Incontinence
Patient Care and Treatment
Online Continuing Education Course
Course Description
Discuss different types of urinary and bowel incontinence in male and female patients. Learn about symptoms, causes, patient assessment, care, and treatment. This CEU course is applicable to nursing, OT, and PT.
Course Price: $28.00
Contact Hours: 3.5
Course updated on
February 2, 2024
"I love that you can download the content to read and study at your own pace and then return to take the test. Very informative and affordable!" - Kathy, RN in Pennsylvania
"Excellent website. The most organized I have found so far. Will use every year from now on! Thank you!" - Kourtney, RN in West Virginia
"I love Wild Iris! The course material is interesting and engaging. The courses are challenging and relevant. I actually learn something when I take your classes. Thank you." - Tamara, RN in California
"I always enjoy learning with this educational site. I recommend it to other agencies and my fellow nurses. Thank you for being a fair, professional learning site." - Genina, RN in New York
Incontinence
Patient Care and Treatment
Copyright © 2024 Wild Iris Medical Education, Inc. All Rights Reserved.
LEARNING OUTCOME AND OBJECTIVES: Upon completion of this continuing education course, you will have increased your understanding of incontinence assessment and treatment. Specific learning objectives to address potential knowledge gaps include:
- Discuss the impact of incontinence on individuals.
- Identify the different types and causes of incontinence.
- Describe the process of conducting a urinary incontinence assessment.
- Summarize treatment options for urinary incontinence.
- Discuss assessment, diagnosis, and interventions for bowel incontinence.
TABLE OF CONTENTS
INTRODUCTION
Incontinence can be a silent and debilitating condition. It can affect individuals in all age groups and walks of life. The classic picture may be of elderly patients in nursing facilities struggling with frequent episodes of bowel and bladder incontinence and wearing diapers. However, this does not tell the full story. Many individuals who are pursuing careers, participating in family activities, and involved in their communities struggle with incontinence on a daily basis.
The definition of urinary incontinence is the inability to control the time and place of voiding, resulting in the involuntary loss of urine. One quarter to one third of people in the United States experience urinary incontinence (UCF, 2023). The rate is 50% or more among nursing home residents, and information from caregivers indicates that 53% of homebound older adults suffer from urinary incontinence (Tran & Puckett, 2023).
The definition of bowel incontinence, also known as fecal incontinence or accidental bowel leakage, is loss of normal control of the bowel. Bowel incontinence is associated with diminished awareness of rectal fullness and diminished ability to control the urge to defecate or pass gas until an appropriate time and place is available.
Data shows that between 7% and 25% of community-living adults experience some degree of fecal incontinence. Women over 40 years of age report more issues with fecal incontinence resulting from pelvic floor problems or obstetrical injuries. However, it is believed that the data available on the prevalence of bowel incontinence do not capture the extent of the problem due to underreporting (WOCN, 2021; UCF, 2023).
Incontinence is not merely a medical problem. The complications associated with urinary and bowel incontinence can seriously impact the physical and emotional well-being of those affected with either or both of these conditions. In a systematic review of 23 studies with close to 25,000 participants, it was found that urinary incontinence is a significant factor in a reduced quality of life. The embarrassment reported by participants resulted in lifestyle changes including less physical activity and the development of depression and anxiety (Pizzol et al., 2021).
Results from quality-of-life surveys also show that bowel incontinence has a negative impact on nearly every part of an individual’s life, including friendships, marriage, sexuality, employment prospects, and the capacity to take part in exercise. Bowel incontinence has been found to be a consistent factor in elderly placement in care facilities. Bowel incontinence is also a leading cause of falls in the elderly population (WOCN, 2021).
Patients’ bladder and bowel health, particularly incontinence, are often neglected by healthcare professionals. Unless the clinician asks about bowel and bladder health, especially problems with incontinence, the patient is often too embarrassed to bring it up. Older patients who are otherwise healthy may also consider incontinence an expected outcome of aging.
TYPES OF URINARY INCONTINENCE
In simplest terms, urinary continence means that a person stays dry and experiences no leakage of urine regardless of the activity the person is engaged in. Continence means that, even with a full bladder and a “need” to go, the person can take the necessary steps to void without rushing and without urine leakage.
The normal pattern for urination is six to eight times per 24 hours. Those under the age of 65 years can expect to void perhaps once during the night. For those over 65 years, the pattern is one to two voids during the night. When the bladder starts filling, the first signal to void usually occurs when there is 150–200 cc of urine present; at this stage the detrusor muscle of the bladder begins to stretch. It is possible to ignore this first signal to void if the time and place are not convenient. When the bladder capacity reaches 400–600 cc of urine, it is time to void (WOCN, 2021; Gill, 2022).
It is important for clinicians to remember that urinary incontinence is not a disease itself; it is a symptom of some other malfunction in the human body. Early diagnosis is essential to determine whether there is an underlying serious medical condition causing urinary incontinence. Some of those conditions include multiple sclerosis (MS), Parkinson’s disease, and tumor. Approximately 80% of individuals with MS develop some form of urinary incontinence (WOCN, 2021).
Urinary incontinence can be divided into several different types, with different underlying factors associated with each type.
Acute or Transient Urinary Incontinence
Acute or transient urinary incontinence occurs in individuals with no previous history of urinary incontinence. It usually comes on suddenly and lasts less than six months. This type of urinary incontinence is caused by reversible factors such as:
- Urinary tract infection
- Medications
- Stool impaction
- Atrophic urethritis and vaginitis
(WOCN, 2021)
URINARY TRACT INFECTION (UTI)
Urinary tract infections are a major cause of transient incontinence. They can occur in any age group and gender, but they are more common in females. Evidence shows that by the age of 35 years, 50% of women have experienced at least one UTI. Urinary tract infections can develop in the kidneys, bladder, or urethra. The most common causative organism is E. coli, which causes inflammation of the bladder wall and urethra.
A change in mental status, such as sudden confusion in elderly patients, along with a new onset of urinary incontinence is a primary symptom of a UTI. Other symptoms of a UTI include:
- Urgency to void
- Increased frequency of urination
- Pain with urination
- Cloudy-colored urine, often with a malodor
- Blood in the urine (hematuria) (which can also indicate a more serious condition)
- Fever
Diagnosis of a UTI can be made by a urine culture and is treated by antibiotic therapy. Patients are advised to stay well hydrated, and female patients are advised against using any female hygiene products that could irritate the urethra (NAFC, 2022c).
MEDICATIONS
Medications can frequently result in urinary incontinence. The medications most commonly associated with urinary incontinence are diuretics. Diuretics can be responsible for the rapid production of large amounts of urine, which can result in incontinent episodes, especially in patients with compromised mobility. This can be of particular concern for older adults.
Other categories of medications can cause urinary incontinence.
- Alpha blockers used to treat high blood pressure can cause the muscles surrounding the bladder neck to relax, resulting in urine leakage.
- Antipsychotics, antihistamines, and tricyclic antidepressants can lead to urinary retention and overflow incontinence (involuntary leakage of a small amount of urine from an overdistended bladder).
- Calcium-channel blockers used for the treatment of high blood pressure can cause urinary retention and overflow incontinence.
Since each patient will have an individualized response to medications, it is important for clinicians to be aware of a patient’s medications and to discuss the possibility of urinary incontinence. If incontinence does occur, the healthcare provider may be able to make medication adjustments (SFC, 2023b).
STOOL IMPACTION
Constipation can result in urinary incontinence. The bladder and rectum are in close proximity in the restricted space in the bony pelvis, and fecal impaction causes the bowel to become distended, leading to obstruction of the bladder neck. Obstruction of the bladder neck can make it difficult for the patient to urinate, causing a buildup of urine in the bladder that results in overflow incontinence. There is also a possibility that straining during bowel movements, which is common with chronic constipation, may result in weakening of the pelvic floor muscles. Clinicians should always inquire about bowel health in conjunction with bladder health, especially when there is an issue with urinary incontinence (WOCN, 2021).
ATROPHIC URETHRITIS
In women, urinary continence is in part dependent on coaptation of the walls of the urethra (when the urethral walls collapse together). The urethra in females is about 4 cm in length and made up of four layers, which supports urethral closure or coaptation. Diminished estrogen supplies, especially in older females, leads to dryness and thinning of the urethral tissue (atrophic urethritis), lessening coaptation and causing urinary leakage. Treatment with estrogen vaginal suppositories or creams can help to counteract this problem (WOCN, 2021).
Urge Urinary Incontinence
Urge urinary incontinence is the most frequently occurring type of urinary incontinence and the result of an overactive detrusor muscle (a smooth muscle that forms part of the bladder wall). When the detrusor muscle contracts, the bladder empties.
Urge incontinence is caused by an abnormal sensitivity and contractibility of the bladder wall, but the exact mechanism is not known. Possible causes include changes in the levels of neurotransmitters, with heightened stimulation of sensory fibers indicating early bladder fullness. In adults over 65, the bladder is more susceptible to untimely contractions. The amount of urine lost can vary from small to considerable (WOCN, 2021).
The most significant finding in urge incontinence is an overpowering urge to void together with the involuntary loss of urine. Urge incontinence is sometimes referred to as the “key-in-lock” syndrome, in which the bladder may begin to contract when the individual knows they will soon be able to reach the toilet and they will be overcome by a sudden urge to void. Triggers for urge incontinence also include the sound of running water or making a position change (WOCN, 2021; Khatri, 2022).
Other symptoms of urge incontinence are needing to void frequently and voiding during the night (nocturia). Nighttime voiding is particularly problematic for older adults, causing disruption in sleep and increasing the risk of falls.
