agent, choosing hospice and palliative care over aggressive treatments, or considering assisted death. This growing awareness around end-of-life issues would not have come about without the educational and outreach efforts of nurses, other health professionals, public health agencies, and private foundations.
Increasing numbers of dying patients have opted to select palliative care or hospice as an alternative to more aggressive medical care performed in acute care hospitals, often in ICUs. Communication with patients and families is essential to stress that these are a means to make the patient more comfortable rather than “giving up.” Palliative care is mostly noninvasive and focuses on the patient’s comfort. Hospice care is ordered when a physician determines that the patient may have less than six months to live and may be renewed after six months with another physical examination.
There are certain populations that require special consideration when planning hospice and palliative care, such as children. Those with various ethnic differences also have practices that are specific to their culture. Those who care for people in these special circumstances should be aware of the unique needs to provide all dying patients with comfort, pain management, and information specific to what is needed.
Since pain, dehydration, excess secretions, and other symptoms at the end of life may cause discomfort, pharmacologic and nonpharmacologic measures are necessary as a part of care, particularly in the last hours of life, when the patient is considered to be actively dying. After death, specific legal considerations and tasks are performed by physicians, nurses, and nursing assistants as part of postmortem care.
All healthcare professionals have a role in helping their patients and families understand the range of options available and the benefits of planning for end-of-life care before it is needed.
RESOURCES
American Academy of Hospice and Palliative Medicine
Center to Advance Palliative Care
Hospice & Palliative Nurses Association
Medical orders for life-sustaining treatment (MOLST)
National Alliance for Care at Home (NAFCH)
(formerly National Association for Home Care & Hospice and the National Hospice and
Palliative Care Organization)
National Coalition for Hospice and Palliative Care
Pediatric Palliative Care Network
Safe disposal of medicines (U.S. FDA)
REFERENCES
AccentCare. (2022). Open access. https://www.accentcare.com/our-services/hospice-palliative-care/hospice-palliative-services/open-access/
AGAPE Hospice NW. (2025). How long does the average hospice patient live? https://www.agapehospicenw.org/blog/average-hospice-patient-lifespan/
Agingstats.gov. (2024). Older Americans 2024: Key indicators of well-being. https://agingstats.gov/docs/LatestReport/Older-Americans-2024-508-May-update.pdf
Akdeniz M, Yardimci B, & Kavukcu E. (2021). Ethical considerations at the end-of-life care. SAGE Open Medicine, 12(9). https://doi.org/10.1177/20503121211000918
Alzheimer’s Association. (2025). Legal planning. https://www.alz.org/help-support/i-have-alz/plan-for-your-future/legal_planning
Alzheimer’s Society. (2022). Changes in behavior in the later stages of Alzheimer’s. https://www.alzheimers.org.uk/about-dementia/symptoms-and-diagnosis/how-dementia-progresses/changes-in-behaviour-later-stages
American Academy of Hospice and Palliative Care (AAHPC). (2025). Artificial nutrition and hydration near the end of life. https://aahpm.org/advocacy/where-we-stand/anh/
American Association of Colleges of Nursing (AACN). (2024). Nursing shortage fact sheet. https://www.aacnnursing.org/Portals/0/PDFs/Fact-Sheets/Nursing-Shortage-Factsheet.pdf
American Association of Nurse Practitioners (AANP). (2025). Issues at a glance: Provider orders for life-sustaining treatment (POLST). https://www.aanp.org/advocacy/advocacy-resource/policy-briefs/issues-at-a-glance-provider-orders-for-life-sustaining-treatment-polst
American Cancer Society (ACS). (2025). How and where is hospice care provided and how is it paid for? https://www.cancer.org/treatment/end-of-life-care/hospice-care/who-provides-hospice-care.html
American Medical Association (AMA). (2025). Orders not to attempt resuscitation. https://www.ama-assn.org/delivering-care/ethics/orders-not-attempt-resuscitation-dnar
American Nurses Association (ANA). (2025). ANA code of ethics for nurses, with interpretive statements: Provision 1.4 the right to self-determination. https://codeofethics.ana.org/provision-1-4
Anekar AA, Hendrix JM, & Cascella M. (2023). WHO analgesic ladder. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK554435/
Angela Hospice. (2023). Food and fluid issues at the end of life. https://angelahospice.org/wp-content/uploads/2023/09/FoodFluid.pdf
Applebury G. (2022). Different cultural beliefs on death and dying practices. Love to Know. https://dying.lovetoknow.com/death-cultures-around-world/different-cultural-beliefs-death-dying-practices
Association for Behavioral and Cognitive Therapies (ABCT). (2025). What is complicated grief? https://www.abct.org/fact-sheets/complicated-grief/
Bhyan P, Shrestha U, Schoo C, & Goyal A. (2024). Palliative sedation in patients with terminal illness. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK470545/
Bijnsdorp FM, Onwuteaka-Philipsen BD, Boot CR, van der Beek AJ, & Pasman HRW. (2022). Caregiver’s burden at the end of life of their loved one: Insights from a longitudinal qualitative study among working family caregivers. BMC Palliative Care, 21, Article 142. https://doi.org/10.1186/s12904-022-01031-1
BlackDoctor.org (BDO). (2025). Cultural competence in healthcare: Why it matters for Black patients. https://blackdoctor.org/cultural-competence-in-healthcare-why-it-matters-for-black-patients/
Bowlby J. (1961). Processes of mourning. International Journal of Psychoanalysis, 42, 317–40.
