Fall Prevention
Interventions for Balance Problems and Risks
Online Continuing Education Course

Course Description
Accidental falls are the second most common cause of unintentional death worldwide. Learn about risk factors for falls and their impacts on the patient and medical team. This course covers prevention and interventions for falls in clinical and home settings and is offered for nursing, OT, and PT CEU.
"Increased my knowledge of falls and prevention." - Michelle, RN in Ohio
"Very comprehensive & educational." - Susanne, RN in California
"Very well presented and very well organized. All areas of the subject were covered." - Clara, RN in New Jersey
"Thank you for this course. I will promote it to others!" - Carol, PT in California
Fall Prevention
Interventions for Balance Problems and Risks
Copyright © 2023 Wild Iris Medical Education, Inc. All Rights Reserved.
LEARNING OUTCOME AND OBJECTIVES: Upon completion of this course, you will have gained increased knowledge related to preventing falls in clinical and community-based settings. Specific learning objectives to address potential knowledge gaps include:
- Discuss the impact of falls on patients, clinicians, caregivers, and facilities.
- Summarize the components involved in maintaining balance.
- Understand the primary roles of the interdisciplinary team members in managing patients at risk of impaired balance and falls.
- Identify common risk factors for balance impairments and increased falls.
- Describe how to assess a patient for increased risk of falls.
- Discuss appropriate fall prevention and risk mitigation strategies for individuals at increased risk of falling in both clinical and community settings.
TABLE OF CONTENTS
FALLS AND THEIR IMPACTS
Falls present a serious and growing public health problem. The World Health Organization defines a fall as “an event which results in a person coming to rest inadvertently on the ground or floor or other lower level” (WHO, 2021a). Falls may be fatal or nonfatal, though most are nonfatal.
Falls have been identified worldwide as the second most common cause of unintentional death. It is estimated that approximately 684,000 people die from fall-related injuries each year, with over 80% of fatal falls occurring in low- or middle-income nations (WHO, 2021a). In the United States, over 36 million falls in older adults (ages 65+) are reported each year, resulting in nearly 3 million people being treated in emergency departments, with over 800,000 older adults subsequently hospitalized and over 32,000 deaths (CDC, 2020a).
Fall risk continues to rise with increased age. Globally, people over age 65 are estimated to have a 1-in-3 risk of a fall during a given year. For older adults, a fall can be a serious threat to health, mobility, and long-term independence, which can also impact caregivers and other family members. Even when falls are not fatal, they can have serious and far-reaching consequences. For example, at least 20% of older people who fall in the United States suffer moderate to severe injuries such as bruises, hip fractures, or head trauma. Over 95% of hip fractures, which can have serious long-term negative effects, are caused by falls. Those who experience a fall are 2–3 times more likely to have another fall (CDC, 2021, 2023a; WHO, 2021b).
For older adults living in facilities, the risks are still higher. Worldwide, it is estimated that nursing home residents experience 1.6 falls per bed per year on average, with almost half of residents experiencing multiple falls per year. Those who require low-to-middle levels of care experience more falls than those requiring either a high level of care or no care (WHO, 2021b).
The financial burden of treating falls is profound. Annual direct medical costs of treating nonfatal fall-related injuries in the United States exceed $50 billion, with $754 million spent on costs related to fatal falls, which places a significant burden on both Medicare and Medicaid, as well as on private insurers and individuals. These medical costs include hospital and nursing home care, healthcare provider and other professional services, rehabilitation, community-based services, rental or purchase of durable medical equipment, prescription drugs, and insurance claims processing (CDC, 2020b). As reported by the National Council on Aging in 2021, the average hospital cost of a fall-related injury exceeds $30,000 (NCOA, 2021).
As a person’s age increases, so too does the average cost of treating a fall-related injury. Indirect costs resulting from falls may include long-term effects such as disability, loss of personal independence, time lost from work and household duties, diminished social and/or community engagement, and overall reduction in quality of life (CDC, 2020b). When falls occurs, fear of falling again may cause older people to limit their household or social activities. Both fear of falling (with or without an accompanying fall event) and actual falls have been independently associated with decreased perceived quality of life (NCOA, 2021; Schoene et al., 2019).
The consequences of falls are not limited solely to the individual who experiences the fall. Loss of independence following a fall event may lead an individual to depend more on caregivers. Research indicates that caregivers may feel increased burden of care, fear of recurrent falls, and potentially increased risk of caregiver depression following the care recipient’s first fall. When surveyed, 1 in 5 caregivers reported increased physical strain as a result of caregiving, while over 40% of caregivers reported a need for more information on how to keep care recipients safe in the home setting (NCOA, 2021).
When preventable falls occur in a facility setting as a result of errors or oversights, both patient welfare and a facility’s finances and reputation may be adversely affected. In 2008, the Centers for Medicare and Medicaid Services stopped reimbursing hospitals for costs related to patient falls, leaving facilities and staff with increased responsibility for making fall prevention a high priority and crucial component of patient care (Fehlberg et al., 2017).
However, for such a serious public health problem, falls are also among the most preventable. Research has shown that injury prevention programs related to falls can significantly decrease the incidence and reoccurrence of balance-related falls for those at risk. Adopting clear and consistent safety guidelines and providing comprehensive education for patients, caregivers, and clinicians may help facilities reduce their risk of patient falls and related injuries, allowing them to provide better care for at-risk patients.
FALLS AND HEALTHCARE-ACQUIRED CONDITIONS
Falls were deemed a healthcare-acquired condition (HAC) by the 2005 Deficit Reduction Act, and hospitals no longer receive reimbursement for treating injuries resulting from falls occurring during hospitalization. Under the 2015 Hospital-Acquired Condition Reduction Program (HACRP), Medicare decreased payments by 1% to hospitals who score in the bottom quartile of performance based on risk-adjusted measures of certain hospital-acquired conditions, including surgical site infections, pressure injuries, or hip fractures resulting from falls (CMS, 2022a, 2022b).
COMPONENTS OF BALANCE
It is commonly accepted that falling is often, if not nearly always, the result of “losing one’s balance.” But what exactly does balance mean and how does its presence or absence contribute to falls?
Defining “Balance”
Balance refers to the ability of an individual to maintain their line of gravity within an established base of support. Alternatively, balance may be described as being able to maintain one’s equilibrium, or a state in which all acting forces cancel one another and create a stably balanced system. Postural control, postural stability, and equilibrium are alternative terms for balance (Physiopedia, 2023a).
Static balance is the ability of the body to be held in a fixed (unmoving) position, maintaining postural orientation and stability with the body at rest and the center of mass held over the base of support. Dynamic balance, in contrast, is the ability to maintain stability and orientation of one’s posture while the body is in motion (Bannister, 1969, quoted in Physiopedia, 2023a).
Systems of Balance
When properly functioning, the human balance systems allow individuals to:
- Clearly see surroundings while in motion
- Determine orientation with respect to gravity
- Interpret the speed and direction of movement
- Make continuous and automatic adjustments to posture
These abilities contribute to maintaining stability while engaging in various activities under varying environmental conditions (VeDA, 2023a).
Balance, or the lack thereof, is thus not a function of merely one discrete component but is the result of input from several distinct sensorimotor control systems within the human body that work synergistically. The ability of an individual to maintain balance is controlled by integrated sensory input from vision, proprioception, and the vestibular system, with subsequent motor output to the muscles of the eyes and body. If one or all of these components is adversely affected (which may be caused by factors such as disease, injury, aging, or drugs), an individual’s overall balance may become compromised (VeDA, 2023a; Physiopedia, 2023a).
VISUAL SYSTEM
The retinae of the eyes contain rods (for vision in low-light situations) and cones (for color and fined-tuned vision). When struck with light, these structures convey impulses to the brain with visual cues regarding how the body is orientated relative to surrounding objects. The visual system provides approximately 10% of total balance input on stable surfaces and 30% on unstable surfaces.
Many different visual dysfunctions contribute to problems with balance. A few examples include:
- Aniseikonia: A condition in which there is a significant difference in how an individual’s right versus left eye perceives an image’s size, which may cause disorientation, eyestrain, headache, and/or issues with dizziness and balance.
- Vertical imbalance: A condition in which one eye aims higher than the other instead of both eyes working in synchrony. An affected person will frequently tilt their head to help align the eyes in order to try to compensate for this vertical maladjustment, which may then adversely affect the vestibular fluid of the inner ear.
- Binocular vision dysfunction: A condition in which the eyes struggle to work together when aiming or focusing at a point in space or when quickly changing gaze between closer and farther objects. It may be caused by brain injury to specific neural centers and can lead to eye teaming/focusing issues, resulting in double or blurry vision.
(NORA, 2023)
SOMATOSENSORY/PROPRIOCEPTIVE SYSTEM
Proprioceptive information from the skin, muscles, and joints involves sensory receptors that are sensitive to stretch or pressure in the surrounding tissues. Proprioceptive cues help a person’s body determine its position in space. Of particular importance to balance, cues from the neck indicate the direction the head is turned, and cues from the ankles indicate body movement and/or sway relative to the standing surface and its quality (soft, uneven, solid, etc.). The somatosensory/proprioceptive systems provide approximately 70% of total balance input on stable surfaces and 10% on unstable surfaces (VeDA, 2023a; Physiopedia, 2023a).