Urge urinary incontinence can be found in women of any age group but is more common in older women. Men are more prone to urge urinary incontinence rather than stress urinary incontinence. Approximately 80% of men with urinary incontinence suffer from urge incontinence, compared to women with incontinence problems, among whom about 30% have urge incontinence (Mayo Clinic, 2023a).
Stress Urinary Incontinence
With stress urinary incontinence, the patient typically complains of involuntary urine leakage with exertion (e.g., sneezing, coughing, laughing, running, or lifting). This type of incontinence is also known as activity-associated incontinence.
Stress incontinence is primarily caused by the inability of the sphincter muscle to sustain closure when the patient is performing activities that increase abdominal and bladder pressure, referred to as sphincter insufficiency. This, in turn, leads to a partially open urethra, which allows urine to escape (WOCN, 2021).
During a first pregnancy, greater than one third of women experience temporary stress incontinence. During succeeding pregnancies, greater than three quarters of women experience stress incontinence. However, the majority of women who develop urinary incontinence during pregnancy regain full continence after the delivery as the birth canal heals. Only around 5% of these women still experience stress incontinence a year after the birth (Rosenman, 2023).
Weak pelvic floor muscles are a secondary contributor to stress urinary incontinence. In particular, the levator ani muscle (which lends support to the bladder from below) in females is susceptible to damage during childbirth. Lengthy and difficult childbirth can cause weakening of the pelvic muscles. Forceps deliveries increase the risk of damage to pelvic floor muscles (Rosenman, 2023).
Stress urinary incontinence can have a debilitating impact on women’s lives and activities. Women with stress urinary incontinence are acutely aware that their control over urination has been greatly diminished, and a simple act such as walking across a room could result in urine leakage.
Stress urinary incontinence is less common in males, affecting less than 10% of men with urinary incontinence. Men most often experience stress urinary incontinence after surgery for prostate cancer or for an enlarged prostate (Mayo Clinic, 2023b).
Mixed Urinary Incontinence
Patients with mixed urinary incontinence have symptoms of both stress incontinence and urge incontinence. It combines bladder muscle dysfunction resulting in bladder overactivity with sphincter dysfunction resulting in urine leakage associated with urgency (WOCN, 2021). Usually, the symptoms of one type of incontinence (stress or urge) are more severe than the other.
Mixed urinary incontinence is a common problem, and the majority of women with incontinence have mixed incontinence. It is usually more prevalent among older women. Mixed urinary incontinence is also found in men who have had their prostate gland removed or undergone surgery for an enlarged prostate. As with women, mixed urinary incontinence occurs in older men (Harris & Riggs, 2023).
Functional Incontinence
In most instances of functional incontinence, the bladder, urethra, and sphincter mechanism is functioning correctly, and the incontinence results from problems outside the urinary tract. These external problems impede the person’s ability to respond appropriately to the need to void. The most frequent types of impairments resulting in functional incontinence are:
- Impaired mobility
- Impaired cognitive function
Impaired mobility can pose several difficulties for individuals, including an inability to reach the restroom in time to void and a hampered ability to prepare for voiding. In some cases, the person may be dependent on others for assistance with toileting, and if assistance is not readily available, incontinence may occur.
Impaired cognition can have several causes, such as advanced dementia. In cases of cognitive impairment, the person does not recognize the urge to void or is unable to recall the stages of voiding (WOCN, 2021).
Medications can also lead to functional incontinence, for example, a person with some degree of impaired mobility who also takes a diuretic medication to treat hypertension or congestive heart failure. The diuretic medication will increase the volume of urine, and the urgency to void along with the extra time needed to reach the restroom may result in episodes of incontinence (SFC, 2023b).
Neurogenic Bladder
Neurogenic bladder is caused by a lack of neuron regulation of the lower urinary tract mechanism. The most common finding in neurogenic bladder is a lesion located between the sacral cord and the brain. These lesions occur most frequently in persons with spinal cord injury and conditions such as multiple sclerosis.
Patients with neurogenic bladder have no sensory awareness of bladder filling. They are unable to instigate voiding and have lost control over the urinary sphincter. This inability to maintain continence is due to a loss of communication between the cerebral cortex, the brainstem, the bladder, and the sphincter muscle. Since the patient has lost voluntary control over voiding, bladder emptying happens due to reflex arc responding to bladder filling.
Patients with neurogenic bladder are at risk for developing a severe problem called detrusor sphincter dyssynergia, which is characterized by failure of the sphincter to relax in response to contraction of the detrusor muscle (WOCN, 2021).
Peyronie’s Disease
The name of this condition is somewhat misleading, since it is not an actual disease but a condition that results from injury or damage to the penile tissue. The consequence of this injury is the development of an irregular twist or curvature of the penis (UCF, 2020). Peyronie’s disease is caused by a problem with wound healing, leading to an accumulation of collagen tissue on the shaft of the penis. This can occur after a single traumatic event or due to frequent minute injuries during sexual intercourse. Other causes include:
- Vigorous sports activities
- Autoimmune conditions, such as scleroderma
- Diabetes
- Heredity
(NIDDK, 2020)
Scar tissue builds up on the surface of the penis and leads to a change in the shape of the penis over a period of time. The condition usually stabilizes after a period of 3 to 12 months (Mayo Clinic, 2020). This gradual change distinguishes Peyronie’s disease from a hereditary curvature of the penis, which remains constant.
Apart from urinary incontinence, the other symptoms of Peyronie’s disease include:
- Firm lumps on the shaft of the penis
- Shortening of the penis
- Erectile dysfunction
- Pain with or without an erection
(NAFC, 2022d)
Peyronie’s disease is estimated to affect around 4 out of every 100 men between the ages of 40 and 70 years. It is a rare occurrence in younger men, but it has been found in men in their 30s. The prevalence of the condition may be higher than what is actually seen in clinical practice since many men maybe too embarrassed to discuss the condition with their healthcare provider (NAFC, 2022d). In cases where men are adversely affected by the disease, drug therapy may help during the acute phase. Penile injections appear to work better. Surgery is only performed in cases where the disease is so severe that it makes sexual intercourse difficult (UCF, 2020).
Incontinence in Children
Urine leakage is the most frequently occurring urine symptom in children and teenagers. Problems with urinary incontinence can result in emotional and mental health issues that may be revealed as behavioral disorders in children. Teenagers who had problems with urinary incontinence during their childhood can develop pervasive concerns about continence and bladder control (WOCN, 2021).
Children usually become continent between the ages of 2 and 4 years, although it is highly individualized. Research has demonstrated a 7.8% incidence of urinary incontinence in children who are 7-1/2 years old, with the possible consideration that urinary incontinence could have a genetic link.
The spinal Galant reflex assists with the process of delivery, facilitating hip movements to pass through the birth canal. About six months after birth, this reflex should then integrate and lay dormant. However, the continuation of the spinal Galant reflex beyond this period is associated with bedwetting after the age of five years (Brain Balance, 2023).
Urinary incontinence, or enuresis, in children has two types. Primary enuresis occurs when the child never gains continence. Secondary enuresis refers to the onset of urinary incontinence in children who have achieved continence for at least six months. This type of incontinence can be associated with an unusually stressful event, such as the birth of a sibling or parents divorcing.
For most children, problems with bladder control resolve as they get older. Urinary incontinence has a spontaneous resolution rate of over 15% annually. Parents and caregivers, although frustrated with the problem, can be educated that incontinence in children is not due to laziness, heedlessness on the part of the child, or problems with toilet training. The majority of children who experience incontinence are emotionally and physically normal (WOCN, 2021).
Conditions that can lead to incontinence in children include:
- Urinary tract infection
- Vesicoureteral reflux (VUR) (retrograde flow of urine from the bladder to the kidneys)
- Constipation
- Diabetes
- Structural malformation of the urinary tract, such as narrowing of the urethra
- Arousal disorder (inability to respond to physical signals that urination is needed)
- Sexual abuse
Incontinence in Adults During Sleep
Bedwetting is an atypical condition related to urinary continence, and it occurs in both children and adults. Adult bedwetting, also known as sleep enuresis, can happen for many reasons, including depression and anxiety. Approximately 1% to 2% of adults have problems with bedwetting. There are several factors that can be related to sleep enuresis, including:
- Heredity. There is a strong possibility of a genetic component in the development of sleep enuresis. An individual is at greater risk if one or both parents experienced bedwetting as children.
- Imbalance in the production of antidiuretic hormone (ADH). This hormone, released by the pituitary gland, decreases the amount of urine produced in the kidneys. Usually, there is an increase in ADH production at night to maintain continence. If there is a decrease in the amount of ADH produced or the kidneys do not respond appropriately to the hormone, there is an increased production of urine that can result in sleep enuresis.
- Small bladder capacity. Individuals with decreased bladder capacity (which can be caused by bladder obstruction, pressure on the bladder caused by an enlarged prostate gland in males, and inflammation) are at greater risk for sleep enuresis. This is not due to a decrease in the actual size of the bladder but to a decrease in the functional capacity of the bladder.
- Overactive detrusor muscle. Studies have found that overactive detrusor muscle occurs in 70% to 80% of people with sleep enuresis (NAFC, 2022a).
- Urinary tract infection. UTI can increase the risk of bedwetting in some individuals.
- Medications. The side effects from certain medications can increase the risk of sleep enuresis. These medications include sleep medications, hypnotics, and medications used to treat psychiatric conditions, such as thioridazine and clozapine.
- Underlying health conditions. Examples include pelvic organ prolapse in females, prostate enlargement in males due to either benign or malignant causes, bladder cancer, diabetes, and sleep apnea.
