Bioterrorism and Weapons of Mass Destruction
Emergency Preparedness for Nevada Nurses
Online Continuing Education Course

Course Description
Fulfills 4-hour Nevada nursing CEU bioterrorism training requirement relating to the medical consequences of an act of terrorism that involves the use of a weapon of mass destruction (WMD). Prepare for and respond effectively to an act of bioterrorism, including methods of protection for NV nurses (RN/LPN) and patients, and the role of HAN and NVHAN.
"Very pertinent and useful information." - Diana, RN in Nevada
"Excellent course for a very complicated topic." - Bonnie, RN in Nevada
"This course reminded me, as a practicing RN, about many of the possible scenarios from disasters that are not normally experienced on the job. A wonderful refresher." - Karen, RN in Nevada
"Very thorough and informative." - Victoria, RN in Nevada
Bioterrorism and Weapons of Mass Destruction
Emergency Preparedness for Nevada Nurses
Copyright © 2024 Wild Iris Medical Education, Inc. All Rights Reserved.
LEARNING OUTCOME AND OBJECTIVES: Upon completion of this course, you will have increased your knowledge of the medical consequences of acts of terrorism involving the use of weapons of mass destruction and be better prepared to protect and care for yourself and your patients during emergencies relating to such an event. Specific learning objectives to address potential knowledge gaps include:
- Describe terrorism and weapons of mass destruction (WMDs).
- Identify appropriate personal protective equipment (PPE) to be used when treating patients potentially or actually exposed to biological, chemical, and nuclear agents.
- Discuss preparedness and response to biological, chemical, and nuclear agents.
- Review signs and symptoms of exposure to and emergency treatment for patients exposed to biological, chemical, and nuclear agents.
- Describe syndromic surveillance and reporting procedures.
- Explain the Health Alert Network (HAN), including its purpose and the features unique to the Nevada HAN.
TABLE OF CONTENTS
OVERVIEW
Over the recent past there has been a markedly increased number of foreign and domestic terrorizing attacks such as mass shootings, bombings, biological attacks, and mass casualty incidents in the United States. Such events have led to an awareness that the U.S. population is at increasing risk for such events in the future and must be prepared to respond quickly and effectively in order to mitigate loss of life and overall impact.
Healthcare professionals in particular must be ready and able to respond to an act of terrorism. This requires education and a basic working knowledge of potential biological, chemical, and nuclear agents that may be deployed as well as the treatment options available to counteract their ill effects.
What Is Terrorism?
The U.S. Department of Defense (DOD) defines terrorism as “the unlawful use of violence or threat of violence, often motivated by religious, political, or other ideologic beliefs, to instill fear and coerce individuals, governments, or societies in pursuit of terrorist goals” (U.S. DOD, 2021).
The Federal Bureau of Investigation (FBI) differentiates between international terrorism and domestic terrorism:
- International terrorism: Violent, criminal acts committed by individuals and/or groups who are inspired by, or associated with, designated foreign terrorist organizations or nations (state-sponsored)
- Domestic terrorism: Violent, criminal acts committed by individuals and/or groups to further ideologic goals stemming from domestic influences, such as those of a political, religious, social, racial, or environmental nature
(FBI, n.d.-a)
The overall goal of terrorism is “to destroy the public’s sense of security in the places most familiar to them.” Major targets of terrorism may include buildings or other locations that are important economic or political symbols (Britannica, 2024).
Aside from the underlying motivation for a terrorist attack, the goals of the attacks themselves are to bring about:
- Mass casualties
- Loss of critical resources
- Disruption of vital services
- Disruption of the economy
(FEMA, 2019)
Terrorist Acts as Mass Casualty Incidents
Terrorist violence may include the use of explosive, biological, chemical, or nuclear means targeted in order to result in mass or multiple casualties.