Problems related to the somatosensory/proprioceptive systems may adversely affect balance. For example:
- Impaired cervical range of motion is associated with diminished protective responses and/or balance. Patients with cervical pain/dysfunction often experience symptoms of dizziness/light-headedness and/or unsteadiness, which lead to increased fall risk (Sung, 2020).
- Loss of ankle range of motion and proprioception after ankle injury has been shown to adversely impact postural and balance control, and athletes with impaired ankle proprioception post injury tend to perform more poorly in both static and dynamic postural and balance control tasks (Alghadir et al., 2020).
- Sensory impairments such as diabetic peripheral neuropathy have been shown both to significantly diminish an individual’s functional balance and to increase their risk of falls (Reeves et al., 2021).
VESTIBULAR SYSTEM
The vestibular apparatus is located within each inner ear. It includes the utricle, saccule, and three semicircular canals and provides sensory information regarding equilibrium, motion, and spatial orientation. The utricle and saccule detect linear movement and vertically oriented input (i.e., gravity), while the semicircular canals detect rotational movement.
The semicircular canals are located at right angles to one another and are filled with endolymphatic fluid. When the head is turned in certain directions, the endolymphatic fluid in the corresponding semicircular canal moves more slowly due to inertia, placing pressure against the canal’s sensory receptor, which subsequently sends impulses to the brain specifically about the movement occurring in that particular canal.
When the vestibular system is functioning correctly, these impulses are symmetrical to both sides of the head. The vestibular system provides approximately 20% of total balance input on stable surfaces and 60% on unstable surfaces (VEDA, 2023b).
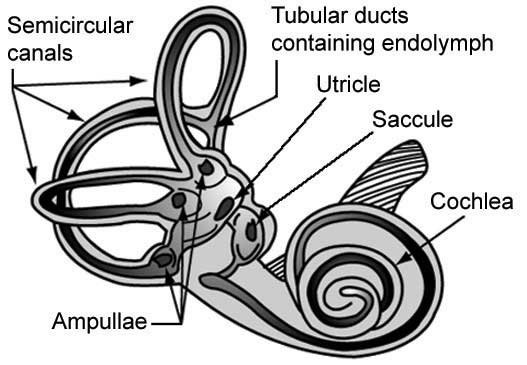
Vestibular system. (Source: NASA.)
There are a number of conditions that can cause vestibular system dysfunction, which may in turn lead to dizziness or affect balance. Some examples include:
- Benign paroxysmal positional vertigo (BPPV): The most common cause of vertigo, BPPV is a mechanical problem that occurs when calcium carbonate crystals (called canaliths or otoliths) become displaced in the inner ear, stimulate nerve hairs, and send false movement signals to the brain, which can cause dizziness and visual disturbance. This may occur as a result of infection, trauma, or normal aging.
- Acoustic neuroma: Nonmalignant tumor that develops on the sheath of the inner ear’s vestibulocochlear nerve. Also known as vestibular schwannoma.
- Autoimmune inner ear diseases: Includes Cogan’s syndrome, relapsing polychondritis, polyarteritis nodosa, Wegener’s granulomatosis, systemic lupus erythematosus, ulcerative colitis, Sjogren’s syndrome, and rheumatoid arthritis.
- Cholesteatoma: A skin growth that occurs in the middle ear behind the eardrum; can increase in size and destroy middle ear structures over time.
- Labyrinthitis and vestibular neuritis: Disorders resulting from an infection of the inner ear or the nerves connecting the inner ear and brain, disrupting transmission of sensory information.
- Mal de débarquement syndrome (MDDS): Most commonly occurs after sea or other forms of travel; the sensation of movement continues after movement has stopped. Cause not definitely known, may last for weeks, months, or even years.
- Migraine associated vertigo (MAV): Approximately 40% of migraine patients have some accompanying vestibular syndrome involving disruption in their balance and/or dizziness; thought to be a combination of altered vascular and neural processes.
- Otosclerosis: Abnormal bone growth in the middle ear, which can cause hearing loss, dizziness, balance problems, or tinnitus.
- Ototoxicity: Poisoning that results from exposure to drugs or chemicals that damage the inner ear or the vestibulocochlear nerve; may be temporary or permanent.
- Perilymph fistula: A tear or defect in either or both the oval window and the round window that separate the middle and inner ear, allowing perilymph to leak into the middle ear. Most frequently caused by head trauma (such as a direct blow or a whiplash injury). Other causes include ear trauma, perforated eardrum, “ear block” during airplane descent, or scuba diving.
- Persistent postural perceptual dizziness (PPPD): Postural dizziness without vertigo and fluctuating unsteadiness provoked by environmental or social stimuli (e.g. crowds), not attributable to another neuro-otologic disorder.
(VEDA, 2023c)
VERTIGO VS. DIZZINESS
While the terms are often used interchangeably, these are two distinct symptoms. Dizziness can refer to a general feeling of feeling off-balance, or like you are about to fall. Vertigo, in contrast, is a sense of feeling as though you or your surroundings are actually moving (Healthline, 2023).
INTERDISCIPLINARY TEAM IN FALL MANAGEMENT AND PREVENTION
Since falls are often a combination of multiple causative factors, the skills of multidisciplinary teams are frequently required to determine and implement the best possible management and prevention plan and quality assurance processes, with appropriate referrals made between various members within the team according to a patient’s demonstrated areas of need. There may be significant overlap in care, with clinicians from more than one discipline addressing the same issues (e.g., patient safety education, vestibular rehabilitation).
A comprehensive management team may include (but is not limited to) the following disciplines and tasks:
Physicians/Primary Care Providers
- Examine for, diagnose, and manage medical causes of falls
- Make referrals to other disciplines or community-based programs, as appropriate
Nurses
- Coordinate care between multidisciplinary team members
- Supervise and/or educate facility staff on the patient’s fall risk status and current safety measures
- Monitor patient status (vital signs, etc.) for changes
- Document and implement risk-reduction strategies (in facility settings)
- Provide patient education/advocacy
Physical Therapists
- Evaluate and help improve strength, balance, and community-level mobility
- Provide recommendations and training on assistive devices (such as canes, walkers, grab bars, etc.)
- Help identify community-based exercise programs for long-term activity options
- Provide more advanced vestibular evaluation and rehabilitation (when specially trained and/or certified)
Occupational Therapists
- Evaluate safety of activities of daily living (ADLs) and offer adaptive strategies as needed
- Assess and offer strategies for optimizing home- or community-based safety
- Provide more advanced vestibular evaluation and rehabilitation (when specially trained and/or certified)
Other Care Team Members
- Psychologists: Screen for any underlying cognitive impairments or depression; help connect individuals to community-based support
- Pharmacists: Review medications for side effects (dizziness, light-headedness, altered blood pressure, etc.) that may affect balance and work with physicians to minimize side effects of consider alternate medication options
- Optometrists/ophthalmologists: Assess vision and vision-related needs that may affect balance
- Audiologists: Assess hearing and screens for vestibular-related issues that may affect balance
Community-based organizations (such as senior centers, parks/recreation departments, hospitals, churches, etc.) may also provide support resource such as affordable exercise/activity options.
(FPTA, n.d.; VEDA, 2023d; Performance Health, 2023)
ASSESSING A PATIENT’S FALL RISK
Identifying specific fall risks and the most appropriate strategies for intervention can be a complex task and may involve multiple members of a healthcare team. Physicians and other primary care providers, nurses, physical therapists, occupational therapists, social workers, caregivers/family members, and the patient/client all hold key areas of expertise that may help build a complete picture of the multiple factors that may put someone at risk for falling.
Every person’s situation is unique, with a distinct combination of physical/functional status, cognitive ability, living situation, family/caregiver supports, and other resources. Most falls are multifactorial in nature and unique to an individual’s specific situation; therefore, there is no one correct means to accurately predict fall risk. Instead, it is recommended that clinicians rely upon a more holistic assessment. The information gathered from multiple information sources may identify multifactorial issues, which are then addressed by various appropriate interventions (Mishra et al., 2022).
Intrinsic and Extrinsic Fall Risk Factors
Most falls occur as a result of multiple factors, and having a greater number of risk factors makes it increasingly likely that a person will suffer a fall. The risk level may be due in part to physical, sensory, and cognitive changes associated with aging in combination with environments that are not adapted for an aging population (Physiopedia, 2023b).
Some risk factors cannot be altered, while others may be lessened or even eliminated. Fall risk factors are either intrinsic (inherent to an individual) or extrinsic (pertaining to situational and/or environmental factors outside an individual).
INTRINSIC FALL RISK FACTORS
- Advanced age (>60 years)
- Young age (due to childhood developmental stages, innate curiosity, and risk-taking behavior)
- Gender (older females more likely to sustain severe injury from falls, males have higher rates of injury and death across lifespan)
- Previous falls
- Muscle weakness
- Gait disorders
- Balance disorders
- Foot and/or ankle disorders
- Poor or insufficiently corrected vision
- Postural hypotension
- Chronic conditions (arthritis, cerebrovascular accident, incontinence, diabetes, neurologic conditions, etc.)