Treatment for adult bedwetting focuses on determining the underlying cause and requires a thorough assessment of the patient by the clinician. Behavioral interventions can include decreasing fluid intake in the evenings, using bedwetting alarms, and using absorbent products (NAFC, 2022a).
ASSESSMENT OF THE PATIENT WITH URINARY INCONTINENCE
Problems with urinary incontinence can be acutely embarrassing for individuals. Therefore, the clinician must adopt a holistic approach to the assessment of a patient with urinary incontinence and be cognizant of its impact on all aspects of the patient’s life.
Initial Assessment
During the initial assessment, patients are asked about:
- Onset and duration of symptoms (to differentiate between acute incontinence and longstanding problems with urination)
- Precipitating factors
- Approximate number of incontinent episodes in a 24-hour period
- Amount of urine leakage
- Fluid intake, including types of fluids and time of day when most fluids are consumed
- Any self-imposed fluid restrictions due to incontinence
- Episodes of bowel incontinence, including onset and duration, precipitating factors, and frequency
Obtaining a complete medication profile is vital, not only for prescription medications, but also for over-the-counter medications, including herbal and vitamin supplements.
The clinician obtains a full and detailed health history, beginning with existing conditions that may lead to incontinence.
One of the goals of the initial patient assessment is to determine whether urinary incontinence may be related to an underlying condition that requires further evaluation and treatment. In such instances, the patient is referred to specialty practitioners. Symptoms that indicate the need for further evaluation include:
- History of frequent or persistent urinary tract infections
- Gross or microscopic hematuria
- Uterine prolapse
- Signs of neurological conditions
- Presence of a mass in the bladder or urethral or pelvic areas
(WOCN, 2021)
Major Systems Assessment
RESPIRATORY ASSESSMENT
Acute or chronic coughing causes an increase in intra-abdominal pressure that may result in stress urinary incontinence or exacerbate the symptoms in those who already have some degree of incontinence. The clinician asks about cigarette smoking, which is a factor in persistent coughing. Nicotine has also been shown to cause bladder irritation in some individuals, which adds to the risk of urinary frequency and urgency (WOCN, 2021).
CARDIOVASCULAR ASSESSMENT
Certain cardiac conditions, such as heart failure and cardiac arrhythmias, can place patients at greater risk for nocturia, difficulty getting to the toilet in time before urine leakage, and falls. Clinicians must consider that diuretics used in the treatment of heart failure may contribute to urinary incontinence (WOCN, 2021).
ENDOCRINE ASSESSMENT
Diabetes is a risk factor for urinary incontinence. Peripheral autonomic neuropathy can cause problems with bladder storage, and poorly controlled diabetes can lead to polyuria (the production of abnormally large amounts of urine), which can increase the risk for urge urinary incontinence. Polyuria can also potentially increase the risk for functional incontinence and make existing functional incontinence worse (WOCN, 2021).
Neurologic Assessment
A neurologic assessment is critical for a patient with urinary incontinence. Urination is regulated by spinal cord reflex centers, the micturition center in the pons, and cortical and subcortical areas in the brain. The sacral spinal cord segments 2–4 (S2–4) play a pivotal role in the voiding process, providing for the relaxation of the internal and external sphincters and facilitating the flow of urine.
Several neurologic conditions can affect voiding. Stroke and Parkinson’s disease are associated with urinary incontinence, in particular urge urinary incontinence. Multiple sclerosis and spinal cord injury are associated with neurogenic bladder and impaired bladder contraction (Gill, 2022).
Genitourinary Assessment
VOIDING SYMPTOMS
Voiding symptoms associated with urinary incontinence in all genders include:
- Hesitancy: a delay in starting urination
- Slow urine stream: the person’s observation of diminished urine flow compared to their longstanding pattern
- Intermittent stream: the flow of urine during voiding that stops and starts and reoccurs frequently
- Straining to void: increase in muscle contraction required to begin micturition
- Spraying of urine: described by the individual as urine spraying out rather than streaming
- Dribbling: a prolonged trickle of urine at the end stage of voiding
- Sensation of incomplete bladder emptying: the sensation of the bladder not being empty after completion of voiding
- Need to instantly urinate again: needing to void a second time immediately after voiding the first time
- Postvoiding leakage: uncontrolled leakage of more urine as soon as urination is complete
- Dysuria: discomfort or pain with urination
(WOCN, 2021)
MALE ANATOMY
Since urinary incontinence is less common among those with male anatomy, it is an area that may be overlooked by clinicians during the assessment of such patients. Physical assessment includes abdominal palpation for a distended bladder as well as examination of the external genitalia. The location of the urethral meatus is determined, along with the ease of retraction of the foreskin and any indication of congenital deformity (WOCN, 2021).
INCONTINENCE AND PROSTATE CANCER
Early detection of prostate cancer has led to increased treatment and better outcomes. However, approximately 1 in 5 men who undergo radical prostatectomy surgery use pads in the long term due to urinary incontinence. Older men are more at risk for postsurgery incontinence, and it is more likely that it will remain a lifetime problem. Around 30% to 50% of men who had no previous problems with urination are found to have some increase in urinary symptoms such as urgency after prostate surgery. There is a decrease in these symptoms for those who undergo a nerve-sparing surgical technique (Johns Hopkins, 2023).
Permanent urinary incontinence is more frequent in men who have had radiation treatment as well as surgery. Radiation results in changes in the bladder neck and urethral tissue, which leads to the development of incontinence. Nocturia and urine hesitancy are reported as being the most troublesome problems for men. Postvoid dribbling can be a sign of benign prostate enlargement or urethral stricture and is a symptom the clinician must inquire about. Stress incontinence is highly prognostic of urinary sphincter dysfunction in men following prostatectomy surgery (University of Utah Health, 2023).
FEMALE ANATOMY
The medical history and physical assessment of patients with female anatomy address a number of genitourinary issues:
- Pregnancy and the type and circumstances of delivery can significantly increase a woman’s risk for incontinence. During pregnancy, the increased pressure of the enlarging uterus on the bladder can lead to episodes of transient incontinence.
- Pelvic surgeries and pelvic pain can be related to problems with pelvic muscle support.
- Vaginitis can lead to the development of urge incontinence, so the clinician must inquire about symptoms such as pruritis, vaginal discharge, and malodor.
- Endometriosis (the growth of uterine lining tissue outside of the uterus) can result in urge urinary incontinence.
- Pelvic organ prolapse, which the patient may experience as a sensation of a vaginal “bulge,” increases the risk for urinary incontinence.
(WOCN, 2021)
During the physical examination, the clinician pays close attention to the abdominal region. The presence of scars may indicate past surgeries. Abdominal palpation can help to detect bladder fullness or retention. Any vaginal pain is recorded, as well as any atrophic changes to the vulva. In postmenopausal patients, findings related to incontinence may include vaginal dryness, pain, itching, irritation, and vaginal atrophy related to estrogen depletion (WOCN, 2021).
INCONTINENCE AND PREGNANCY
Most women who give birth do not develop problems with urinary incontinence. In the majority of cases, damage caused by childbirth self-repairs over time as the tissues progress through the normal stages of healing. The rate and severity of incontinence is higher in women who have had multiple pregnancies and in those who have had vaginal deliveries compared to those with cesarean section deliveries. The rate and severity of incontinence are also found to be higher in women with multiple pregnancies who had an instrument-assisted delivery vs. a vaginal birth in which instrument use was not required (Rosenman, 2023).
Pelvic Floor Muscle Strength Assessment
An examination may be indicated to determine pelvic floor muscle strength. A vaginal examination of the female anatomy (or a rectal examination in those who cannot endure a vaginal examination) or a rectal examination of the male anatomy is a critical part of a continence assessment to determine pelvic floor muscle strength. A rectal exam also allows the clinician to assess for rectal impaction. Rectal examination for male patients is a means for assessing the prostate gland; an enlarged prostate gland can be palpated through the rectum wall (WOCN, 2021).
These exams are carried out by professionals, including RNs, APRNs, OTs, and PTs, who have the appropriate training and qualifications. The clinician begins by explaining to the patient the reason for the examination and how it will be performed, including obtaining verbal and/or written consent per facility policy. It is vital that the clinician preserve the patient’s dignity and comfort at all times while performing these procedures.
The pelvic floor muscle strength evaluation is graded using the Modified Oxford Scale (see table below).
| Patient Capacity | Grade | Description |
|---|---|---|
| (Core Pelvic Floor Therapy, 2023) | ||
| Absent | 0 | No palpable muscle contraction noted |
| Slight trace | 1/5 | A slight, quick contraction with insubstantial compression of the clinician’s finger |
| Feeble | 2/5 | Feeble contraction with faint pressure felt on the clinician’s finger; may or may not result in lifting of clinician’s finger; sustained >1 second but <3 seconds |
| Moderate | 3/5 | Moderate contraction and compression noted on the clinician’s finger; may or may not result in lifting of the clinician’s finger; sustained for a minimum of 4–6 seconds and can be replicated 3 times |
| Steady | 4/5 | A solid contraction with effective compression of the clinician’s finger and lifting of the clinician’s finger near the pelvic bone; sustained for a minimum of 7–9 seconds and can be replicated 4–5 times |
| Robust | 5/5 | Distinct strong contraction and compression of the clinician’s finger along with posterior lifting of the clinician’s finger; sustained for a minimum of 10 seconds and can be replicated 4–5 times |
Skin Assessment
Maintaining skin integrity can be challenging for patients with urinary incontinence (and for their caretakers, among patients who need assistance). Incontinence-associated dermatitis (IAD), also called perineal dermatitis, can be caused by urine and stool coming in sustained contact with the skin surface. It is found on the perineal area, buttocks, and upper thighs.