A mass casualty incident (MCI or MASCAL) is an event that significantly overwhelms the local resources and capabilities in a short period of time. The key factor is the relationship between the number of casualties generated and the capabilities and resources of the receiving facility or facilities (DeNolf & Kahwaji, 2022). Examples of MCIs include:
- 2024 shooting in Chicago over the Independence Day weekend, with more than 100 people shot and 18 fatalities
- 2024 school shooting at Georgia high school, with four deaths and at least nine injuries
- 2021 intentional SUV crash into crowd at Wisconsin Christmas parade, leaving five dead and 40 injured
- 2019 shooting at an El Paso, Texas, Walmart store, which left 22 dead and 23 injured
- 2017 shooting at the Route 91 concert in Las Vegas, which left 58 victims dead and 851 injured
- 2017 shooting in a church in Sutherland Springs, Texas, which left 27 dead, including 9 children, and 30 injured
- 2013 terrorist attack near the finish line of the Boston Marathon, in which a pair of homemade bombs were detonated in the crowd watching the race, killing 3 people and injuring more than 260
(Ray, 2022; JEMS, 2024)
A second, less frequently used term is multiple casualty incident. Although superficially similar to a mass casualty incident, this term carries a different meaning for first responders and first receivers of trauma victims. Unlike a mass casualty incident, a multiple casualty incident:
- Can be managed with heightened response by a single EMS agency or system
- Typically does not overwhelm the hospital capabilities of a jurisdiction and/or region but may exceed the capabilities of one or more hospitals within a locality
- Usually produces a short, intense peak demand for health and medical services, unlike the sustained demand typical of a mass casualty incident
(EMS1, 2023)
Characteristics of Targets
Targets for terrorism are referred to as “hard” or “soft.” Most of the terrorism today is aimed at soft targets.
- Hard targets are crowded places with high-security measures against terrorism. Examples include:
- Military or government facilities
- Key industries
- Key transportation facilities
- Banking and finance
- Soft targets are places with high concentration of civilians without a direct association with the government and with low or no security measures against terrorism. Examples include:
- Schools
- Theaters and cinemas
- Civilian businesses
- Churches
- Hotels, bars, clubs
- Train and bus stations
- Shopping malls
- Venues such as parades, athletic events, or concerts
Nature of an Attack
An act of terrorism may be either covert or overt. The timing and/or sequencing of an attack are also factors that can impact numbers and types of casualties as well as the number and mix of available first responders.
A covert attack takes its advantage from the element of surprise. A covert operation is an activity that is planned and executed to conceal the identify of or permit plausible deniability by the attacker(s). This type of attack is also called clandestine.
An overt attack is openly acknowledged by or is readily attributable to the attackers without concealment.
After an initial attack, terrorists may try to target others by using a secondary attack. Secondary devices may be found in any configuration, not limited to the primary attack method. Tactics that terrorists may use include:
- Use of a secondary device to target first responders and onlookers
- Terrorist impersonation of first responders to gain access to a secure site and create more victims
- Swatting, which refers to making a hoax 911 call to draw a response from first responders or police
- Diversion to draw first responders away from the intended primary target of attack and/or as part of a complex multipronged attack
(JCAT, n.d.)
Weapons of Mass Destruction (WMDs)
According to the U.S. DOD (2021), WMDs are weapons capable of a high order of destruction or causing a large number of casualties, and excluding the means of transporting or propelling the weapon where such means is a separable and divisible part from the weapon. (An example of such excluded means would be an airplane used to deliver a bomb, such as occurred on 9/11.)
TYPES OF WMDS
The acronym CBRNE is a method of describing the types of weapons of mass destruction that can be used by terrorists:
- Chemical
- Biological
- Radiologic
- Nuclear
- Explosives, high yield
Over the years, terrorist groups have tested new ways and means to acquire and use more dangerous weapons to maximize damage and incite terror. As advancements are made in technology and with the expanded legal and illegal commercial channels, including the dark web, some of these weapons have become increasingly accessible (UN, n.d.).
This course will focus on specific implications of the triad of nuclear/radiologic, biological, and chemical—or “NBC”—weapons. It will not cover caring for victims of solely incendiary and/or explosive weapons. The general principles of trauma care apply to patients suffering from burn or blast injuries no matter the source.
PERSONAL PROTECTIVE EQUIPMENT (PPE)
When responding to a WMD incident, responders and healthcare personnel must consider the agent used and the route of dispersal. Knowing these can help determine what personal protective equipment (PPE) is needed, the method of decontamination, and expectation as to the number of possible victims.
Dispersal of biological, chemical, or nuclear contaminants can occur via:
- Aerosolization
- Thermal detonation
- Contamination of food and water
- Human-to-human contact
(Zhang & Wang, 2022)
Regardless of the type of dispersal method used, intended victims are contaminated via three routes: skin, gastrointestinal, and pulmonary.