Bryan AF, Reich AJ, Norton AC, Campbell ML, Schwartzstein RL, et al. (2024). Process of withdrawal of mechanical ventilation at end of life in the ICU. CHEST Critical Care, 2(3), Article 100051. https://doi.org/10.1016/j.chstcc.2024.100051
Burtka J. (2025). About physician orders for life sustaining treatments (POLST) forms. https://www.nolo.com/legal-encyclopedia/about-physician-orders-life-sustaining-treatment-polst-forms.html
California Department of Social Services (CDSS). (2025). In-home supportive services. https://www.cdss.ca.gov/In-Home-Supportive-Services
Canadian Cancer Society. (2025). High calcium levels (hypercalcemia). https://cancer.ca/en/treatments/side-effects/high-calcium-levels
CaringInfo. (2025). During serious illness, CaringInfo is here to help you make informed decisions about care and services before a crisis. https://www.caringinfo.org/
Celerian Group Services (CGS). (2025). Hospice payment rates calculator. https://www.cgsmedicare.com/medicare_dynamic/hospice_rate_calculator/hospice_rate_calc/index.aspx
Center to Advance Palliative Care (CAPC) and National Palliative Care Research Center (NPCRC). (2024). America’s readiness to meet the needs of people with serious illness: A state-by-state look at palliative care capacity: 2024 serious illness scorecard. https://reportcard.capc.org/
Centers for Disease Control and Prevention (CDC). (2024a). About chronic diseases. https://www.cdc.gov/chronic-disease/about/
Centers for Disease Control and Prevention (CDC). (2024b). HIV surveillance report: Diagnoses, deaths, and prevalence of HIV in the United States and 6 territories and freely associated states, 2022. http://www.cdc.gov/hiv-data/nhss/hiv-diagnoses-deaths-prevalence.html
Centers for Disease Control and Prevention (CDC). (2024c). Clinical guidance for transplant safety. https://www.cdc.gov/transplant-safety/hcp/clinical-guidance/
Centers for Medicare and Medicaid Services (CMS). (n.d.). Medicare hospice benefits. https://www.medicare.gov/publications/02154-medicare-hospice-benefits.pdf
Centers for Medicare and Medicaid Services (CMS). (2025). Hospice monitoring report. https://www.cms.gov/files/document/hospice-monitoring-report-2025.pdf
Cleveland Clinic. (2025a). Palliative care. https://my.clevelandclinic.org/health/articles/22850-palliative-care
Cleveland Clinic. (2025b). Delirium. https://my.clevelandclinic.org/health/diseases/15252-delirium
Cleveland Clinic. (2025c). What is an autopsy. https://my.clevelandclinic.org/health/diagnostics/autopsy
Cleveland Clinic. (2025d). Do-not-resuscitate (DNR). https://my.clevelandclinic.org/health/articles/8866-do-not-resuscitate-orders
Compassion & Choices. (2025). States where medical aid in dying is authorized. https://compassionandchoices.org/resource/states-or-territories-where-medical-aid-in-dying-is-authorized
Coverdale MR & Murtagh F. (2024). Destitute and dying: Interventions and models of palliative and end of life care for homeless adults—A systematic review. BMJ Support Palliative Care, 19(14), e3–241. https://doi.org/10.1136/spcare-2024-004883/
Crossroads. (2025). Spirituality and end-of-life care. https://www.crossroadshospice.com/hospice-resources/spirituality-end-of-life-care/
Davies A. (2025). Clinically assisted nutrition and hydration at the end of life. Clinical Medicine, 25(4), Article 100323. https://doi.org/10.1016/j.clinme.2025.100323
DeSpelder LA & Strickland AL. (1987). The last dance: Encountering death and dying (2nd ed.). Mayfield.