Both urine and stool are caustic to the skin and lead to maceration and breakdown of the acid mantle that protects the skin integrity. The most common presentation of IAD is reddened skin. In people with darker skin, IAD may present as areas of hypo- or hyperpigmentation. When left untreated, it can progress to a partial-thickness skin injury. A serious concern for patients with IAD is their greater risk for developing pressure injury.
Another important concern for patients with incontinence is malodor of their skin and clothing. This often leads them to isolate themselves and to decrease their participation in activities (Baranoski & Ayello, 2020).
Functional Assessment
Patients with limitations in functional ability, such as difficulties with ambulation and sitting balance, are at high risk for functional incontinence. A functional assessment of the patient includes a comprehensive review of the patient’s ability to maintain independence in activities of daily living (ADLs) and instrumental activities of daily living (IADLs).
A functional assessment can be performed by a physical therapist or occupational therapist. The clinician first assesses for balance. Is the patient able to maintain a safe sitting position without losing their balance? Are they safe when standing independently and ambulating? If assistance is needed for any of these activities, how much assistance is required? Range of motion, transfer ability, ambulation, coordination, and proprioception are also evaluated.
The Berg Balance Scale is a standardized test commonly used to determine functional balance. This test examines both dynamic and static balance. Although it was initially used mostly with stroke patients, this scale has been found to have high validity and dependability in varying patient scenarios, including patients with neurological conditions including Parkinsons’ disease and multiple sclerosis (Cantellops & Tiu, 2023; Quinn, 2021).
Several musculoskeletal conditions can impede a patient’s ability to maintain continence, including osteo- and rheumatoid arthritis and back problems, to name two. These conditions affect ambulation and the person’s ability to reach a bathroom as well as dexterity and the ability to manipulate clothing to successfully achieve toileting. Chronic pain and fatigue can also impair motivation to attain continence. Other mobility impediments include braces, splints, and immobilizers (Edemekong et al., 2023).
A home evaluation is also particularly valuable because it provides insight into environmental issues that can lead to or increase the risk for incontinence, e.g., poor lighting, inadequate toileting facilities, and placement of furniture or rugs that hinders quick access to bathrooms. The clinician also inquires about the patient’s living situation and occupations, such as:
- Do they live in the community or a care facility?
- If in the community, with family or others?
- Are they still in the workforce?
- What are their activities and hobbies?
- Do they require assistance from others to perform activities of daily living, such as toileting?
- Is their bathroom easily accessible?
- Does the patient use a bedside commode or urinal at night?
(WOCN, 2021)
Cognitive/Mental Status Assessment
Cognitive conditions can impact an individual’s ability to maintain continence. For instance, depression and dementia may lessen the motivation for toileting. Persons with cognitive decline may not recognize the need for toileting or they may not remember the location of the toilet or how to prepare for toileting. The Mini-Mental State Exam (MMSE) is a short, structured test that can be used as an initial assessment of a patient’s cognitive status (WOCN, 2021; Rosenzweig, 2023).
- Delirium (an abrupt change in mental function resulting in confusion and decreased awareness of the environment) is associated with an acute onset of urinary incontinence. Delirium is reversible and can be caused by dehydration and/or a urinary tract infection, especially in those over 65 years.
- Dementia is a progressive condition and results in worsening episodes of incontinence. Those with advanced dementia may not be able to make known their need for toileting, may respond to toileting help with distress, and may be unable to respond to toileting cues from caretakers.
- Depression is a frequently occurring and underdiagnosed condition in older patients and in those with cognitive loss. It may lessen the motivation for toileting and heighten the risk of urinary incontinence. Conversely, many persons with urinary incontinence are too embarrassed to seek professional help and may instead withdraw from society as a means of dealing with their condition, which may increase their risk for depression.
(WOCN, 2021)
Laboratory and Diagnostic Studies
Laboratory and diagnostic studies play a critical role in diagnosing urinary incontinence. Some of the more common tests performed are discussed below.
URINALYSIS
For all patients with urinary incontinence, a urinalysis is ordered to assess for the presence of urinary tract infection and hematuria. Results from a urinalysis may require a follow-up urine culture and sensitivity testing.
POSTVOIDING RESIDUAL
Measurement of postvoiding residual (PVR) determines the amount of urine in the bladder after the patient voids. There are two methods of measuring postvoiding residual:
- A catheter is inserted into the bladder (using sterile technique) immediately after the patient has voided to drain and measure the amount of any residual urine left in the bladder.
- A noninvasive ultrasonic examination of the patient’s abdomen measures the three-dimensional amount of urine remaining in the bladder. Ultrasound has proven to be as accurate as catheterization at measuring postvoiding residual and is the preferred method (Ballstaedt & Woodbury, 2023).
There is a considerable lack of agreement and conflicting data on what constitutes a significantly elevated postvoiding residual for both men and women. Generally agreed-upon normal PVR volumes are described in the table below.
| Amount | Finding |
|---|---|
| (Ballstaedt & Woodbury, 2023) | |
| <100 ml | Normal |
| ≤200ml | Satisfactory |
| >200 ml | Deficient emptying |
| >300 ml | Indicative of urinary retention |
| >400 ml | Urinary retention |
| >20 ml in children | Abnormal (but varies with age) |
BLOOD TESTS
Blood tests include a prostate-specific antigen test (PSA) for men. This test checks the amount of PSA present in the blood, with a result of ≥4 nanograms/ml considered abnormal and requiring further investigation. Elevated levels can indicate an enlarged prostate, prostatitis, or prostate cancer.
Other blood tests to assess the status of renal and endocrine functioning include:
- Blood urea nitrogen (BUN)
- Serum creatinine
- Complete blood count (CBC)
- Estimated glomerular filtration rate (which may be done as part of a blood chemistry panel)
- Fasting blood sugar
- Hemoglobin A1C
(WOCN, 2021)
PAD TEST
A pad test is a noninvasive method used to measure the amount of urine lost in each incontinent episode and to determine the severity of urine incontinence. Pad tests can be done at home by having the patient wear pads continuously for 24–48 hours. The pad is weighed before and after an episode of incontinence. A one-hour pad test can be done in the clinical setting by inserting a predetermined amount of saline into the patient’s bladder before they are asked to perform a series of exercises. A pad test, however, will not distinguish between the different types of incontinence (Shenot, 2023).
BLADDER DIARY
The patient (or their caretaker) may be requested to keep a 24-hour record of:
- Fluid intake
- Frequency and amount of voiding
- Number of incontinent episodes
- Activities the patient was engaged in when an episode of incontinence occurred
- Any patient-reported sensation of urgency, discomfort, or pain
URODYNAMIC TESTING
Urodynamic testing is used to gain a clear picture of how well the lower urinary tract is functioning, the bladder’s urine storage capabilities, and how well the bladder can empty. Types of urodynamic testing include:
- Uroflowmetry. This is a noninvasive test that can be used for male and female patients. It measures the flow rate of urine and the patient’s ability to empty the bladder. The patient is asked to arrive for the test with a full bladder. The patient is provided with privacy and asked to void into a commode fitted with a flow meter funnel. The flow of urine is continuously measured, and the findings are displayed on a graph. A normal uroflowmetry test produces a bell-shaped curve.
- Filling cystometry. This test measures the pressure within the bladder to determine its storage capacity and intra-activity abdominal pressures. It is an invasive test and requires the placement of two pressure-sensitive catheters, one in the patient’s bladder and the other in the rectum, to gauge the abdominal pressure range. The bladder is then filled with normal saline via the catheter placed in the bladder. Pressure is monitored while the bladder is being filled and before the patient is allowed to void. The abdominal pressure readings are subtracted from the bladder pressure readings, and the resulting value indicates the pressure wielded by the bladder.
- Electromyography (EMG). Electrode patches are placed in the groin area to monitor the functioning of the pelvic muscles during the different stages of voiding, with the electrical output from the pelvic floor muscles displayed graphically. During the bladder-filling phase, a slight increase in electrical activity should be noted, which is referred to as the guarding reflex. During voiding, the pelvic floor muscles will normally relax, indicated by minimal or no EMG activity, while abnormal pelvic floor functioning is characterized by an increase in EMG activity during voiding.
(WOCN, 2021)
Assessing Incontinence in Children
The initial assessment of a child with urinary incontinence centers on voiding and defecation patterns. Ruling out constipation is important.
Prior to the appointment with the healthcare provider, the family and child are requested to complete a fluid intake/voiding and stooling frequency diary. Factors to be included in the diary include frequency of urination, number of episodes of incontinence, the presence of urgency, and how long each voiding lasted. This can provide valuable information on the child’s condition.
Attention is given to fluid intake, both the type and number of fluids that the child drinks. It is not uncommon to find that what most children drink on a daily basis consists mainly of caffeinated beverages and juices, with limited water intake. Educating children and families about the importance of swapping out some snack drinks for water is something the clinician should keep in mind (WOCN, 2021).
Access to toileting facilities at school should also addressed. If the provider determines that the child needs more frequent toilet breaks during the school day, this may be discussed with the school nurse and accommodations made to provide the child with more frequent toilet breaks.
The abdomen should be palpated to detect retained stool and/or distended bladder. If the equipment is available, performing a bladder scan to determine pre- and postvoiding volumes can provide valuable information on urine retention. Genital findings of concern include vaginal redness, labial adhesions, and continuous urine leakage in girls, and meatal and foreskin abnormalities in boys.