- Impaired cognition
- Fear of falling
(Physiopedia, 2023b; Lee et al., 2022)
EXTRINSIC RISK FACTORS
- Lack of stair handrails
- Poor stair design
- Lack of bathroom grab bars
- Dim lighting or glare
- Obstacles and tripping hazards
- Slippery or uneven surfaces
- Psychoactive medications
- Taking more than one medication (polypharmacy)
- Improper use of an assistive device
- Occupations at elevated heights or other hazardous working conditions
- Alcohol or substance use
- Socioeconomic factors (poverty, overcrowded housing, sole parenthood, young maternal age)
(Physiopedia, 2023b; Lee et al., 2022)
Multifactorial Risk Assessment and Patient History
Falls-related clinical guidelines include recommendations from the World Falls Task Force (see box below), the American Geriatric Society, the British Geriatric Society, and the American Academy of Orthopedic Surgeons. While there are many areas of overlap between various guidelines, a recent systematic review by the Journal of the American Medical Association found that there are also considerable variations in consistency between recommendations in some areas (Montero-Odasso et al., 2021).
The components of the risk assessment described below have been drawn from numerous existing guidelines. They include a careful and comprehensive patient history in order to gain valuable information regarding an individual’s intrinsic and extrinsic risk factors for falling, which can, in turn, help to appropriately guide any needed interventions and/or preventive strategies (Physiopedia, 2023b).
WORLD GUIDELINES
In 2022, the World Falls Task Force, a global collaboration of 96 multidisciplinary experts from 39 countries and representing 36 scientific/academic societies, developed and released The World Guidelines for Fall Prevention and Management for Older Adults: A Global Initiative. These global guidelines are intended to provide a comprehensive framework and recommendations resource for clinicians and other professionals who work with the older adult population and to provide guidance for fall risk assessment and management.
World Falls Task Force guidelines include the following recommended framework with regard to individual fall risk assessment (with tailoring as needed to adapt to diverse environments and patient populations):
- Risk stratification (categorizing older adults into low, medium, or high risk of falling)
- Risk assessment
- Management/interventions
- Assessment and treatment
(Task Force, 2022)
SCREENING FOR FALL RISK
Numerous guidelines recommend that all older adults receive a basic fall screening on an annual basis. This may help determine specific risk levels and thus guide an individually tailored, multifactorial prevention and/or management strategy. Risk stratification may be completed as part of regular annual clinical exam, during a hospitalization, and/or after any fall-related event. Patients may be asked about:
- Falls within the past 12 months
- Severity of any recent falls
- Dizziness or altered consciousness
- Feeling of unsteadiness or difficulty walking
- Fear of falling (particularly if severe enough to limit activities)
Based upon the information gathered from such screening questions, clinicians may be able to categorize patients according to risk categories and provide associated recommendations (see table below) (Physiopedia, 2023b; Montero-Odasso et al., 202; Task Force, 2022).
| Category | Description | Recommendation |
|---|---|---|
| (Task Force, 2022) | ||
| Low risk | No fall in last 12 months or nonsevere fall without gait or balance impairment | General fall prevention education and exercise/fitness recommendations |
| Intermediate risk | Nonsevere fall with gait or balance impairment | Physical therapy referral and/or specific balance and strengthening exercise recommendations in addition to general fall prevention education |
| High risk | Severe fall with gait and balance impairment | Highly individualized management, including a comprehensive/multifaceted fall risk assessment |
FALL RISK ASSESSMENT
Fall risk assessment should be performed by a healthcare professional with appropriate skills and experience and may include:
- Identification of fall history (particularly within the past year)
- Assessment for impaired mobility (gait, balance, strength, assistive device use, foot conditions/footwear, etc.)
- Assessment of dizziness, hearing, and/or vestibular issues
- Assessment of heart rate, rhythm, and blood pressure
- Assessment of ADLs (activities of daily living)
- Assessment of osteoporosis risk
- Assessment of the person’s perceived functional ability and fear related to falling
- Assessment of visual impairment
- Assessment of cognitive impairment, mental status, and neurological examination
- Assessment of urinary continence
- Assessment of home hazards
- Cardiovascular examination
- Review of overall medication history, polypharmacy, etc.
- Assessment of vitamin D levels (as locally indicated)
- Assessment for history or presence of orthostatic hypotension
- Assessment for current medications specifically associated with falls (e.g., sedative-hypnotics, blood pressure drugs)
(NICE, 2023; Task Force, 2022; Physiopedia, 2023b)
Medical Tests
For individuals with a history of falling, their primary care provider may order certain tests to rule out specific conditions and/or injuries, as well as complete a review of the patient’s most current list of medications. Some common, relevant medical tests may include (but not be limited to):
- Complete blood count (to detect leukocytosis or anemia)
- Blood glucose measurement
- Electrolyte measurement to test for dehydration
- Electrocardiogram (ECG), ambulatory cardiac monitoring, and/or echocardiography if cardiac pathology is suspected
- Carotid massage (with cardiac monitoring and IV access) to help determine whether a pacemaker may be indicated
- Magnetic resonance imaging (MRI), computerized tomography (CT), and/or spinal x-rays (if new neurological abnormalities are present)
(Merck & Co., 2022a)
MEDICATIONS REVIEW
According to the CDC, it is important for a patient’s medical provider and/or pharmacist to conduct a comprehensive medication review to look for the presence of central nervous system active or psychoactive medication; presence of any medication that can cause dizziness, sedation, orthostatic hypotension, blurred vision, or confusion; or use of four or more medications (polypharmacy), as any of these factors can increase fall risk. The STEADI-Rx Older Adult Fall Prevention Guide for Community Pharmacists is a newer tool to assist with identifying medication-based fall risks and promoting interdisciplinary coordination in fall risk reduction (CDC, 2020c).
The American Geriatrics Society (AGS, 2019) released the Beers Criteria, with the collaboration of a 13-member interdisciplinary panel of experts in geriatric care and pharmacotherapy, in order to provide clinicians with recommendations on drugs that may be inappropriate and/or unsafe for older adults, including those that may increase risk of falls. The list is periodically updated based on careful review of the most up-to-date evidence and is available in pocket-sized clinician guides.
Functional Assessment
There are a wide variety of functional assessment tools available for helping to determine an individual’s risk of falling. Some tools are self-assessments that may be used by individuals and/or their caregivers; others require specialized training to administer and should only be carried out by clinicians with appropriate levels of training. It is important to consider an individual’s physical capabilities, previously known risk factors, home and living environment, and level of family/caregiver support when selecting an appropriate assessment tool.
FALL RISK FUNCTIONAL ASSESSMENT TOOLS
Some commonly used tools in clinical and community settings are:
- 2-Minute Walk Test (2MWT): Assesses walking distance over a timed period of two minutes to determine walking endurance.
- Activities-Specific Balance Confidence Scale (ABC): Self-administered or conducted in person or via telephone; participants indicate level of self-confidence that they will not lose balance or become unsteady during 11 various activities.
- Ankle range of motion: Measured using goniometer, inclinometer, or knee-to-wall ratio (using tape measure), ideally by a rehabilitation professional skilled in joint measurement with kinesiology background; lower-than-average ankle dorsiflexion linked to increased risk of balance-related falls in some populations as one factor contributing to variance in gait and balance performance.
- Berg Balance Scale (with adaptations for special patient populations): 14-item scale measuring balance of an adult in a clinical setting (does not assess gait); requires 15 to 20 minutes to administer; training required to administer.
- Dizziness Handicap Inventory (DHI) for Benign Paroxysmal Positional Vertigo (BPPV): Subjective 25-item patient self-assessment that measures functional limitation due to vestibular-related vertigo.
- Dynamic Gait Index: Assesses eight facets of gait in order to predict fall risk in community-dwelling older adults.
- Elderly Mobility Scale (EMS): 20-point validated scale that assesses functional mobility of frail older adult subjects in hospital settings.
- Falls Efficacy Scale-International (FES-I): 16-item self-assessment that assesses fear of falling in community-dwelling older adult populations.
- Falls Risk Assessment Tool (FRAT): Assesses fall risk via brief, clinician-administered questions; offers general guidance on any identified areas of fall risk.
- Four Step Square Test: Assesses an individual’s dynamic balance when stepping over objects forward, backward, and sideways.
- Functional Independence Measure (FIM): 18-item assessment of physical, psychological, and social function for individuals with any motor impairment that addresses feeding, grooming, bathing, upper-body dressing, lower-body dressing, and toileting.
- Functional Reach: Assesses a patient’s/client’s ability to reach outside a fixed based of support while maintaining balance; may be modified to perform in sitting posture if needed.
- Head-Shaking Nystagmus Test (pHSN): Tests for peripheral vestibular disorders by observing for presence of nystagmus during specific abrupt head movements; training and specialized equipment highly recommended for administration.
- STEADI Falls Screening Tool: Used for screening and fall risk assessment; includes patient questionnaire, fall history, and balance performance tests (Timed-Up-and-Go [TUG], static balance testing, and 30-second sit-to-stand).