Donor Alliance. (2025). The organ and tissue donation process. https://www.donoralliance.org/professional-partners/
Dutta PA, Flynn SJ, Oreper S, Kantor MA, & Mourad M. (2023). Across race, ethnicity, and language: An intervention to improve advance care planning documentation unmasks health disparities. Journal of Hospital Medicine, 19(1), 5–12. https://doi.org/10.1002/jhm.13248
Estrada LV, Malani PN, & Vitale CA. (2025). Eating and swallowing problems in people with advanced dementia. Journal of the American Medical Association, 334(6), 550. https://doi.org/10.1001/jama.2025.7857
Fadiman A. (1997). The spirit catches you and you fall down. Farrar, Straus, and Giroux.
Fisher J. (2023). 5 stages of grief: Coping with the loss of a loved one. Harvard Health. https://www.health.harvard.edu/mind-and-mood/5-stages-of-grief-coping-with-the-loss-of-a-loved-one
Friedman J. (2025). “Wake-up call”: Aggressive cancer care common at end of life, supportive care lacking. HemOnc Today. https://www.healio.com/news/hematology-oncology/20250521/wakeup-call-aggressive-cancer-care-common-at-end-of-life-supportive-care-lacking
Golhar A. (2024). Types of organ and tissue transplants: What are the most common procedures? https://health.medicaldialogues.in/health-topics/types-of-organ-and-tissue-transplants-what-are-the-most-common-procedures-dr-ankush-golhar-138874
Goodley A. (2024). 7 most expensive human organ transplants in the U.S. https://rarest.org/general/expensive-human-organ-transplants-in-the-us
Harding MM, Kwong J, Roberts D, Hagler D, & Reinisch C. (2023). Lewis’s medical–surgical nursing: Assessment and management of clinal problems (11th ed.). Elsevier.
Health Resources & Services Administration (HRSA). (2024). What can be donated. https://www.organdonor.gov/learn/what-can-be-donated
Heart Rhythm Society (HRS). (2023). HRS expert consensus statement on the management of cardiovascular implantable electronic devices (CIEDS) in patients nearing end of life or requesting withdrawal of therapy. https://www.hrsonline.org/guidance/clinical-resources/2010-hrs-expert-consensus-statement-management-cardiovascular-implantable-electronic-devices-cieds
Hwang DY, Oczkowski SJ, Lewis K, Birriel B, Downar J, et al. (2025). Society of Critical Care Medicine guidelines on family-centered care for adult ICUs: 2024. Critical Care Medicine, 53(2), e465–82. https://doi.org/10.1097/CCM.0000000000006549
Jain S. (2025). What is a durable power of attorney, and how does it work? https://www.legalzoom.com/articles/what-is-a-durable-power-of-attorney
Jose CG, Lucy R, Parker AM, Clere J, Montecillo L, & Cole AM. (2024). Pakikisama: Filipino patient perspectives on health care access and utilization. The Journal of the American Board of Family Medicine, 37(2), 242–50. https://doi.org/10.3122/jabfm.2023.230165R2
Kang KA, Kim DB, Koh SJ, Park MH, Park HY, et al. (2023). Spiritual care guide in hospice∙palliative care. Journal of Hospice and Palliative Care, 26(4), 149–59. https://doi.org/10.14475/jhpc.2023.26.4.149
Kingsly Clinic. (2025). Erythropoiesis-stimulating agents: Effective anemia treatment options. https://thekingsleyclinic.com/resources/erythropoiesis-stimulating-agents-effective-anemia-treatment-options/
Kübler-Ross E. (1969). On death and dying. Macmillan.
Lerner M. (1996). Choices in healing: Integrating the best of conventional and complementary approaches to cancer. MIT Press.
Leukemia and Lymphoma Society (LLS). (2025). Children and end of life. https://www.lls.org/managing-your-cancer/end-life-care/children-and-end-life
Lightner B. (2022). Palliative sedation. https://www.ebsco.com/research-starters/health-and-medicine/palliative-sedation
Lindemann E. (1994). Symptomatology and management of acute grief. American Journal of Psychiatry, 151(Suppl 6), 155–60.