The clinician also inspects the child’s back to rule out the presence of sacral dimples or hairy patches, which could indicate a spinal cord pathology, such as spina bifida or tethered spinal cord syndrome. A urinalysis is conducted to rule out the possibility of infection or the likelihood of renal disorder or metabolic abnormalities that would lead to incontinence (WOCN, 2021).
TREATING INCONTINENCE
A multidisciplinary team of healthcare professionals is involved in the diagnosis and treatment of incontinence. They include:
- Urologists
- Urogynecologists, who are specially trained in the care of women with pelvic floor disorders
- Primary care providers such as physicians and nurse practitioners
- Nurses, including those with specialized training and certification in incontinence care, who are involved in patient assessment, addressing behavioral and lifestyle changes, and interventions such as bladder training
- Physical therapists, who are proficient in the evaluation and treatment of urinary and fecal incontinence and who may specialize in interventions for pelvic floor disorders, including instruction in pelvic floor exercises, manual manipulation, and other treatment modalities (such as electrostimulation, biofeedback, and/or vaginal dilators or weighted vaginal cones)
- Occupational therapists, who are involved in all areas of incontinence care, including patient assessment and identification of the type of urinary incontinence, training patients in increased awareness of pelvic floor muscle activity, and developing patient lifestyle interventions (i.e., ADL, IADL, home assessment) to cope with urinary incontinence
During the assessment process and before interventions are put in place, it is important for each clinician to establish the patient’s perception of the severity of the problem and its impact on their life. Treatment should be guided by the limitations incontinence places on the patient and the degree of intervention preferable to them (WOCN, 2021).
Treatment generally begins with noninvasive interventions that reduce incontinence and enhance coping skills.
Lifestyle Interventions
Lifestyle and behavioral interventions are the first line of treatment for urinary incontinence and may include smoking cessation and weight loss. Smoking has been shown to have a negative impact on continence. Smokers, particularly those who have a long-term history of tobacco use, are at risk of developing a chronic cough that puts significant pressure on the pelvic floor muscles. Nicotine is a bladder irritant and results in frequent urges to void. Nicotine is also a primary cause of bladder cancer (SFC, 2023c).
Obesity increases pressure on the bladder and pelvic floor muscles and increases the risk of developing stress urinary incontinence. It has been shown that for every five-unit increase in body mass index (BMI), females increase their likelihood of developing urinary incontinence by as much as 70% (WOCN, 2021).
Patients are also instructed to avoid dehydration. Decreased fluid intake may lead to concentrated urine, which can irritate the bladder. It can also lead to the formation of kidney stones and increase the risk of urinary tract infections and constipation. Adults ages 65 and over are particularly susceptible to the effects of dehydration. Older patients are educated not to wait to feel thirsty before drinking fluids and that dark-colored urine can be a sign of dehydration.
The timing of fluid intake is discussed with the patient, with the recommendation to develop an individualized, day-to-day pattern of fluid intake. This may include limiting fluid intake in the later part of the day and avoiding caffeinated beverages, alcohol, and acidic foods, which are all bladder irritants (SFC, 2023a; Mayo Clinic, 2023b).
Behavioral Interventions
For urge and stress incontinence, a bladder-retraining program can be initiated during the daytime hours. This is a technique to delay urination once the person feels the urge to void. To begin, the patient is asked to maintain a voiding diary to establish their voiding pattern. Then, the patient is asked to void 15 minutes prior to their usual voiding time in order to avert the urge sensation to void. For example, if the voiding diary shows that the patient voids every 90–95 minutes, the retraining program will start with voiding every 60 minutes. If the urge to void arises before the 60-minute interval, the patient is encouraged to postpone voiding if possible until the scheduled time, or at a minimum to wait for 5 minutes beyond the initial urge to void. At intervals that are comfortable for the patient, perhaps weekly, a goal is set to extend the voiding time by another 15–30 minutes until a 3- to 4-hour time period is achieved between each void (WOCN, 2021).
Double voiding is a mechanism that helps the patient to empty their bladder more completely with each voiding. The patient voids and remains on the toilet for a few minutes then tries to void again.
Scheduled toileting is a technique commonly used with cognitively impaired patients who cannot recognize or communicate their need to void. The patient is assisted to the restroom to void every 2 hours rather than waiting for the need to urinate. The goal is to prevent an incontinent episode by toileting on a regularly scheduled basis. To be successful, caregivers must be able to adhere to the schedule.
Prompted voiding is another behavioral intervention advanced by psychologists specifically for nursing home residents. The staff member asks the resident if they are wet or dry. Once the resident answers, the staff member checks the patient and informs them about the accuracy of their response. The staff member then helps the resident to the toilet, even if they already had an incontinent episode, and praises them when they void in the toilet. Once the resident is comfortably settled back into their environment, the staff member tells them when they will have another opportunity to use the restroom, ensuring that the resident can see a clock or a watch.
One of the goals of prompted voiding is to help patients become better aware of when they have an incontinence episode and when they are dry. Recognizing that they are dry but need to void is intended to remind the resident to ask for assistance to the restroom. The disadvantage of this intervention is that it can be time-consuming. Studies have shown positive results when it is consistently applied (Quinn, 2021).
Urinary Incontinence Products
Some patients may need to or choose to use incontinence products, including:
- Patients for whom incontinence can be completely reversed
- Patients who have to cope with incontinence for a period of time, e.g., those waiting to achieve the benefits of pelvic floor muscle training
- Patients who choose incontinence management over other interventions
For all of these people, incontinence products are an essential intervention in maintaining their personal and social activities.
Absorbent products can include panty liners, pads, and specially designed underwear. Patients with female anatomy are advised to use incontinence pads rather than feminine hygiene pads for moderate to heavy leakage. Incontinence products are created with the surface area nearest to the urethral orifice, which is superior to the vagina. These products are highly absorbent, with a decrease in skin irritation when compared to less-absorbent products (WOCN, 2021).
For patients with male anatomy, a drip shield can be used for mild episodes of incontinence, while a drip guard is useful for more excessive leakage. The shields have a waterproof backing. They are placed over the head of the penis and can be secured in place by wearing relatively snug-fitting underwear (NAFC, 2022b).
When deciding on the optimal product(s) to use, the clinician, patient, and caregiver take into consideration the following factors:
- Severity of the incontinence problem
- Anatomy of the patient
- Physical build, height, and weight of the patient
- Mental capacity
- Mobility level
- Problems with dexterity
- Eyesight
- Lifestyle, including home and work environments
- Level of independence or assistance needed
- Available storage
- Personal preferences and priorities, such as need for discreetness
(WOCN, 2021)
Treating Incontinence-Associated Dermatitis
The primary approach to the treatment of IAD includes:
- Reversing the cause(s) of incontinence or reducing the incidence of incontinence
- Avoiding cleansing the perineal area with soap, substituting cleansing products that prevent overdrying or irritation of the skin
- When bathing, using warm (not hot) water and refraining from vigorous rubbing or scrubbing of the skin
- After cleansing and drying, applying a barrier cream such as zinc oxide or dimethicone
If an absorptive product is used for incontinence containment, it should wick urine (and stool, if applicable) away from the skin (WOCN, 2021).
Psychological and Emotional Interventions
Psychological and emotional interventions aim to enhance the patient’s ability to cope with urinary symptoms. Many people with urinary incontinence feel alone and are unable to talk to family or friends about their problem. Being able to talk to a clinician about constant fear of uncontrolled urinary leakage and the feelings of embarrassment and depression is an important step in developing coping mechanisms (WOCN, 2021).
Incontinence Devices
Pessaries provide a low-risk treatment choice for many women and are used frequently. These devices are fitted into the vagina and provide support to pelvic organs that have moved downward. They also supply compression to the urethra to decrease the risk of urinary incontinence. Whether the patient is sexually active will influence the type of pessary used. Most women find pessaries comfortable.
Pessaries are fitted by the clinician and usually require follow-up appointments every three to six months to ensure the patient is appropriately self-managing pessary use. During the follow-up visit, the clinician exams the vaginal vault for any signs of mechanical erosion or other lesions. The clinician also inspects the pessary for any signs of damage.
Pessaries are not suitable in all cases, such as for women who have scarring of the vagina, vaginal dryness, or a restricted or shortened vagina. Women with weakened pelvic muscles may have difficulty keeping a pessary in place, but strengthening of pelvic floor muscles may alleviate this problem.
Men with urinary incontinence can use clamps as an alternative to pads and collection devices. A clamp prevents incontinence by exerting pressure on the penis. It is placed around the base of the penis and secured just to the point where it will prevent urine leakage. Clamps are recommended for men who are diagnosed with stress incontinence only.
The use of clamps requires careful assessment by the clinician. The clinician must ensure that the patient has no cognitive deficits and that they have the manual dexterity to apply and remove the clamp safely. Patients are educated to use clamps with caution since they can impede blood flow, resulting in ischemic damage to the penis. Patients are also reminded to be alert for signs of skin damage to the penile surface caused by the clamp. Clamps have been found to be most successful in situations that require short-term usage, such as when a patient has to attend a meeting or is engaged in recreational activities (WOCN, 2021).
Pelvic Floor Rehabilitation
Pelvic floor rehabilitation includes an emphasis on weak or tight muscles, postural modifications, body mechanics, and lifestyle adjustments. Interventions include behavioral approaches, manual therapies, education, and functional retraining.
In 1950, Dr. Arnold Kegel developed pelvic floor exercises known as Kegel’s exercises. More generally referred to as pelvic floor muscle training (PFMT), this is the first-line treatment for women with urinary incontinence. It has been found that PFMT provides benefits regardless of the type of incontinence present. Although there is abundant evidence that PFMT is a safe and effective treatment, many candidates who could benefit from PFMT have only a scant understanding and insight into this treatment choice.