- Timed-Up-and-Go (TUG), with optional cognitive (TUG-COG) and/or manual (TUGman) variations: Assesses dynamic mobility for determining fall risk by observing the patient/client rising from a chair, walking a predetermined distance, and returning to sitting; may be modified by adding cognitive and/or manual task components.
- Tinetti Performance-Oriented Mobility Assessment (POMA): Assesses gait and balance; rates ability to maintain balance while performing ADL-related tasks; training recommended to administer.
(Prost, 2021; CDC, 2023b; Physiopedia, 2023c, 2023d; Shirley Ryan Abilitylab, 2020a–i; Smiling Senior, 2023; University of Scranton, 2020; Healthy Aging Resource Group, 2023).
Comprehensive Balance Evaluation
While not all falls are the result of specific balance impairments, problems with balance do comprise a significant subset of risk factors for falling. If an initial patient screening shows any potential red flags for specific balance impairments, a referral to a physical therapist may be indicated. A physical therapist may perform a comprehensive balance evaluation to determine specific causes of impairment and to design an appropriate intervention strategy.
When conducting a balance assessment, the following questions may be helpful in obtaining detailed and relevant patient information:
- How often do you experience problems with your balance?
- What are you doing when you experience balance problems?
- Is your balance worse at nighttime or in dark rooms?
- Does the room spin, or do you feel off balance?
- How many times have you fallen in the past year?
- Have you suffered injuries from falling?
- Have you changed or limited your daily activities because of your balance problems?
- What medications do you take?
- Have you had a vision or ear checkup recently?
- Do you have difficulty with any daily activities?
- How much and what kind of daily exercise do you get?
- Do you have any other medical conditions or problems?
- Are you under the care of a physician?
- What are your goals?
(APTA, 2021)
Home Safety Assessment
A home safety assessment by a healthcare professional is particularly valuable when there are questions or concerns regarding a patient’s/client’s ability to safely navigate their home environment physically and/or cognitively, with sufficient safety awareness to minimize risk of injury. Observing an individual operating within their home environment provides a more holistic picture of their functional abilities than can be gleaned solely from a more controlled clinical setting.
A comprehensive home safety assessment provides an in-depth evaluation of potential structural and/or environmental hazards or concerns that may put an individual at greater risk for a fall. Home safety assessments may be performed by occupational therapists, physical therapists, medical social workers, specially trained nurses, or other appropriately trained professionals. A referral from a primary care provider or home health services may be needed for a patient to receive a professional home safety assessment.
(Recommendations for addressing specific safety deficits or potential hazards are discussed later in this course.)
CLINICIAN HOME SAFETY ASSESSMENT TOOLS
- Safe at Home Checklist: Created in partnership by the Administration on Aging and the American Occupational Therapy Association (AOTA), this checklist is used by clinicians to identify home safety, fall hazards, and accessibility issues for homeowners, patients/clients, and/or family members. It includes modifiable checklists of suggestions for addressing specific identified safety concerns.
- I-HOPE: This tool identifies performance struggles faced by individuals in their homes, with the clinician observing for barriers during problematic activities. Each barrier carries a score to determine severity level. Designed for individuals with higher functional levels, it is not appropriate for pediatric clients or for those with dementia.
- SAFER-HOME: A task performance observation and an interview are combined to assess safety concerns and functional performance. This tool addresses mobility, household, and bathroom safety. It does not fully address issues such as food preparation and personal care.
(AOTA, 2019)
When conducting a home safety assessment, it is important for clinicians to remember that what may seem like clutter or a hazard to them may mean something entirely different to the individual and/or their family. Mementos, keepsakes, old furniture, and other seemingly replaceable items may hold great sentimental value for their owners. Clinicians should be mindful of potential emotional attachments and be respectful of an individual’s available resources and values when identifying potential environmental modifications.
PATIENT HOME SAFETY SELF-ASSESSMENT
There are a number of home safety checklists available for use by a patient and their family to examine their own living environment for potential hazards that may increase risk of a fall at home. Two examples include:
- Check for Safety: A Home Fall Prevention Checklist for Older Adults: Created by the CDC, this brief checklist helps assess a home for common environmental fall risks (such as clutter, loose rugs, improper lighting) and provides suggestions for addressing these risks.
- Home Safety Self-Assessment Tool (HSSAT): Created by the University of Buffalo’s Occupational Therapy Geriatric Group, this extensive tool includes a screening checklist for identifying environmental hazards in the home as well as written and video resources with suggestions and instructions for specific home safety improvements.
(See also “Resources” at the end of this course.)
FALL PREVENTION STRATEGIES
The best strategy to avoid the negative impacts of falls is to prevent them from happening in the first place. It is in the best interests of everyone involved in patient/client care—clinicians, caregivers, facilities, and most importantly, at-risk patients/clients themselves—to consider and adopt comprehensive and individualized strategies and planning to minimize the risk of falls.
Whether in clinical, community, or home-based settings, there are a number of strategies to mitigate risk of patient falls. There is no one-size-fits-all strategy; effective fall prevention planning is highly specific to an individual’s unique situation, environment, and needs.
Interventions Based on Type of Fall Risk in Clinical Settings
In order to design the most effective prevention strategies in the clinical environment, it is helpful to determine which specific type(s) of fall an individual may be most at risk for. The primary types of fall risk include anticipated physiologic falls, unanticipated physiologic falls, and accidental falls.
ANTICIPATED PHYSIOLOGIC FALLS
Anticipated physiologic falls may be predicted when patients have certain known risk factors. Examples of risk factors for anticipated physiologic falls may include:
- Muscle weakness or balance difficulties
- History of falling
- Frequent toileting needs and/or urinary urgency
- Altered mental status, such as dementia, which can lead to disorientation
- Vision or hearing problems
- Certain medications (especially those that have side effects such as dizziness or lightheadedness) or polypharmacy
Intervention strategies for anticipated physiologic falls require careful consideration of a patient’s specific risk factors, both intrinsic (visual impairment, balance, gait, sensory neuropathy, orthostatic hypotension, confusion, etc.) and extrinsic (medications, mobility aids, etc.). To minimize risk of anticipated physiologic falls, the following strategies may be useful:
- Employ interventions tailored to the patient’s identified risk factors.
- Implement consistent toileting schedules and encourage consistent drinking schedules for patients with elimination needs.
- Ensure that patients have access to visual and auditory aids (glasses, hearing aids, etc.) if indicated.
- Consult with medical provider about alternative medication options, if indicated.
- Ensure a safe, consistent environment (e.g., no clutter, mobility aids within reach).
- Referrals to rehabilitation specialists (such as physical, occupational, or speech therapy) may be beneficial for further evaluation of specific concerns related to mobility, assistive equipment, ADL function, cognition, etc.
(Progress Lifeline, 2021)
UNANTICIPATED PHYSIOLOGIC FALLS
These falls may occur with a temporary change in physical or cognitive function and unfamiliar surroundings. Such falls are considered unanticipated because the patient may be otherwise classified as lower risk for falls. This type of fall may potentially occur with conditions such as seizures, syncopal episodes, delirium, stroke, or heart attack. Due to the unexpected and often sudden nature of these falls, preventative strategies may be difficult to implement, and it is important to consult closely with the patient’s medical provider to address potential underlying medical causes. Following an unanticipated physiologic fall, it may be useful to consider assistive technology options, which may alert caregivers to subsequent falls (Yang, 2023; Progress Lifeline, 2021).
ACCIDENTAL FALLS
This type of fall can stem from slipping, tripping, or other accidents and is frequently linked to extrinsic (and often modifiable) factors such as obstacles, poor lighting, or poorly designed ergonomic features in the immediate environment.
Risk reduction strategies for accidental falls in facility settings include careful assessment of a patient’s physical environment, bedroom and bathroom setup, assistive devices, clothing, footwear, and other physically modifiable potential risk factors. Steps to minimize risk of accidental falls include:
- Providing patients with nonslip, comfortable, well-fitting footwear
- Keeping floor surfaces clean and dry and promptly cleaning any spills
- Providing sturdy handrails in bathrooms, rooms, and hallways
- Keeping wheelchair brakes locked whenever chair is stationary
- Use of night lights or other supplemental lighting
- Keeping patient rooms free of clutter
(Yang, 2023; Progress Lifeline, 2021)
Rehabilitation for Nonvestibular Balance Deficits
Patients who have experienced more than one fall or who demonstrate any difficulty with initial balance or gait testing should likely be referred to physical therapy for further evaluation and treatment (Merck & Co., 2022a).
BALANCE RETRAINING
For balance deficits determined to be nonvestibular in nature, a physical therapist can provide a comprehensive evaluation and individualized treatment program. (For balance deficits due to specific vestibular dysfunction, see “Vestibular Rehabilitation” later in this course.)
A balance retraining program may include specific interventions to improve static and dynamic balance, reaction time, protective responses, proprioception, and the ability to perform balance tasks under varying environmental conditions—such as on soft surfaces, in high-distraction environments, or while simultaneously performing cognitive tasks.