Linebarger JS, Johnson V, & Boss RD. (2022). Guidance for pediatric end-of-life care. Pediatrics, 149(5). https://publications.aap.org/pediatrics/article/149/5/e2022057011/186860/Guidance-for-Pediatric-End-of-Life-Care
Liu JC, Lo JC, & Gordon NP. (2023). Racial ethnic differences in advance directive completion among middle-aged and older U.S. adults (Sch455). Journal of Pain and Symptom Management, 65(5), e608–9. https://www.sciencedirect.com/science/article/abs/pii/S0885392423002713
Makic MBF & Morata LT. (2024). Sole’s introduction to critical care nursing. Elsevier.
Marie Curie. (2022). Communication needs in palliative care. https://www.mariecurie.org.uk/professionals/palliative-care-knowledge-zone/individual-needs/communication-needs
McCall M. (2023). What is the Uniform Determination of Death Act (UDDA)? FindLaw. https://www.findlaw.com/healthcare/patient-rights/what-is-the-uniform-declaration-of-death-act-or-udda.html
McCuistion LE, Vuljoin-DiMaggio K, Winton MB, & Yeager JJ. (2023). Pharmacology: A patient-centered process approach (11th ed.). Elsevier.
Medicare. (2025). Hospice care. https://www.medicare.gov/coverage/hospice-care
Memory Tree. (2022). Customs and religious protocols: Different cultural beliefs at the time of death. http://www.amemorytree.co.nz/customs.php
Merriam-Webster Dictionary. (2025). Palliative. http://www.merriam-webster.com/dictionary/palliative
MHP Salud. (2022). Promotores and promotoras de salud. https://mhpsalud.org/our-chw-initiatives/promotoras-de-salud/#readmore
Mirasol Health. (2024). Providing hospice and end-of-life care to the homeless. https://mirasolhealth.org/providing-hospice-and-end-of-life-care-to-the-homeless/
Morrow A. (2022). 5 stages of grief when facing a terminal diagnosis. Very Well Health. https://www.verywellhealth.com/dabda-the-five-stages-of-coping-with-death-1132148
National Cancer Institute (NCI). (n.d.). Supportive care. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/supportive-care
National Cancer Institute (NCI). (2025). Cancer stat facts: Common cancer sites. https://seer.cancer.gov/statfacts/html/common.html
National Cancer Institute (NCI). (2024). Depression (PDQ®)—Patient version. https://www.cancer.gov/about-cancer/coping/feelings/depression-pdq#_8
National Health Care for the Homeless Council (NHCHC). (2025). Adapting your practice: Recommendations for end-of-life care for people experiencing homelessness. https://nhchc.org/wp-content/uploads/2019/08/2018-end-of-life-care-guidelines.pdf
National Institute on Aging (NIA). (2023). Advance care planning worksheets. https://www.nia.nih.gov/health/advance-care-planning/advance-care-planning-worksheets
National Institute on Aging (NIA). (2022). Advance care planning: Advance directives for health care. https://www.nia.nih.gov/health/advance-care-planning/advance-care-planning-advance-directives-health-care
Nationwide Children’s. (2025). Discussing death with children. https://www.nationwidechildrens.org/conditions/health-library/discussing-death-with-children
Oliveira T, Monteiro NF, & Cipriano P. (2024). Deactivation of cardiac implantable electronic devices in palliative patients: When and how. Medicina Clínica (English Edition), 163(10), 512–6. https://www.sciencedirect.com/science/article/abs/pii/S2387020624004947
Pan H, Shi W, Zhou O, et al. (2022). Palliative care in the intensive care unit: Not just end-of-life care. Intensive Care Research, 3(102), 77–82. https://doi.org/10.1007/s44231-022-00009-0
Pew Research Center. (2025). Facts about Asians in the U.S. https://www.pewresearch.org/race-and-ethnicity/fact-sheet/asian-americans-in-the-u-s/
Reverso Dictionary. (2025). Hospice. http://dictionary.reverso.net/spanish-english/hospicio
Rhodes RL, Barrett NJ, Ejem DB, Sloan DH, Bullock K, et al. (2022). A review of race and ethnicity in hospice and palliative medicine research: Representation matters. Journal of Pain and Symptom Management, 64(5), e289–99. https://doi.org/10.1016/j.jpainsymman.2022.07.009