Positive results reported by women include decreased episodes of incontinence and an improved quality of life. Research has shown that strengthening the muscles of the pelvic floor can diminish the incidence of urinary incontinence by up to 90% (Mayo Clinic, 2022a; Huang & Chang, 2023).
PFMT has not been as well studied in men as it has been in women, but it is still considered a primary recommendation for men with urinary incontinence after radical prostatectomy. Continence may be regained sooner if PFMT instruction is introduced in the preoperative or immediate postoperative period to male patients undergoing radical prostatectomy surgery (WOCN, 2021; Sayner & Nahon, 2022).
Instruction in PFMT is provided by physical therapists and occupational therapists who have obtained specialized PFMT training. Important first steps include patient education about the utility of PFMT, exploring patients’ treatment expectations, and realistic goal setting. Patients are advised that PFMT requires a time commitment and that positive results may only be noticeable after several treatment sessions (Stratton, 2022).
How does PFMT work? During a strong contraction, the levator ani muscles are moved upward and forward, facilitating compression of the urethra and adding to urethral closing pressure. Strengthened pelvic floor muscles give support to the bladder neck and the proximal urethra. Maintaining the urethra in its normal position during activities that heighten intra-abdominal pressure decreases the likelihood of urine leakage.
In conjunction with the patient, the clinician creates an individualized program of exercises. A key factor to success is the patient’s level of motivation and their willingness to adhere to the exercise maintenance program (Stratton, 2022).
The clinician first teaches the patient how to identify the pelvic floor muscles by instructing them to “draw in” or contract the muscles around the vagina and/or anal sphincter, as if they are trying to stop urination or defecation. The contraction of these muscles is maintained for about 10 seconds, followed by a period of relaxation for a minimum of 10 seconds. A typical training schedule is to perform three to four rounds of pelvic muscle exercises each day and to include 10 to 15 repetitions in each round. The clinician teaches the patient to perform the exercises while sitting, standing, and lying supine. The patient is counseled not to use the abdominal or buttock muscles while doing pelvic floor muscle exercises. For some patients, this takes time and conscious effort to master (WOCN, 2021).
Evaluating the patient’s body stance and breath-holding patterns with purposeful activities can also be valuable in treating urinary incontinence. A patient’s posture when sitting on the commode can increase the pressure on the bladder and constrict pelvic floor muscles, making it difficult for the patient to empty their bladder. Patients who have developed the habit of holding their breath (which can be a response to tension and stressful life events) can also experience increased tension on pelvic floor muscles, which in the long term can result in pelvic floor muscles weakening and increasing episodes of incontinence. A good intervention is to teach patients pursed-lip breathing and to encourage them to use this breathing technique, especially when voiding or having a bowel movement.
Another useful intervention is to have the patient do forward trunk flexion followed by trunk extension while sitting on the toilet after voiding to ensure complete bladder emptying (Quinn, 2021).
OTHER PELVIC FLOOR REHABILITATION MODALITIES
Other interventions that can be used to assist with isolating the pelvic floor muscles include:
- Electrostimulation: A small electrical current is used to assist the patient in identifying the pelvic floor muscles.
- Biofeedback: A vaginal or rectal pressure sensor provides audible or visual feedback of the strength of the pelvic floor muscle contraction.
- Vaginal dilators or vaginal cones: These devices are placed in the vagina, and the patient is taught to retain them in position by pelvic muscle contractions during regular daily activities.
(WOCN, 2021)
Pharmacology
Several different classes of medications are used to treat urinary incontinence. These include:
- Anticholinergics (also known as antimuscarinics) reduce bladder contractions, increase bladder capacity, and decrease the urgency to void. Medications in this category include fesoterodine (Toviaz) and solifenacin (VESIcare).
- Beta-3 agonists, such as mirabegron (Myrbetriq), have been shown to reduce the number of incontinent episodes per day.
- Antidepressants. Imipramine (Tofranil) is a tricyclic antidepressant sometimes used to treat bedwetting in children 6 years of age and up. Duloxetine (Cymbalta) is a serotonin/norepinephrine reuptake inhibitor approved in Europe for the treatment of stress urinary incontinence, but it is not approved by the U.S. Food and Drug Administration (FDA) for incontinence treatment in the United States.
- Topical estrogen. Estrogen receptors are found in the vagina and also in the tissues of the bladder and urethra. It is thought that estrogen deficiency contributes to the development of urinary incontinence.
(WOCN, 2021; Ellsworth & Kim, 2022)
Surgical Interventions
The most commonly used surgical interventions are described below:
- Sling procedures are used for urethral support and to exert external urethral compression. The most frequently performed sling procedure involves the placement of a synthetic mesh to form a suburethral sling. The midurethral sling procedure is currently regarded as the “gold standard” for the treatment of stress urinary incontinence in women. Sling procedures are also regarded as an effective choice for male patients coping with incontinence after prostatectomy surgery, in particular those with slight to moderate leakage.
- Artificial urinary sphincter. For male patients this procedure has been found to give the best long-term success in dealing with urinary incontinence after radical prostatectomy surgery. It is regarded as the primary surgical intervention for these patients.
- Urethral bulking agents. The injection of bulking agents is used to cushion the urethral mucosa, thereby increasing urethral coaptation (closing) and reestablishing continence. Collagen and synthetic agents are used as bulking materials. The body will eventually absorb collagen, and so collagen bulking agents usually require repeat injections every 6 to 18 months. Synthetic materials require less-frequent repeat treatments.
(WOCN, 2021)
INTRAVAGINAL LASER TREATMENT
Intravaginal laser treatments are used for the treatment of mild and moderate stress urinary incontinence. Clinical studies into the effectiveness of this treatment are ongoing. A study conducted in Europe in 2019 indicated that intravaginal laser treatment resulted in improvement for patients with mild and moderate stress urinary incontinence (Ranjbar et al., 2022).
CASE
Jennifer is in her late 40s, is married with three children, and works in a management position with a local company. During a visit with her healthcare provider, she confides to the nurse that since the birth of her youngest child 15 years ago, she has had problems with urinary incontinence, stating, “I can’t walk across a room without leaking.” The nurse asks her to keep a detailed voiding diary for a week, including fluid intake.
At the next appointment Jennifer and the nurse review the voiding diary, and Jennifer is referred to a specialized continence clinic. At the continence clinic, Jennifer is evaluated by the different professionals who make up the continence team. Jennifer tells the urologist that she does not want to undergo any surgical procedures. While the continence nurse works with Jennifer on interventions to deal with the immediate problems of incontinence, including skin care and odor control, the occupational therapist provides instruction on mind-body relaxation, coping skills to deal with the constant worry about incontinence, and biofeedback to help identify pelvic floor muscles. The physical therapist educates Jennifer about pelvic floor physical therapy, and together they devise an individualized program of rehabilitation, which includes pelvic floor muscle training, manual manipulation, biofeedback, electrostimulation, and weighted vaginal cones.
Jennifer is highly motivated and carefully follows the instructions from all the team members. After three months, Jennifer’s problem with incontinence is greatly reduced.
Treating Urinary Incontinence in Children
Treatment options include:
- Bedwetting alarm
- Nighttime waking and toileting by parents
- Bladder therapy
- Psychotherapy
- Medications such as desmopressin (DDAVP, Nocdurna)
(WOCN, 2021)
Alarm systems to treat nighttime enuresis in children have a success rate of around 66%. Parent involvement is critical to the success of this intervention, since they must be available to wake up the child when the alarm sounds if the child does not wake up on their own. After waking up, the child is taken to the restroom to void even if the child has voided in bed. The aim of the intervention is to teach the child to wake up to the feeling of a full bladder.
There are challenges to this treatment. During the school term, the disturbance to the child’s sleep pattern may cause the child to become overtired and cause a negative impact on their performance in school. The child may be sharing a room with siblings, and parents may be hesitant about causing possible disruptions to their sleep. However, studies indicate that when this intervention is used consistently, it results in the majority of children achieving nighttime dryness. Parents should be told that using an alarm system can take up to two to three months of continuous use before there are positive results (WOCN, 2021).
For children who have unintegrated spinal Galant reflex, occupational therapists may have special training in primitive reflex integration techniques. These techniques include balance games and core strengthening training exercises (Brain Balance, 2023; Hill, 2021).
To be effective, management of children with voiding problems must also include consideration of psychological or cognitive issues. Assessing the impact that urinary dysfunction has on the child’s life is key, and questionnaires have been developed to address this, including the Pediatric Urinary Incontinence Quality of Life Score (WOCN, 2021).
BOWEL INCONTINENCE
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK, 2017) defines bowel incontinence as “the inability to hold a bowel movement until reaching the bathroom.” Fecal incontinence can occur at any age, but it is more common in older adults. It is estimated that bowel incontinence affects 1 in 5 adults aged 65 years and older who live in the community and residential care settings and affects half of those living in long-term care facilities (WOCN, 2021).
Types of Fecal Incontinence
Fecal incontinence can be divided into several different types.
URGE FECAL INCONTINENCE
Urge fecal incontinence occurs when the individual experiences an immediate urge to defecate and is unable to reach the restroom in time. Causes of urge fecal incontinence include colorectal motility disorders, reduced rectal capacity, and malfunctioning of the external anal sphincter (WOCN, 2021).