A balance retraining program is highly specific to an individual’s unique functional strengths and deficits and may contain specific exercises and task to improve gait, balance, functional coordination, and strength. The following are examples of generalized exercises that help to improve or maintain balance:
- Standing march
- Standing three-way kicks
- Sidestepping
- Single-legged standing
- Sit-to-stands
- Tandem standing or walking
(APTA, 2023a; Physiopedia, 2023a)
Reactive balance training is a whole-body movement type of balance exercise aimed at improving static and dynamic balance, as well as an individual’s ability to react quickly to external balance challenges. A physical therapist applies deliberate, controlled pressure to different parts of a patient’s body (usually the hips or shoulders) from multiple different directions, progressively increasing in speed, to help develop protective stepping response (Physiopedia, 2023f).
Specific exercise recommendations and individualized programs should be made by clinicians with appropriate training and expertise and implemented under appropriate supervision.
OTAGO EXERCISE PROGRAM
Originally developed in New Zealand, the Otago Exercise Program (OEP) is one example of an evidence-based, home-based strength and balance retraining program. The program is carried out by physical therapists/physiotherapists and/or trained community providers such as nurses. The program consists of a number of face-to-face home visits, independent home exercise training, and phone support and includes specific balance and strengthening exercises. This program has been found to reduce rates of falls and death in older adults (particularly those over age 80) as well as being fairly straightforward to implement (Physiopedia, 2023e).
THERAPEUTIC EXERCISE
Rigorous evidence exists to indicate that exercise can help reduce risk of falls by up to 25% in community-dwelling older adults (Sherrington et al., 2020). Specific and progressive exercise regimens devised and supervised by a physical therapist target and address specific and individualized deficits that may contribute to falls.
In order to maximize benefit from therapeutic exercise interventions aimed at fall reduction, it is recommended that exercise programs be designed and taught by a trained professional, be specifically tailoring to an individual patient’s areas of weakness/need, be provided for at least four months’ duration, and contain a significant component of balance challenge (Merck & Co., 2022b).
Precautions and recommendations for specific exercise regimens are assessed on a case-by-case basis. While most older people are able to successfully engage in and benefit from some level of physical activity, the following conditions are considered absolute contraindications to exercise:
- Acute myocardial infarction (MI), within 2 days
- Ongoing unstable angina
- Uncontrolled cardiac arrhythmia with hemodynamic compromise
- Active endocarditis
- Symptomatic severe aortic stenosis
- Decompensated heart failure
- Acute pulmonary embolism, pulmonary infarction, or deep vein thrombosis
- Acute myocarditis or pericarditis
- Acute aortic dissection
- Physical disability that precludes safe and adequate exercise
(Merck & Co., 2022b)
COMMUNITY-BASED ACTIVITY PROGRAMS
A number of community-based programs (such as Pilates, tai chi, or adaptive yoga) have been shown to help maintain or improve mobility and balance. Any engagement in a community health program for balance purposes should only be undertaken after discussion with and approval from an individual’s appropriate healthcare provider.
AQUATICS
Water-based programs allow the patient to perform challenging exercises characterized by lower impact, increased resistance and buoyancy, and reduced fear of falling (as may occur with land-based exercise programs). The viscosity of water creates increased drag and sensory stimulation, and functional gains in balance made during exercises practiced in the water may be transferrable to land-based situations. Though more research is needed, there is some evidence to suggest that participating in aquatic exercise programs may be associated with increased balance and decreased risk of falls (Nissim et al., 2020; Inverarity, 2022). Aquatic therapy is provided in a supervised setting by a physical or occupational therapist and is tailored to an individual patient, while aquatic exercise is a more generalized water-based exercise program (often in a group setting) offered in a community setting.
GAIT TRAINING
An atypical or impaired gait pattern may increase an individual’s risk of falling. A physical therapist can provide a comprehensive gait evaluation, including an analysis of an individual’s walking speed, step length, and step symmetry (or lack thereof) as well as evaluation and treatment of any specific gait abnormalities (e.g., antalgic, ataxic, steppage, Parkinsonian, etc.). The treatment of gait deviations may include:
- Specific pre-gait training activities (standing in place, side-to-side weight-shifting, stepping practice)
- Specific gait training activities (retraining how to walk, individualized to each patient)
- Selective neuromuscular re-education
- Balance and coordination retraining
- Evaluation for orthotic, splinting, or assistive device needs
(APTA, 2023b)
VIRTUAL REALITY AND VIDEO GAMES
Virtual reality (VR) is an emerging area in fall management and involves the use of computerized technology to provide patients with simulated experiences. Repetitive, task-oriented training is shown to help increase synaptic strength, positively affect nerve transmission, and enhance neuroplasticity. Training in VR environments can lead to the maintenance and transfer of individual motor skills, which is an important feature of motor skills learning and the basis of real-world behavior. VR therapy has become an increasingly accepted part of many rehabilitation programs.
A growing body of research supports the use of VR programs and exercises to help improve balance and reduce fall risk in older adults. In a randomized-control trial of 60 nursing home–dwelling residents, participating in two weekly 30- to 45-minute sessions of Xbox VR exercises for six weeks resulted in significantly increased Berg Balance and Timed-Up-and-Go scores, as well as deceased fear of falling, compared to control groups who received routine, non-VR exercises (Wu et al., 2022; Zahedian-Nasab, 2021).
Rehabilitation for Vestibular Dysfunction
Vestibular dysfunction is a common contributor to balance-related issues and falls. An estimated 35.4% of all adults in the United States have some degree of vestibular dysfunction, including 75% of adults over age 70 and more than 85% of adults over age 80. When left unaddressed, vestibular hypofunction can result in subjective dizziness/imbalance, blurred vision with head movements, and postural instability, and the incidence of falls in those with vestibular hypofunction is known to be greater than in age-comparable, community-dwelling healthy individuals (Hall et al., 2022).
Vestibular rehabilitation interventions target aberrant vestibular symptoms and resultant functional limitations and have been demonstrated to diminish dizziness, improve visual acuity, and reduce fall risk. Vestibular rehabilitation is an important subspecialty of physical therapy practice and study.
EXERCISE-BASED INTERVENTIONS
There are four primary components to the exercise-based approach used in vestibular rehabilitation:
- Gaze stability exercises: Exercises to promote vestibular adaptation involve head movements while focusing on an object that may be moving or stationary. Exercises to promote substitution involve the development of alternative strategies (such as smooth-pursuit eye movements or central preprogramming of eye movements) in order to help compensate for deficiencies in vestibular function.
- Habituation exercises: Involves systematic and repeated exposure to symptom-provoking stimuli, with the goal of reducing symptoms over time as the vestibular system becomes gradually accustomed to the stimuli. Examples include optokinetic stimuli, which uses repeated moving patterns, and virtual reality, which puts patients into virtual and visually challenging environments.
- Balance and gait training: Designed to use visual and somatosensory cues as compensation for vestibular deficiencies, this component of vestibular rehabilitation may include balancing exercises under enhanced or altered conditions (such as under distraction, with altered visual input, on foam or moving surfaces, with altered base of support, etc.). Gait activities may be executed while turning the head or performing additional tasks in order to increase challenge. Virtual reality and/or gaming technology may be employed.
- Endurance training: While not an effective treatment for vestibular dysfunction on its own, general endurance training is often included in a vestibular rehabilitation program because many people affected by vestibular dysfunction may self-limit their physical activities in order to avoid eliciting symptoms.
(Hall et al., 2022)
When vestibular impairments significantly affect an individual’s ability to meaningfully engage in preferred roles, activities, and/or occupations, occupational therapists may also work with patients to modify, remediate, and/or adapt as needed to help affected individuals maximize their participation, performance, self-efficacy, and perceived quality of life (AOTA, 2017b).
MANUAL TECHNIQUES FOR BENIGN PAROXYSMAL POSITIONAL VERTIGO (BPPV)
One of the most common causes of vestibular dysfunction, BPPV is a condition that occurs when small calcium carbonate crystals (called canaliths or otoliths) move within the semicircular ear canals, leading to dizziness and visual disturbance and increase the risk of falling (VEDA, 2023e). The diagnostic and treatment process for BPPV differs from other vestibular dysfunctions and is generally more focused on specific manual techniques to locate and reposition displaced canaliths.
Diagnosis with Dix-Hallpike Test
The Dix-Hallpike maneuver is a manual test performed to help clinicians determine which specific semicircular canal contains displaced canaliths, as well as whether they are in the canals themselves (canalithiasis) or trapped in the cupola of one of the canals (cupulolithiasis) (VEDA 2023f). To minimize the risk of neck/back injury or worsening of symptoms, this testing maneuver—as well as any of the following treatment techniques—should only be performed by clinicians with appropriate training. The general test progression is as follows:
- The patient is positioned on the examination table in long-sitting, with the examiner in front of them. The examiner rotates the patient’s head to one side and helps the patient lie quickly with their head hanging off the table in 30° of cervical extension (while maintaining rotation).
- The examiner asks the patient to look at their nose and simultaneously watches the patient’s eyes for signs of elicited nystagmus. Appearance and timing of any nystagmus can help identify whether the patient’s vertigo is of central (CNS) or peripheral (inner ear) origin.
- The patient sits up and is given time to recover from any symptoms elicited during the test. The test is then repeated with the patient’s head turned in the opposite direction.