PPE and Exposure Risks
Just as with Standard Precautions and transmission-based precautions, the components of appropriate PPE are determined by the nature of the anticipated exposure. This includes:
- The nature of the known or suspected hazardous agent (biological, radiologic, or chemical), which is the most important factor
- The method(s) of dispersal and exposure (inhalation, skin absorption, ingestion, eye or skin contact)
- The circumstances under which a care provider is exposed
(U.S. DHHS, 2024a)
The last is exceptionally important: the closer in time and place the victim is to the exposure incident, the greater the risk to the care provider. This is the rationale for the distinctions between first responder and first receiver (see box below).
FIRST RESPONDERS VS. FIRST RECEIVERS
First responders are personnel who are responsible for going immediately to the scene of an accident of emergency to provide assistance. Some examples are firefighters, HAZMAT team members, law enforcement officers, lifeguards, forestry personnel, ambulance attendants, and other public service personnel. In the case of hazardous materials incidents, these personnel typically respond at the site where the incident occurred (Merriam-Webster, 2024).
First receivers are personnel at a hospital or other care site who have a role in receiving and treating contaminated victims, which may include triage, decontamination, medical treatment, and security. In mass casualty incidents, many individuals will arrive at a hospital without having been decontaminated and/or cared for by first responders at the site. For example, it is not uncommon for victims to arrive via private car, taxi, or ride-sharing app (Shertz, 2024).
Levels of Protection
There are four levels of protection and associated protective equipment, which range from the most protection (A) to the least (D). Protection level is assigned based on the hazardous substance being confronted and must adequately protect the individual from any type of biological, physical, or chemical exposure.
| Level | Protection Provided |
|---|---|
| (U.S. DHHS, 2024a) | |
| A | Highest level of respiratory, skin, and eye protection |
| B | Highest level of respiratory protection, but lesser level of skin and outer body protection |
| C | Lower level of respiratory protection; liquid splash protection |
| D | Environmental nuisance contamination only; no respiratory or chemical protection |
LEVEL A PPE
Level A protection is used by first responders when the greatest potential for exposure to hazards exists and when the greatest level of skin, respiratory, and eye protection is required.
Elements:
- Positive-pressure (pressure demand), self-contained breathing apparatus (SCBA) (NIOSH approved), or positive-pressure supplied air respirator with escape SCBA
- Fully encapsulating chemical protective suit
- Gloves, chemical-resistant inner and outer
- Boots, chemical-resistant outer, steel toe and shank (depending on suit boot construction, worn over or under suit boot)
(U.S. DHHS, 2024a)

Level A–equivalent totally encapsulating chemical- and vapor-protective suit. (Source: U.S. DHHS, 2024b.)
LEVEL B PPE
Level B protection is necessary for first responders under circumstances requiring the highest level of respiratory protection, with a lesser level of skin and eye protection. It is used when ambient atmospheric vapors or gas levels have not approached sufficiently high concentrations to warrant Level A protection.
Elements:
- Positive-pressure (pressure-demand) SCBA (NIOSH approved), or positive-pressure supplied air respirator with escape SCBA
- Chemical-resistant clothing (overalls and long-sleeved jacket, coveralls, hooded two-piece chemical splash suit, disposable chemical-resistant coveralls)
- Gloves, chemical-resistant inner and outer
- Boots, chemical-resistant outer, steel toe and shank
(U.S. DHHS, 2024a)
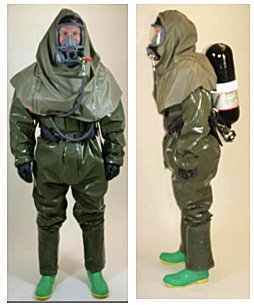
Level B–equivalent non–gas-tight encapsulating suit. (Source: U.S. DHHS, 2024b.)
LEVEL C PPE
Level C protection is required for first responders and first receivers when the type of airborne substance is known, concentration measured, criteria for using air-purifying respirators met, and skin and eye exposure unlikely. Periodic monitoring of the air must be performed.
Elements:
- Full-face or half-mask, air-purifying respirator (NIOSH approved)
- Chemical-resistant clothing (one-piece coverall, hooded two-piece chemical splash suit, chemical-resistant hood and apron, disposable chemical-resistant coveralls)
- Safety helmet
- Gloves, chemical-resistant inner and outer
- Boots, chemical-resistant, steel toe and shank
(U.S. DHHS, 2024a)

Level C–equivalent PPE. (Source: U.S. DHHS, 2024b.)