PASSIVE FECAL INCONTINENCE
Passive fecal incontinence refers to stool or gas that is passed when the individual is not aware that it has happened. This occurs when anal closure is not intact and there is a lack of sensation. It can be caused by rectal prolapse, injury, or trauma, sometimes sustained during childbirth. Passive incontinence ranges from slight soiling of undergarments to complete evacuation of bowel contents. It is frequently found in persons with cognitive impairments such as dementia (WOCN, 2021).
PARTIAL FECAL INCONTINENCE
Partial fecal incontinence occurs when there is a small amount of fecal leakage resulting in soiling of underwear. This can be a continuous problem, or it can occur from time to time in persons who are normally continent. It can be caused by malfunctioning of the internal anal sphincter, which is responsible for preventing leakage of small amounts of stool and gas, or it can be caused by diminished sensory ability that impedes detection of stool in the rectal vault (WOCN, 2021).
FUNCTIONAL BOWEL INCONTINENCE
Functional incontinence is associated with physical limitations, mobility issues, and structural impediments such as inaccessibility of toileting facilities (WOCN, 2021).
OVERFLOW INCONTINENCE
Overflow incontinence occurs as a result of stool impaction, where there is leaking of soft feces from around hard, impacted stool. This is not always easy to diagnose, and it is a frequent problem among frail elderly residents in long-term care facilities (WOCN, 2021).
Patient Assessment
INTERVIEW
During the interview with the patient, the clinician develops an inclusive assessment of the problem with bowel incontinence. This includes such factors as:
- Onset of the problem and its severity
- Whether the patient still has some controlled bowel movements
- Stool consistency during both continent and incontinent episodes of bowel evacuation
- Whether the patient experiences episodes of constipation or diarrhea
- Whether the patient is aware of when there is gas or stool in the rectal vault
- Whether the patient can distinguish between gas and stool
- How long the patient can maintain continence when they have the urge to defecate
The interview also includes detailed questions about the patient’s food and fluid intake as well as a complete review of their medication profile. The clinician pays specific attention to the patient’s use or misuse of laxatives and any large intake of caffeine products, alcohol, and food items that contain sorbitol (an artificial sweetener), which can result in loose stools that are more difficult to contain. Alarm signals, which include worsening bowel symptoms, weight loss, and blood loss, require immediate further assessment (WOCN, 2021).
The above problem-focused history helps the clinician to determine the type of bowel incontinence the patient is experiencing: urge fecal incontinence, passive fecal incontinence, or minor leakage of bowel contents.
Beyond this, the holistic assessment determines preexisting conditions that could result in bowel incontinence. Some of the major conditions that may give rise to bowel incontinence include:
- Diabetes. Diabetes has been found to be a risk factor for bowel incontinence.
- Obesity. Obesity is a significant risk factor for bowel incontinence, with increase in BMI correlated to increased risk of bowel incontinence.
- Radiation treatment. There is a high incidence of bowel incontinence after the use of pelvic floor radiation for prostate cancer, gynecological cancers, and rectal and anal cancers.
- Irregular bowel elimination. Diarrhea and fecal impaction are leading causes of bowel incontinence, especially in older adults.
- Dementia. The incidence of bowel incontinence is higher in patients with dementia than those of similar age without this condition.
- Depression. Depression is a risk factor; this may be related to the side effects of antidepression medication.
- Irritable bowel syndrome. Irritable bowel syndrome is a risk factor for bowel incontinence.
- Spinal cord injury. Patients with spinal cord injury frequently have issues with bowel incontinence.
(Atnip, 2023; WOCN, 2021)
Bowel incontinence can have a detrimental effect on the individual’s quality of life and is an acutely embarrassing problem. Psychological findings associated with bowel incontinence include:
- Diminished self-esteem and confidence
- Unwillingness to discuss bowel incontinence with others, including clinicians
- Heightened risk for anxiety and depression
- Demoralization by negative feelings of embarrassment, fear, and shame
- Dependence on caretakers and loneliness
PHYSICAL EXAMINATION
The physical examination of the patient includes the following components:
- Digital rectal exam, which allows the clinician to assess rectal filling, resting anal tone, the patient’s ability to generate a voluntary contraction, and overall anal sensitivity
- Examination of perineal skin surfaces for signs of incontinence-induced skin damage such as redness, rash, and excoriation
- Assessment of the perineal area for signs of obstetrical injury in female patients or scars from previous surgery
- Abdominal palpitation to assess for pain, tenderness, and possible abdominal masses
DIAGNOSTIC TESTING
Diagnostic testing for bowel incontinence includes:
- Stool tests for ova and parasites and stool culture for various infectious organisms such as salmonella, E. coli, and C. difficile
- Anoscopy and proctoscopy to assess for hemorrhoids and anorectal masses
- Endo-anal ultrasound (EAUS) (regarded as the “gold standard”) to determine the presence of anal sphincter injury
- Anorectal manometry to evaluate pressures in the anal canal and distal rectum; primarily used to gauge the functionality of the internal and external anal sphincters
- Defecography to identify functional difficulties with rectal emptying, which can occur in the presence of rectal prolapse or posterior vaginal prolapse (rectocele)
(WOCN, 2021)
Management and Treatment Interventions
Managing bowel incontinence requires a holistic, multidisciplinary team approach, with interchanging and overlapping roles between nursing, physical therapy, and occupational therapy. The overall goal of management interventions is either the complete elimination of bowel incontinence or, where this is not achievable, a decrease in the frequency or severity of bowel incontinence.
The first step in deciding on a management program is a discussion between the patient, family, caregivers, and clinicians regarding the treatment options available and which will best fit the patient’s unique circumstances.
Conservative management of bowel incontinence is the primary intervention for patients without anal sphincter damage or defects. Patients who have sphincter defects are recommended to have a surgical evaluation (WOCN, 2021).
BOWEL RETRAINING
First-line interventions include establishing a regular bowel habit. The clinician educates the patient and family about peristaltic contractions of the colon, which are most active in the morning after wakening and after eating. These contractions aid with bowel evacuation and should not be ignored. The clinician emphasizes the importance of establishing a regular time for toileting and maintaining that routine, even if at first the patient does not feel a need for defecation. Following a consistent schedule will assist in training the bowel to empty. Scheduling toileting for the time after breakfast is optimal.
DIETARY CHANGES
Dietary adjustments are frequently necessary in reducing the rate of bowel incontinence. Successful dietary approaches include:
- Scheduling meals to meet individual needs for travel, work, and recreational activities
- Decreasing food intake and avoiding large meals
- Maintaining a food diary to identify foods that may worsen episodes of incontinence and then eliminating those foods from the diet
- Adding yogurt, high-fiber foods, and/or a fiber supplement to the diet
- Increasing water intake to 2 to 3 liters daily
PHARMOCOLOGIC TREATMENT
The medication loperamide (Imodium) is a first-line treatment used to treat bowel incontinence associated with loose stools. Patients taking loperamide are warned not to drink tonic water, which can interact with loperamide and result in serious heart problems (Drugs.com, 2023).
BOWEL THERAPY TREATMENTS
When the pressure of the stool in the rectum is more than the pressure in the pelvic floor, then the individual will achieve a bowel movement. Therefore, the pelvic floor must be able to contract so that the individual can maintain bowel continence, and the pelvic floor muscles must be able to relax to facilitate defecation. For individuals who are unable to relax the pelvic floor muscles, this leads to straining and incomplete emptying of stool (WOCN, 2021).
Therapeutic treatments that can be used for bowel incontinence include:
- Pelvic floor muscle training (PFMT). The procedure for teaching and performing PFMT exercises is basically the same as for patients with urinary incontinence (see “Pelvic Floor Rehabilitation” earlier in this course). The primary goal of physiotherapeutic muscle training in the treatment of bowel incontinence is to enhance the strength, tension, endurance, and coordination of the anal sphincter and the pelvic floor muscles. The clinician develops an individualized exercise pattern for each patient based on their baseline pelvic muscle strength and endurance.
- Biofeedback is regarded as the primary treatment for mild to moderate incontinence. Biofeedback enhances sensory awareness, increases pelvic muscle strength and ability, and augments coordination between abdominal and pelvic floor muscles. Since one of the main obstacles to pelvic floor strengthening is the inability of patients to correctly identify and isolate pelvic floor muscle contractions, biofeedback is used to assist the patient to identify the pelvic floor muscle and anal sphincter contractions without the concurrent contraction of other muscles.
Devices used to provide biofeedback include anorectal manometry and surface or endoanal EMG. The goal for using these devices is to provide the patient with knowledge about their muscle activity or a variation in the anal canal pressures. Biofeedback done in conjunction with PFMT has proven to be successful in the treatment of bowel incontinence not responsive to lifestyle changes. Biofeedback is helpful to more than 75% of those with pelvic floor dysfunction. - Perineal massage has been found to be therapeutic in the prevention of fecal incontinence when it is performed in late stages of pregnancy. Antenatal perineal massage results in relaxation, enhances the blood flow within the perineum, and allows the pelvic floor muscles to become more flexible. Research indicates that pelvic floor massage has no adverse side effects and is well tolerated by women. The recommended treatment is 10 minutes of massage each day beginning at the 34th week of pregnancy until delivery.
- Electrical stimulation of the anal mucosa and/or tibial nerve may be used to improve anal sphincter functionality.
(Cleveland Clinic, 2020; Mazur-Bialy et al., 2020; WOCN, 2021)
FECAL CONTAINMENT
Various products are used for fecal containment. These include pads and briefs. Other devices used are:
- Anal plug. This is a small, cup-shaped device that is placed in the rectum. An attached string is used to remove the device.
- Anal pouch. This is an external collection device with a wafer that sticks to the perianal skin. The pouch is equipped with a resealable port that allows it to be drained. Pouches can be difficult to apply and difficult to maintain adherence.