(Physiopedia. 2023g)
Canalith Repositioning Techniques
If testing indicates the presence of BPPV, the following treatment measures may be indicated to attempt to reposition displaced canaliths out of the semicircular canals. Repositioning techniques have been found to relieve symptoms in a majority of patients with BPPV, although recurrence of symptoms may occur (MFMER, 2023a). Detailed instruction in vestibular rehabilitation is beyond the scope of this course, but the following is a list of more commonly used manual repositioning techniques.
- Modified Epley’s maneuver/canalith repositioning maneuver (CRP): Used to treat BPPV occurring in the anterior or posterior semicircular canals; intended to relocate free-floating canaliths out of the canals in order to reduce or eliminate vertigo
- Semont-Liberatory maneuver: Used to redirect unattached canaliths out of the posterior semicircular canal and into the utricle
- BBQ roll: Used to treat BPPV caused by canaliths in the lateral semicircular canal
- Brandt-Daroff exercises: Adjunct treatment to the above clinician-administered techniques; may be taught to a patient to perform independently at home
(Physiopedia, 2023g)
Addressing Environmental Safety Hazards in the Home
Falls that occur at home are often the result of environmental factors that may be easy to overlook but comparatively simple to address. Occupational therapists are specifically skilled in helping individuals identify and address potential safety hazards in the home that may increase the likelihood of a fall (AOTA, 2017a).
Specific steps that may improve environmental safety in a patient’s home may include:
- Ensuring that stairs have secure handrails (on both sides, if possible)
- Ensuring that lighting is appropriate and sufficient
- Installing grab bars beside the toilet and inside/outside the shower
- Using nonskid mats or strips on any surfaces that may become wet
- Removing throw rugs (or securing with appropriate, double-sided tape)
- Keeping a phone/charger beside the bed and consider carrying a charged phone with you at all times
- Keeping frequently used kitchen items (dishes, pans, utensils, etc.) in easy-to-reach cabinets or shelves
- Minimizing clutter, which may present trip hazards
- Taping down or bundling up wires away from main walking paths
(NIA, 2023)
ADL Training
Limitations in one’s ability to perform basic activities and instrumental activities of daily living (ADLs and IADLs)—such as dressing, meal preparation, toileting—may lead to increased risk of falling. Occupational therapists (OTs) are the clinical experts in the evaluation and management of ADL deficits, and a referral to an occupational therapist should be considered if any concerns exist regarding an individual’s functional abilities in these areas.
Occupational therapists work with patients to identify specific ADL and IADL deficits and strengths and assist individuals to design safe and beneficial daily activity programs based on what a patient enjoys (e.g., gardening or walking to promote balance/endurance). OTs can also work with patients at a highly individualized level to help break the cycles of inactivity that can result from fear of falling and, if unaddressed, can increase odds of falling due to decreased physical functioning (AOTA, 2012).
Examples of therapeutic interventions to help address ADL deficits include:
- Functional exercises geared specifically toward performance of ADLs (reaching, stepping up/down, practicing shower transfers, etc.)
- Home safety modifications
- Training a patient/client in the use of specific assistive devices (reachers, tub transfer chairs, dressing aides, etc.)
FUNCTIONAL COGNITION AND FALL PREVENTION
Functional cognition is how an individual utilizes and integrates their thinking and processing skills to accomplish everyday activities. Occupational therapists are experts in measuring functional cognition, which encompasses assessment of everyday task performance. Early identification of performance-based cognitive impairments then allows for the timely implementation of an occupational therapy care plan. The plan can include environmental and personal care supports necessary to prevent harmful events that commonly happen during routine activities for patients with cognitive impairments—for example, falls due to problematic sequencing during bathing or dressing (AOTA, 2021).
LIFESTYLE INTEGRATED FUNCTIONAL EXERCISE
There is some research to indicate that Lifestyle Integrated Functional Exercise, which works to embed exercise into daily activities, can be beneficial in reducing falls, reducing fall risk, and improving self-efficacy with regard to managing fall risk. Evidence suggests that dual-task or multi-task activities, which combine both cognitive and motor components, may be especially beneficial (Jansen et al., 2021).
Devices to Reduce Fall Risk or Injury
There are a number of items—some commonly available and others more specialized—which can help reduce risk of falls if selected and used correctly. Three general categories of such devices include environmental, surveillance/monitoring, and injury prevention.
ENVIRONMENTAL SAFETY DEVICES
There are a number of devices that may be employed to improve environmental safety—both in clinical and home/community settings—and help mitigate the risk of falls in commonly utilized areas of the home. Some examples include:
- Handrails for both sides of stairways (should be sturdily attached)
- Nonslip materials on treads of uncarpeted steps and in the shower
- A raised toilet seat or 3-in-1 commode
- Grab bars for shower or tub
- Shower seat or tub transfer bench
- Hand-held showerhead to allow bathing while seated
(MFMER, 2023b)
SURVEILLANCE/MONITORING DEVICES
Various devices and technologies are available to monitor patients or individuals at increased risk of falling. Such devices are frequently used in clinical or residential care settings, and some may also be used in a home-based setting to assist caregivers of at-risk individuals. Examples of surveillance devices used in fall prevention include bed alarms, pressure-sensing chair alarms, clip-on personal alarms, wall-mounted motion sensors, and video monitoring equipment.
However, available evidence is somewhat mixed regarding the safety and efficacy of patient monitoring devices of this nature. In particular, a recent systemic review and meta-analysis of patient monitoring devices in the hospital setting actually showed an increase in patient falls when bed or chair alarms were used (versus control groups), in part because sensors placed on beds or chairs do not offer a warning if the patient moves away from the sensor. Portable/wearable monitoring devices, in contrast, were found to be a more viable adjuvant to individualized patient safety plans (Cortés et al., 2021).
Recent years have also brought a host of newer technologies geared toward improving the safety of older adults in the home setting, such as remote data collection of geolocation and/or physiologic data, alarm systems trigged when a fall occurs, and other app-based monitoring systems and wearable or nonwearable sensors. While promising in nature, more evidence is needed to more fully determine the efficacy of these new technologies in preventing falls in the home-based setting (Pech et al., 2021).
INJURY-PREVENTION DEVICES
Despite clinicians’ best efforts, a patient/client fall is not always avoidable. When falls are anticipated despite best practices and vigilant staff and/or caregiver intervention, a number of specialized devices may help mitigate the potential for fall-related physical injury.
As with any specialized device, it is important to carefully determine the proper device and/or strategy for each individual patient and to train staff and caregivers in its correct usage. Up-to-date and standardized care plans, routine in-service training, and appropriate staff orientation and caregiver training can help optimize the safe use of injury-prevention devices and strategies.
Injury-prevention devices provide an environment that minimizes fall potential and/or fall-related injury. Examples include:
- Flooring/matting: Compliant floors or matting provide a softer, shock-absorbing surface that may prevent or minimize risk of injury from a fall. Floor matting is relatively cost effective, portable, and easily cleaned. Mats with beveled edges and luminescent strips may offer increased safety to both patients/clients and staff/caregivers. Floor matting should be in place when a patient is unattended (such as at night) and rolled up during direct patient care (Elderly Fall Prevention, 2023).
- Hip protectors: These garments, available as slip-on briefs or pants, have special padding at the lateral hip areas, which can provide cushioning at areas vulnerable to injury and/or fracture from a fall. Designed for use by one patient only, hip protectors are washable, relatively inexpensive, and may be indicated particularly for frail patients. Studies suggest that the use of hip protectors reduce the risk of hip fractures in older adult patients residing in nursing home or residential care settings (Nolan et al., 2022).
- Helmets/protective caps: These protect the head from falls-related impact and may be full-coverage, headband style (either stand-alone or embedded into other headwear) or involve adding padding into an existing piece of headwear (such as a baseball cap). Compared to helmets used for sporting activities, there is a comparative paucity of safety engineering standards with regard to protective headgear for older adults and what research does exist indicates a wide range in impact attenuation among current devices and also notes that existing options appear to be more effective against back-of-head impacts (Martel et al., 2021).
- Low-floor beds (no longer recommended): Specialized beds that keep the patient positioned as low to the ground as possible in order to mitigate risk of injury in the event of a fall from bed. While these beds were commonly used in the past, more recent research indicates that they may not reduce falls and may even contribute to increased falls incidence in older adults. Therefore, the most current clinical practice guidelines do not recommend the use of low-floor beds for the purpose of falls prevention (Schoberer et al., 2022).
RESTRAINTS
Once common in clinical settings, the use of restraints is now deemed controversial and a measure of absolute last resort for the prevention of patient/resident falls. According to the American Medical Association Code of Ethics, a patient should never be restrained for convenience, as a punitive measure, or without a physician’s specific order (except in rare emergency cases). Additionally, a physician who deems restraint to be the only alternative should seek informed consent of a patient or surrogate, as well as explain the following:
- Why restraint is being recommended
- What type of restraint will be used
- Length of time for which restraint is intended to be used
It is imperative that the need for restraint be regularly reassessed and updated in the patient’s medical record (AMA, 2023).