Robison J, Shugrue N, Dillon E, Migneault D, Charles D, et al. (2023). Racial and ethnic differences in hospice use among Medicaid-only and dual-eligible decedents. JAMA Health Forum, 4(12), Article e234240. https://doi.org/10.1001/jamahealthforum.2023.4240
San Francisco Board of Supervisors (SFBoS). (n.d.). Section V. Medical examiner’s inquests. https://sfbos.org/section-v-medical-examiners-inquests
Santo L, Peters ZJ, Guluma L, & Ashman JJ. (2025). Visits to health centers, by selected characteristics: United States, 2023. National Center for Health Statistics (U.S.), 216, 1–19. https://dx.doi.org/10.15620/cdc/174585
Schoener B & Borger J. (2024). Erythropoietin stimulating agents. StatPearls. https://pubmed.ncbi.nlm.nih.gov/30725682/
Scripps. (2025). What are the top 10 health concerns for baby boomers? https://www.scripps.org/news_items/5475-top-health-concerns-of-baby-boomers
Sengupta M, Lendon JP, Caffrey C, Melekin A, & Singh P. (2022). Post-acute and long-term care providers and services users in the United States, 2017–2018. National Center for Health Statistics. Vital Health Stat, 3(47). https://dx.doi.org/10.15620/cdc:115346
Shryer D. (2024). Study finds racial disparities in end-of-life hospital care. https://www.mcknights.com/news/study-reveals-racial-disparities-in-end-of-life-care-during-hospital-stays/
SOHO in China. (2024). Chinese cultural considerations in healthcare explained. https://www.sohoinchina.com/cultural-considerations-in-healthcare/
Stanford School of Medicine. (2025). A child’s concept of death. https://www.stanfordchildrens.org/en/topic/default?id=a-childs-concept-of-death-90-P03044
Stanford University. (2023). Doctrine of double effect. Stanford Encyclopedia of Philosophy Archive. https://plato.stanford.edu/archives/fall2025/entries/double-effect/
Statista. (2025). Hospice and end-of-life care in the U.S.—Statistics and facts. https://www.statista.com/topics/13209/hospice-care-in-the-us/#topicOverview
UNAIDS. (2024). The urgency of now: AIDS at a crossroads, 2024 global AIDS update. https://www.unaids.org/sites/default/files/media_asset/2024-unaids-global-aids-update_en.pdf
United Network for Organ Sharing (UNOS). (2025). Data and trends. https://unos.org/data/
U.S. Department of Health & Human Services (U.S. DHHS), Administration for Children & Families. (2024). About TANF. http://www.acf.hhs.gov/ofa/programs/tanf/about
U.S. Department of Veterans Affairs (U.S. DVA). (2025). Hospice care. https://www.va.gov/geriatrics/pages/Hospice_Care.asp
U.S. Department of Veterans Affairs (U.S. DVA). (2024). VA caregiver support program. https://www.caregiver.va.gov/REACH_VA_Program.asp
U.S. Food & Drug Administration (U.S. FDA). (2024). Safe opioid disposal: Remove the risk outreach toolkit. https://www.fda.gov/drugs/ensuring-safe-use-medicine/safe-opioid-disposal-remove-risk-outreach-toolkit
USA Facts. (2023). What is the U.S. infant mortality rate? https://usafacts.org/articles/what-is-the-us-infant-mortality-rate/
USLegal. (2025). Understanding the Uniform Anatomical Gift Act-UAGA: Legal insights and implications. https://legal-resources.uslegalforms.com/u/uniform-anatomical-gift-act-uaga
Vitas Healthcare. (n.d.). Challenges in pediatric end-of-life care. http://www.vitas.com/resources/end-of-life-care/challenges-in-pediatric-end-of-life-care
Vossel H. (2025). Keys to improving palliative care community outreach. Hospice News. https://hospicenews.com/2024/09/05/combined-nahc-nhpco-unveils-new-name-brand-identity/
Washington State Department of Health (WSDOH). (2025). Portable orders for life sustaining treatment (POLST). https://doh.wa.gov/you-and-your-family/illness-and-disease-z/portable-orders-life-sustaining-treatment-polst
We Honor Veterans. (2025). We Honor Veterans recognizes the unique needs of America’s veterans and their families. https://www.wehonorveterans.org/
Well-Wisp. (2025). Understanding Hispanic American health beliefs. https://wellwisp.com/hispanic-american-health-beliefs/
Wolters C. (2024). How to choose a hospice provider and questions to ask. US News & World Report. https://health.usnews.com/senior-care/articles/how-to-choose-and-questions-to-ask-a-hospice-provider-near-you



Customer Rating
5.0 / 145 ratings