LEVEL D PPE
Level D protection is primarily a work uniform and is used for nuisance contamination only. It requires only coveralls and safety shoes/boots. Other PPE is based upon the situation (types of gloves, etc.). Level D is not to be worn on any site where respiratory or skin hazards exist (U.S. DHHS, 2024a).

Level D–equivalent PPE. (Source: U.S. DHHS, 2024b.)
BIOLOGICAL TERRORISM PREPAREDNESS AND RESPONSE
The U.S. Department of Homeland Security (2022) defines biological attack as “the intentional release of a pathogen (disease causing agent) or biotoxin (poisonous substance produced by a living organism) against humans, plants, or animals. An attack against people could be used to cause illness, death, fear, societal disruption, and economic damage.”
The department distinguishes between two kinds of biological agents:
- Transmissible agents that spread from person to person (e.g., smallpox, Ebola) or animal to animal (e.g., foot-and-mouth disease)
- Agents that may cause adverse effects in exposed individuals but that do not make those individuals contagious to others (e.g., anthrax, botulinum toxin)
Biological weapons are a common choice for terrorist organizations due to their ease of being deployed, the devastating effects they cause, and how inexpensive they are to produce. There is, however, an unpredictability in that these weapons may affect the intended victims and, inadvertently, the perpetrators (Rathish et al., 2023).
BIOLOGICAL INCIDENTS
Countries, groups, and individuals have attempted/used agents of bioterrorism to cause fear and panic. This is not a recent phenomenon. One of the earliest occurrences of bioterrorism was recorded in the sixth century B.C.E. when Persian armies poisoned wells with a fungus (CDC, 2020b).
Recently, a Marine Corps University report described biotechnology advances that have increased the risk for North Atlantic Treaty Organization (NATO) forces being confronted with a biological weapon by 2030 (Juling, 2023).
Examples of biological terrorism (both planned and implemented) include:
- 1972: Two college students were arrested for planning to poison the Chicago water supply with typhoid bacteria.
- 1984: Followers of Bhagwan Shree Rajneesh in Oregon infected doorknobs and salad bars in restaurants with Salmonella typhimurium bacteria in order to affect a local election.
- 2001: Mail laced with infectious anthrax was delivered to offices of the news media and members of the U.S. Congress.
- 2003: The first U.S. case occurred of letters filled with ricin toxin; the perpetrator has never been identified.
- 2003: Al-Qaeda terror cells in Great Britain, Spain, Italy, Turkey, Sweden, and Germany planned attacks with ricin toxin; suspects were found and arrested.
- 2013: Ricin letters were sent to a number of American politicians.
- 2014: A laptop discovered in Syria contained many instructions for the construction, storage, and delivery of weapons of mass destruction.
- 2020: The COVID-19 pandemic triggered various extremist groups to call for the virus to be spread and infect specific religious or ethnic groups.
(CDC, 2020b; Juling, 2023)
Mode of Transmission
Biological agents can be very difficult to detect, and many do not cause illness for several hours or even days. These agents are most likely to be dispersed as aerosols so as to spread among large populations more easily. Some, however, are spread from person to person or by vectors, ingestion, direct contact, or other methods. Water systems are rarely a target; however, water systems have received threats, and because the possibility exists that these threats could be carried out, they must be taken seriously.
Biological weapons include bacteria, viruses, fungi, and toxins. While the standard chain of infection applies to diseases caused by exposure to a pathogen, the obvious difference is the mode of transmission link when it is used as a weapon.
- Naturally occurring disease is almost always spread unintentionally. In many cases, it occurs as part of carrying out normal daily activities, with a contaminated hand or uncovered sneeze passing on the infectious agent.
- Intentional spread indicates biological terrorism.
(Rathish et al., 2023; Hayoun & King, 2024)
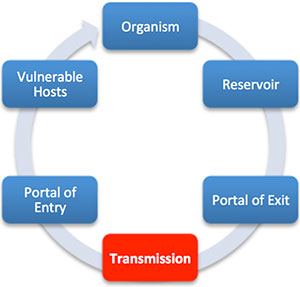
Chain of infection. In biological terrorism, the mode of transmission is intentional. (Source: Wild Iris Medical Education, Inc.)