A restraint is defined by the Centers for Medicare and Medicaid Services as “any manual method, physical or mechanical device, material, or equipment that immobilizes or reduces the ability of a patient to move his or her arms, legs, body, or head freely; or a drug or medication when it is used as a restriction to manage the patient’s behavior or restrict the patient’s freedom of movement and is not a standard treatment or dosage for the patient’s condition” (ACEP, 2020).
Examples of physical restraints utilized for fall prevention (only as an absolute last resort) may include hand mitts, limb restraints, vests, or belts. Examples of chemical restraints may include benzodiazepines or antipsychotic medications (Shuwarger, 2021).
CASE
Ms. Lupe Morales, an active 75-year-old woman, was walking briskly across the grocery store parking lot when she tripped over a curb, lost her balance, and fell onto her left side. Bystanders called EMS, and Ms. Morales was transported to nearest emergency department (ED) with the presenting complaint of severe hip pain. She was examined by the ED physician, who ordered X-rays that showed a femoral fracture requiring surgical intervention, and Ms. Morales subsequently underwent an open-reduction internal fixation (ORIF) procedure and was eventually cleared to perform functional mobility with weight bearing as tolerated (WBAT), with appropriate assistance and instruction from clinical staff.
During the acute-care phase of her recovery, clinicians from multiple disciplines were involved in Ms. Morales’s postsurgical care, early-stage rehabilitation, patient education, and discharge planning. Her primary care nurse played a key role in helping to coordinate the interdisciplinary team’s interventions both pre- and post-surgery and monitored Ms. Morales’s pain level and medication needs throughout her hospitalization and early-stage rehabilitation. As Ms. Morales was considered to have an increased risk of falling—both because of her postoperative status and because of her initial injury mechanism—her primary care nurses ensured that all inpatient floor staff were aware of Ms. Morales’s fall precautions, made sure that her call button was always within reach, and reminded Ms. Morales not to attempt to get out of bed without assistance.
A physical therapist evaluated Ms. Morales’s functional mobility and worked with her on improving her ability to safely perform bed mobility, transfers, and negotiate several steps with handrail support, as well as instructing Ms. Morales in the safe and appropriate use of a front-wheeled walker for ambulating and prescribing lower-extremity strengthening and balance exercises under appropriate supervision. An occupational therapist evaluated Ms. Morales’s ability to perform ADLs such as dressing, bathing, and toileting and worked with her to devise safe strategies for performing these tasks, as well as discussing which tasks she liked to perform at home that might require safety adaptations. The hospital social worker helped Ms. Morales identify community resources and prepare for her eventual return home, and the nursing team helped coordinate interdisciplinary consults and recommendations while advocating for the patient’s overall and ongoing needs.
As the time approached for Ms. Morales to be discharged home, the care team expressed some concerns as to whether she would be able to safely navigate her home environment, as she lived alone in a one-story home with three steps to enter. The occupational therapist performed a home safety assessment at Ms. Morales’s home and made several recommendations for safety modifications, including the addition of grab bars in the bathroom, removal of several throw rugs in the kitchen area, and the addition of a shower chair so that Ms. Morales could bathe with reduced risk of slips/falls. When the OT had determined that Ms. Morales could safely navigate her home environment with appropriate modifications, the team met and collectively agreed that Ms. Morales could be discharged to home with specific supports, including home health nursing, PT and OT evaluations, and Meals on Wheels, with a follow-up outpatient appointment scheduled with her orthopedist.
Discussion
Each member of the interdisciplinary team played a key role in helping Ms. Morales avoid falls and remain safe during her recovery by focusing on their specific areas of expertise. Communication and collaboration are key elements in maximizing the effectiveness of each discipline and of the care team as a whole when helping a patient recover from a fall-related injury and working to prevent additional falls.
CONCLUSION
Balance-related falls are a significant cause of injury-related mortality and disability, especially in older and/or otherwise compromised populations, and can significantly impact the quality of life of affected individuals and their loved ones. Preventable falls place a costly financial burden on healthcare systems, and effective prevention strategies and protocols are of high priority for clinicians and healthcare institutions wishing to provide the best quality of patient/client care and to mitigate potential consequences of preventable fall-related injuries.
The successful management of fall-related injuries and the prevention of additional falls require strong collaboration among the multidisciplinary healthcare team as well as the patient/client and family. A careful and detailed patient history and a comprehensive physical examination are key components to effectively identifying and addressing balance deficits and other risk factors that may lead to preventable falls. There are a number of evidence-based, standardized assessment tools used by clinicians to determine a patient’s risk of falling so that appropriate preventive measures may be undertaken. Home safety assessments may provide valuable additional information regarding environmental factors that can be modified to improve patient safety in their home setting.
By understanding the primary risks and causes of falls, together with the numerous medical conditions and environmental factors that can adversely affect balance, healthcare professionals work collaboratively with one another and patients and their caregivers to provide effective clinical and rehabilitative interventions and preventive measures. Both individual and institutional strategies may be employed to minimize the risk of preventable falls, thereby creating a safer environment for patients and clinicians alike.
RESOURCES
Check for safety: A home fall prevention checklist for older adults (CDC)
Global guidelines for falls in older adults
Home safety self-assessment checklist
REFERENCES
NOTE: Complete URLs for references retrieved from online sources are provided in the PDF of this course.
Alghadir AH, Iqbal ZA, Iqbal A, Ahmed H, & Ramteke SU. (2020). Effect of chronic ankle sprain on pain, range of motion, proprioception, and balance among athletes. Int J Environ Res Public Health, 17(15), 5318. doi:10.3390/ijerph17155318
American College of Emergency Physicians (ACEP). (2020). Policy statement: Use of patient restraints. https://www.acep.org
American Geriatrics Society (AGS). (2019). 2019 updated Beers criteria for potentially inappropriate medication use in older adults. Journal of the American Geriatrics Society, 67(4), 674–94.
American Medical Association (AMA). (2023). Use of restraints: Code of medical ethics opinion 1.2.7. https://www.ama-assn.org
American Occupational Therapy Association (AOTA). (2021). Role of occupational therapy in assessing functional cognition. https://www.aota.org
American Occupational Therapy Association (AOTA). (2019). Home safety and accessibility assessments. https://www.aota.org
American Occupational Therapy Association (AOTA). (2017a). Occupational therapy and prevention of falls. https://www.aota.org
American Occupational Therapy Association (AOTA). (2017b). Vestibular impairment, vestibular rehabilitation, and occupational performance. American Journal of Occupational Therapy, 71, 7112410055. doi.org/10.5014/ajot.2017.716S09
American Occupational Therapy Association (AOTA). (2012). Tips for living life to its fullest: Fall preventions for older adults. https://www.aota.org
American Physical Therapy Association (APTA). (2023a). 6 exercises to promote balance that you can do at home. https://www.choosept.com
American Physical Therapy Association (APTA). (2023b). Physical therapy guide to gait dysfunctions. https://www.choosept.com
American Physical Therapy Association (APTA). (2021). Physical therapy guide to balance problems. https://www.choosept.com
Bannister R. (1969). Brain’s clinical neurology (3rd ed.). Oxford University Press.