SKIN CARE
Bowel incontinence places the patient at risk for skin damage. Stool is more irritating to the skin than urine, and a combination of urine and fecal incontinence increases the risk for skin breakdown. A skincare protocol is individualized for each patient, depending on the severity and frequency of bowel incontinence. Moisture barrier products are used, especially when there is frequent and excessive bowel incontinence. Zinc oxide may be used (or a combination of zinc oxide and petrolatum, which allows for easier application and removal than zinc oxide on its own).
SURGICAL TREATMENTS
When bowel incontinence cannot be successfully managed using conservative treatments, a surgical evaluation is considered. Several different surgical interventions are used to treat bowel incontinence, including:
- Sphincteroplasty: a procedure to repair a damaged or weakened anal sphincter
- Sphincter replacement: a procedure to replace a damaged sphincter with an artificial sphincter, which is an inflatable cuff implanted around the anal canal
- Dynamic graciloplasty: relocating the gracilis or gluteus maximus muscles by wrapping them around the anal sphincter to restore muscle tone
- Sacral nerve stimulation: implanting electrodes to treat internal sphincter and external sphincter muscle damage
(Mayo Clinic, 2022b; WOCN, 2021)
CASE
Donald is a 76-year-old man with bowel incontinence. According to the patient, his greatest problem is that he has been unable to play golf due to fear of bowel accidents, which he describes as “sad and depressing.”
After obtaining a thorough history and performing a physical examination, the clinician determines that Donald is experiencing frequent episodes of moderate stool leakage. The clinician discusses dietary changes and a bowel retraining program with the patient. After determining that Donald is cognitively intact and has good manual dexterity, the clinician suggests the use of an anal plug and provides the patient with teaching and instructions on using the plug.
At a follow-up visit six weeks later, Donald describes the changes he has been making, including a diet higher in fiber and a regularly scheduled time for toileting after breakfast. The patient notes that he is having fewer episodes of incontinence. He uses the anal plug when he leaves home, which he is now doing more frequently, and he is playing golf three times a week. Donald describes his life as “much improved” and expresses his motivation to continue with the current interventions.
CONCLUSION
Bladder and bowel incontinence are frequently a hidden and unspoken problem. Due to shame and embarrassment, many people are hesitant to discuss these issues with healthcare providers. Incontinence results in both physical and emotional problems that diminish the quality of life for individuals in all age groups. Older adults often mistakenly consider incontinence to be a consequence of aging and one they must learn to live with. It is up to clinicians to be proactive in inquiring about problems with incontinence with sensitivity and not to assume that there is no problem if the patient does not bring it up on their own.
RESOURCES
Bladder control problems (NIDDK)
National Association for Continence
Simon Foundation for Continence
Urinary incontinence (ACOG)
Urinary incontinence (Urology Care Foundation)
Urinary incontinence in older adults (National Institute on Aging)
REFERENCES
NOTE: Complete URLs for references retrieved from online sources are provided in the PDF of this course.
Atnip S. (2023). Diabetes. Simon Foundation. https://simonfoundation.org
Ballstaedt L & Woodbury B. (2023). Bladder post void residual volume. StatPearls Publishing. https://www.ncbi.nlm.nih.gov
Baranoski S & Ayello EA. (2020). Wound care essentials, practice principals (4th ed.). Wolters Kluwer.
Brain Balance. (2023). Retained primitive reflexes as a sign of brain imbalance. https://www.brainbalancecenters.com
Cantellops NM & Tiu TM. (2023). Berg balance testing. StatPearls Publishing. https://www.ncbi.nlm.nih.gov
Cleveland Clinic. (2020). Pelvic floor dysfunction. https://my.clevelandclinic.org
Core Pelvic Floor Therapy. (2023). Understanding pelvic floor strength: A guide to the Modified Oxford Scale. https://corepelvicfloortherapy.com
Drugs.com. (2023). Loperamide. https://www.drugs.com
Edemekong PF, Bomgaars DL, Sukumaran S, & Schoo C. (2023). Activities of daily living. StatPearls Publishing. https://www.ncbi.nlm.nih.gov
Ellsworth P & Kim ED. (2022). Overactive bladder medication. Medscape. https://emedicine.medscape.com
Gill B. (2022). Neurogenic bladder. Medscape. https://emedicine.medscape.com
Harris S & Riggs J. (2023). Mixed urinary incontinence. StatPearls Publishing. https://www.ncbi.nlm.nih.gov
Hill J. (2021). What is the spinal Galant reflex? Harkla. https://harkla.co/blogs/special-needs/spinal-galant-reflex
Huang YC & Chang KV. (2023). Kegel exercises. StatPearls Publishing. https://www.ncbi.nlm.nih.gov
Johns Hopkins. (2023). Urinary dysfunction after prostate cancer treatment. https://www.hopkinsmedicine.org
Khatri M. (2022). Urge incontinence. WebMD. https://www.webmd.com
Mayo Clinic. (2023a). Treatment options for men with urinary leakage. https://www.mayoclinichealthsystem.org
Mayo Clinic. (2023b). Urinary incontinence. https://www.mayoclinic.org
Mayo Clinic. (2022a). Kegel exercises: A how-to-do guide for women. https://www.mayoclinic.org
Mayo Clinic. (2022b). Fecal incontinence: Diagnosis and treatment. https://www.mayoclinic.org
Mayo Clinic. (2020). Peyronie’s disease: Symptoms & causes. https://www.mayoclinic.org
Mazur-Bialy AI, Kołomańska-Bogucka D, Opławski M, & Tim S. (2020). Physiotherapy for prevention and treatment of fecal incontinence in women—systemic review methods. Journal of Clinical Medicine, 9(10), 3255. https://doi.org/10. 3390/jcm9103255
National Association for Continence (NAFC). (2022a). Adult bedwetting (sleep enuresis). https://www.nafc.org
National Association for Continence (NAFC). (2022b) Male incontinence products. https://nafc.org
National Association for Continence (NAFC). (2022c). Urinary tract infections: Causes and treatments. https://nafc.org
National Association for Continence (NAFC). (2022d). Peyronie’s disease causes and treatment options. https://nafc.org
National Institute of Diabetes and Digestive and Kidney Disorders (NIDDK). (2020). Penile curvature (Peyronie’s disease): What is Peyronie’s disease? https://www.niddk.nih.gov
National Institute of Diabetes and Digestive and Kidney Disorders (NIDDK). (2017). Bowel control problems (fecal incontinence). https://www.niddk.nih.gov
Pizzol D, Demurtas J, Celotto S, Maggi S, Smith L, Angiolelli G, Trott M, et al. (2021). Urinary incontinence and quality of life: A systemic review and meta-analysis. Aging Clinical and Experimental Research, 33(1), 25–35. https://doi.org/10.1007/s40520-020-01712-y
Quinn G. (2021). How OTs and PTs can assess and treat geriatric incontinence. https://www.foxrehab.org
Ranjbar A, Mehrnoush V, Darsareh F, Kotb A, Zakaria A, Shekari M, & Jahromi MS. (2022). Vaginal laser therapy for stress urinary incontinence: A systematic review of prospective randomized clinical trials. Journal of Menopausal Medicine, 28(3), 103–11. https://doi.org/10.6118/jmm.22017
Rosenman A. (2023). Childbirth and incontinence: Things you should know. UCLA Health. https://www.uclahealth.org
Rosenzweig A. (2023). Overview of the mini-mental state exam for Alzheimer’s. Verywellhealth. https://www.verywellhealth.com
Sayner A & Nahon I. (2020). Pelvic floor muscle training in radical prostatectomy and recent understanding of the male continence mechanism: A review. Seminars in Oncology Nursing, 36(4). https://doi.org/10.1016/j.soncn.2020.151050
Shenot PJ. (2023). Urinary incontinence in adults. Merck Manuals. https://www.merckmanuals.com
Simon Foundation for Continence (SFC). (2023a). Bladder health and aging—Fact sheet. https://simonfoundation.org
Simon Foundation for Continence (SFC). (2023b). Medications that may cause or worsen incontinence. https://simonfoundation.org
Simon Foundation for Continence (SFC). (2023c). Smoking and incontinence. https://simonfoundation.org
Stratton KL. (2022). Pelvic floor muscle training exercises. MedlinePlus. https://medlineplus.gov
Tran LH & Puckett Y. (2023). Urinary incontinence. StatPearls Publishing. https://www.ncbi.nlm.nih.gov
University of Utah Health. (2023). Urethral strictures & radiation treatment after cancer. https://healthcare.utah.edu
Urology Care Foundation (UCF). (2023). Urinary incontinence. https://www.urologyhealth.org
Urology Care Foundation (UCF). (2020). What is Peyronie’s disease? https://www.urologyhealth.org
Wound, Ostomy, and Continence Nurses Society (WOCN). (2021). Core curriculum: Continence management (2nd ed.) (J Ermer-Seltun & S Engberg, Eds.). Wolters Kluwer.
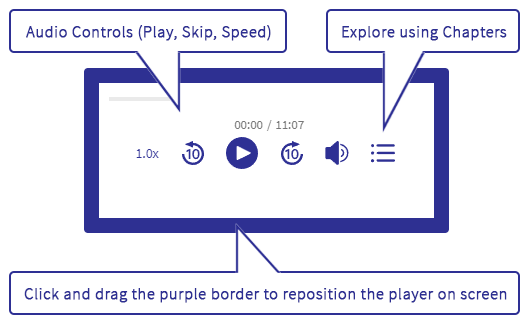





Customer Rating
5.0 / 426 ratings