Bioweapon Classification Categories
The Centers for Disease Control and Prevention (CDC) has separated bioterrorism agents into three categories, depending on how easily they can be spread and the severity of illness or death they cause. Factors that contribute to these categories include:
- Ability to have a profound impact on health
- Ability to cause health fears
- Potential for spread
- Availability of protective vaccines or antimicrobial agents
- Secondary transmission potential
- Public health preparedness
CATEGORY A
These high-priority agents include organisms that pose the highest risk to the public and national security because they:
- Can be easily disseminated or transmitted from person to person
- Result in high mortality rates and have the potential for a major public health impact
- Might cause public panic and social disruption
- Require special action for public health preparedness
Category A agents and diseases include:
- Anthrax (Bacillus anthracis)
- Botulism (Clostridium botulinum toxin)
- Plague (Yersinia pestis)
- Smallpox (variola major)
- Tularemia (Francisella tularensis)
- Viral hemorrhagic fevers, including filoviruses (Ebola, Marburg) and arenaviruses (Lassa, Machupo)
(CDC, 2018, 2020a; Rathish et al., 2023)
CATEGORY B
Second-highest-priority agents include those that:
- Are moderately easy to disseminate
- Result in moderate morbidity rates and low mortality rates
- Require specific enhancements of CDC’s diagnostic capacity and enhanced disease surveillance
Category B agents/diseases include:
- Brucellosis (Brucella species)
- Epsilon toxin of Clostridium perfringens
- Food safety threats (Salmonella species, Escherichia coli O157:H7, Shigella)
- Glanders (Burkholderia mallei)
- Melioidosis (Burkholderia pseudomallei)
- Psittacosis (Chlamydia psittaci)
- Q fever (Coxiella burnetii)
- Ricin toxin from Ricinus communis (castor beans)
- Abrin toxin from jequirity (rosary) peas
- Staphylococcal enterotoxin B
- Typhus fever (Rickettsia prowazekii)
- Viral encephalitis (alphaviruses, such as eastern equine encephalitis, Venezuelan equine encephalitis, and western equine encephalitis)
- Water safety threats (Vibrio cholerae, Cryptosporidium parvum)
(CDC, 2020a; CDC, 2018; Rathish et al., 2023)
CATEGORY C
Third-highest-priority agents include emerging pathogens that could be engineered for mass dissemination in the future because of:
- Availability
- Ease of production and dissemination
- Potential for high morbidity and mortality rates and major health impact
Category C agents/diseases include:
- Emerging infectious diseases such as Nipah virus and hantavirus
(CDC, 2020a; CDC, 2018; Rathish et al., 2023)
COVID-19 AND BIOTERRORISM
The intelligence community has examined the potential for terrorists to weaponize the COVID-19 virus, particularly against high-level targets. It has been found that the COVID-19 virus, despite the high number of deaths and significant illnesses it has caused, does not have the desired characteristics of a biological weapon. While strains of COVID-19 could be acquired and cultured in a laboratory, its ability to be disseminated from a point or line source is questionable and is too unpredictable as to its effects on a targeted population.
Nevertheless, the COVID pandemic has revealed several weaknesses in government and population response that increase our vulnerability to bioterrorism and reduce our bioweapon deterrence. In addition, adversaries have witnessed this response and can make use of it (Mauroni, 2021).
Category A Diseases with Potential for Use as Bioweapons
ANTHRAX
Bacillus anthracis is a spore-forming organism, with the spores being the infectious element. In its natural state, it is present in the soil, where it may be ingested by grazing animals. It can be transmitted to humans by handling or ingesting contaminated animals, animal products, or soil. Unless exposure is due to an intentional release, anthrax infections are very rare. There are two types of anthrax: inhalation and cutaneous.
ANTHRAX ATTACKS
Seven days after the attacks of 9/11, anonymous letters laced with anthrax began arriving at news media companies and congressional offices. Over the following months, five people died from inhaling anthrax, and 17 others were infected after exposure. Some 10,000 U.S. residents took two months of antibiotics for possible anthrax exposure. Because the anthrax was of weapons grade or near weapons grade, it appears to have come from a sophisticated laboratory. The perpetrator(s) of these attacks has not yet been identified. Extensive FBI investigations have failed to determine the sender’s exact motive, but the letters included the lines “Death to America,” “Death to Israel,” and “Allah is great” (FBI, n.d.-b).