Centers for Disease Control and Prevention (CDC). (2023a). CDC compendium of effective fall interventions: What works for community-dwelling older adults (4th ed.). https://www.cdc.gov
Centers for Disease Control and Prevention (CDC). (2023b). STEADI—Older adult fall prevention. https://www.cdc.gov
Centers for Disease Control and Prevention (CDC). (2021). Facts about falls. https://www.cdc.gov
Centers for Disease Control and Prevention (CDC). (2020a). Keep on your feet—Preventing older adult falls. https://www.cdc.gov
Centers for Disease Control & Prevention (CDC). (2020b). Cost of older adult falls. https://www.cdc.gov
Centers for Disease Control and Prevention (CDC). (2020c). STEADI-Rx older adult fall prevention guide for community pharmacists. https://www.cdc.gov
Cortés OL, Piñeros H, Aya PA, Sarmiento J, & Arévalo I. (2021). Systematic review and meta-analysis of clinical trials: In-hospital use of sensors for prevention of falls. Medicine, 100(41), e27467. https://doi.org/10.1097/MD.0000000000027467
Elderly Fall Prevention. (2023). Reducing fall injuries with fall mats. https://elderlyfallprevention.com
Fehlberg EA, Lucero RJ, Weaver MT, McDaniel AM, Chandler AM, Richey PA, Mion LC, & Shorr RI. (2017). Impact of the CMS no-pay policy on hospital-acquired fall prevention related practice patterns. Innovation in Aging, 1(3), igx036. https://doi.org/10.1093/geroni/igx036
Florida Physical Therapy Association (FPTA). (n.d.). Create a fall prevention team. https://www.fpta.org
Hall CD, Herdman SJ, Whitney SL, Anson ER, Carender WJ, Hoppes CW, Cass SP, et al. (2022). Vestibular rehabilitation for peripheral vestibular hypofunction: An updated clinical practice guideline from the Academy of Neurologic Physical Therapy of the American Physical Therapy Association. Journal of Neurologic Physical Therapy, 46(2), 118–77. doi:10.1097/NPT.0000000000000382
Healthline Media. (2023). How to tell the difference between dizziness and vertigo. https://www.healthline.com
Healthy Aging Resource Group. (2023). FES-I. University of Manchester. https://sites.manchester.ac.uk/fes-i/
Inverarity L. (2022). The benefits of aquatic therapy. Verywell Health. https://www.verywellhealth.com
Jansen CP, Nerz C, Labudek S, et al. (2021). Lifestyle-integrated functional exercise to prevent falls and promote physical activity: Results from the LiFE-is-LiFE randomized non-inferiority trial. Int J Behav Nutr Phys Act, 18, 115. https://doi.org/10.1186/s12966-021-01190-z
Lee FS, Sararaks S, Yau WK, et al. (2022). Fall determinants in hospitalised older patients: A nested case control design – incidence, extrinsic and intrinsic risk in Malaysia. BMC Geriatr, 22, 179. https://doi.org/10.1186/s12877-022-02846-6
Martel DR, Tanel MR, & Laing AC. (2021). Impact attenuation provided by older adult protective headwear products during simulated fall-related head impacts. Journal of rehabilitation and assistive technologies engineering, 8, 20556683211050357. https://doi.org/10.1177/20556683211050357
Mayo Foundation for Medical Education and Research (MFMER). (2023a). Canalith repositioning procedure. https://www.mayoclinic.org
Mayo Foundation for Medical Education and Research (MRMER). (2023b). Fall prevention: Simple tips to prevent falls. https://www.mayoclinic.org
Merck & Co. (2022a). Falls in older people. Merck Manual Professional Version. https://www.merckmanuals.com
Merck & Co. (2022b). Exercise in older adults. Merck Manual Professional Version. https://www.merckmanuals.com
Mishra AK, Skubic M, Despins LA, Popescu M, Keller J, Rantz M, Abbott C, et al. (2022). Explainable fall risk prediction in older adults using gait and geriatric assessments. Front. Digit. Health, 4, 869812. doi:10.3389/fdgth.2022.869812
Montero-Odasso MM, Kamkar N, Pieruccini-Faria F, et al. (2021). Evaluation of clinical practice guidelines on fall prevention and management for older adults: A systematic review. JAMA Netw Open, 4(12), e2138911. doi:10.1001/jamanetworkopen.2021.38911
National Council on Aging (NCOA). (2021). Falls prevention conversation guide for caregivers. https://www.ncoa.org
National Institute for Health Care and Excellence (NICE). (2023). Falls in older people: Assessing risk and prevention. https://www.nice.org
National Institute on Aging (NIA). (2023). Preventing falls at home: Room by room. https://www.nia.nih.gov
Neuro-Optometric Rehabilitation Association (NORA). (2023). Dizziness and balance problems related to vision. https://noravisionrehab.org
Nissim M, Livny A, Barmatz C, Tsarfaty G, Berner Y, Sacher Y, Giron J, & Ratzon NZ. (2020). Effects of aquatic physical intervention on fall risk, working memory and hazard-perception as pedestrians in older people: A pilot trial. BMC geriatrics, 20(1), 74. https://doi.org/10.1186/s12877-020-1477-4
Nolan P, Tiedt L, Ellanti P, & McCarthy T. (2022). A description of novel uses of hip protectors in an elderly hip fracture population: A technical report. Cureus, 14(1), e21028. https://doi.org/10.7759/cureus.21028
Pech M, Sauzeon H, Yebda T, Benois-Pineau J, & Amieva H. (2021). Falls detection and prevention systems in home care for older adults: Myth or reality? JMIR Aging, 4(4), e29744. https://doi.org/10.2196/29744
Performance Health. (2023). The role of nurses in fall prevention. https://www.performancehealth.com
Physiopedia. (2023a). Balance. https://www.physio-pedia.com
Physiopedia. (2023b). Falls. https://www.physio-pedia.com
Physiopedia. (2023c). Activities-specific balance confidence scale. https://www.physio-pedia.com
Physiopedia. (2023d). Tinetti test. https://www.physio-pedia.com
Physiopedia. (2023e). Otago exercise programme. https://www.physio-pedia.com
Physiopedia. (2023f). Reactive balance training. https://www.physio-pedia.com
Physiopedia. (2023g). Benign paroxysmal positional vertigo. https://www.physio-pedia.com
Progress Lifeline. (2021). Three types of falls in older adults and how to manage them. https://www.progresslifeline.org
Prost E. (2021). Geriatric examination tool kit. University of Missouri, School of Health Professions, Department of Physical Therapy. https://geriatrictoolkit.missouri.edu
Reeves ND, Orlando G, & Brown SJ. (2021). Sensory-motor mechanisms increasing falls risk in diabetic peripheral neuropathy. Medicina (Kaunas, Lithuania), 57(5), 457. https://doi.org/10.3390/medicina57050457
Schoberer D, Breimaier HE, Zuschnegg J, Findling T, Schaffer S, & Archan T, the Guideline Development Group. (2022). Fall prevention in hospitals and nursing homes: Clinical practice guideline. Worldviews on Evidence-Based Nursing, 19, 86–93. https://doi.org/10.1111/wvn.12571 17416787
Schoene D, Heller C, Aung YN, Sieber CC, Kemmler W, Freiberger E. (2019). A systematic review on the influence of fear of falling on quality of life in older people: Is there a role for falls? Clin Interv Aging, 14, 701–19. doi:10.2147/CIA.S197857
Sherrington C, Fairhall N, Kwok W, et al. (2020). Evidence on physical activity and falls prevention for people aged 65+ years: Systematic review to inform the WHO guidelines on physical activity and sedentary behaviour. Int J Behav Nutr Phys Act, 17, 144. https://doi.org/10.1186/s12966-020-01041-3
Shirley Ryan Abilitylab. (2020a). Berg balance scale. https://www.sralab.org
Shirley Ryan Abilitylab. (2020b). Dizziness handicap inventory. https://www.sralab.org
Shirley Ryan Abilitylab. (2020c). Dynamic gait index. https://www.sralab.org
Shirley Ryan Abilitylab. (2020d). Falls efficacy scale—International. https://www.sralab.org
Shirley Ryan Abilitylab. (2020e). Four step square test. https://www.sralab.org
Shirley Ryan Abilitylab. (2020f). Functional independence measure. https://www.sralab.org
Shirley Ryan Abilitylab. (2020g). Functional reach test/modified functional reach test. https://www.sralab.org
Shirley Ryan Abilitylab. (2020h). Head-shaking nystagmus test. https://www.sralab.org
Shirley Ryan Abilitylab. (2020i). Two-minute walk test. https://www.sralab.org
Shuwarger M. (2021). Fall prevention and restraints. Level Up RN. https://www.leveluprn.com
Smiling Senior. (2023). Elderly mobility scale. https://www.smilingsenior.com
Sung YH. (2020). Upper cervical spine dysfunction and dizziness. J Exerc Rehabil, 16(5), 385–91. doi:10.12965/jer.2040612.306
Task Force on Global Guidelines for Falls in Older Adults (Task Force). (2022). World guidelines for falls prevention and management for older adults: A global initiative, Age and Ageing, 51(9), afac205. https://doi.org/10.1093/ageing/afac205
University of Scranton. (2020). Goniometry: Ankle dorsiflexion. https://www.scranton.edu
U.S. Centers for Medicare and Medicaid Services (CMS). (2022a). Hospital-acquired conditions. https://www.cms.gov
U.S. Centers for Medicare and Medicaid Services (CMS). (2022b). Hospital-acquired condition reduction program. https://www.cms.gov
Vestibular Disorders Association (VeDA). (2023a). The human balance system. https://vestibular.org
Vestibular Disorders Association (VeDA). (2023b). Your balance system. https://vestibular.org
Vestibular Disorders Association (VeDA). (2023c). Causes of dizziness. https://vestibular.org
Vestibular Disorders Association (VeDA). (2023d). Vestibular rehabilitation therapy (VRT). https://vestibular.org
Vestibular Disorders Association (VeDA). (2023e). Canalith repositioning technique for BPPV. https://vestibular.org
Vestibular Disorders Association (VeDA). (2023f). Benign paroxysmal positional vertigo (BPPV). https://vestibular.org
World Health Organization (WHO). (2021a). Falls. https://www.who.int/news-room/fact-sheets/detail/falls
World Health Organization (WHO). (2021b). Step safely: Strategies for preventing and managing falls across the life-course. https://www.who.int/teams/social-determinants-of-health/safety-and-mobility/step-safely
Wu J, Zhang H, Chen Z, Fu R, Yang H, Zeng H, & Ren Z. (2022). Benefits of virtual reality balance training for patients with Parkinson disease: Systematic review, meta-analysis, and meta-regression of a randomized controlled trial. JMIR serious games, 10(1), e30882. https://doi.org/10.2196/30882
Yang E. (2023). 3 different types of elderly falls explained. OK2StandUp. https://www.ok2standup.com
Zahedian-Nasab N, Jaberi A, Shirazi F, & Kavousipor S. (2021). Effect of virtual reality exercises on balance and fall in elderly people with fall risk: A randomized controlled trial. BMC Geriatr, 21, 509. https://doi.org/10.1186/s12877-021-02462-w





Customer Rating
4.9 / 1009 ratings