Inhalation Anthrax
Inhalation anthrax is considered to be the deadliest form of the disease. Infection usually develops within a week following exposure but can take up to two months. Without treatment, inhalation anthrax is almost always fatal. However, if treated aggressively, about 55% of individuals survive. Inhalation anthrax is not contagious.
| (CDC, n.d.-a; Mayo Clinic, 2023a; OSHA, n.d.-a; Williams et al., 2023) | |
| Signs/symptoms |
Initially:
Later:
|
| Treatment |
|
| Personal protective equipment |
|
Cutaneous Anthrax
Cutaneous anthrax is the most common form of anthrax infection and is also considered to be the least dangerous. Infection usually begins 1 to 7 days following exposure. This can happen when anthrax spores enter the skin, usually through a cut or scrape, or while handling infected animals or contaminated animal products. Cutaneous anthrax is most common on the head, neck, forearms, and hands. Without treatment, up to 20% of people with cutaneous anthrax die. With proper treatment, almost all patients with this form of anthrax survive.
| (CDC, n.d.-a; Mayo Clinic, 2023a; OSHA, n.d.-a; Williams et al, 2023) | |
| Signs/symptoms |
Within 2 weeks of exposure:
|
|---|---|
| Treatment |
|
| Personal protective equipment |
|
BOTULISM
Clostridium botulinum is also a soil-inhabiting, spore-forming organism. The neurotoxin it forms is extremely potent and is one of the deadliest toxins known; less than 1 microgram is fatal for adults. It causes difficulty breathing, muscle paralysis, and, if untreated, possible death. Botulism can be contracted by ingesting contaminated canned, smoked, or vacuum-packed foods and also by inhaling spores. Human botulism may refer to inhalation, infant, foodborne, or wound botulism. Inhalation of the toxin is rare.
The botulism bacteria are found to occur naturally in a variety of places but rarely cause illness, even if they are eaten. There are certain conditions, however, in which spores grow and make one of the most lethal toxins known. These conditions are:
- Low- or no-oxygen environment
- Low acid
- Low sugar, low salt
- Temperature range 68–113 °F (20–45 °C)
(UF/IFAS Extension, 2024)
| (CDC, 2024a) | |
| Signs/symptoms in adults |
No matter how a person acquires botulism, the symptoms are usually the same, with the defining feature of weakness beginning on both sides of the face, going down the neck and to the rest of the body. Initially:
Other symptoms that can follow:
|
|---|---|
| Signs/symptoms in infants |
|
| Treatment |
|
| Personal protective equipment |
|
PLAGUE
Yersinia pestis is a bacterium that causes acute, potentially fatal infections in both humans and animals. It is naturally occurring in environments in which rats and their fleas exist. Plague has occurred in rural and semirural areas of the western United States, primarily in semiarid upland forests and grasslands. In addition, wild carnivores can become infected by consuming infected prey. Plague can be deadly if not treated promptly with antibiotics. The rarest and deadliest form of plague affects the lungs and can spread from person to person.
Plague is rarely naturally transmitted by inhalation, but that is the most likely means if the organism were to be released intentionally. If released as an aerosol, an outbreak of pneumonic plague is the anticipated result. A plague vaccine is no longer available in the United States. New vaccines are in development but are not expected to be commercially available in the immediate future (CDC, n.d.-b).
Although plague has long been referred to a disease of the Middle Ages, there have been a number of outbreaks in India and Africa during the last 20 years. Thus, plague is now considered to be a reemerging disease. It is hypothesized that the plague’s reemergence may be due to global warming. Globally, the three most endemic countries are Madagascar, the Democratic Republic of Congo, and Peru. Cases have also been reported in the United States (Minnaganti, 2024).
Plague can take different clinical forms, but the most common are bubonic, pneumonic, and septicemic.
Bubonic Plague
Bubonic plague is an infection of the lymphatic system and is usually the result of an infected flea bite. The bacteria multiply in a lymph node near where the bacteria entered and can spread to other areas of the body. Without treatment, the mortality rate is 60%.
| (Minnaganti, 2024; CDC, n.d.-b; WHO, 2022) | |
| Signs/symptoms |
In the first several days:
2–6 days following exposure:
|
|---|---|
| Treatment |
|
| Personal protective equipment |
|
Pneumonic Plague
Pneumonic plague may develop from inhaling infectious droplets or from untreated bubonic or septicemic plague that spreads to the lungs. Pneumonic plague is the most serious form of the disease and is the only form of plague that can spread from person to person. Without treatment the mortality rate is 100%, and with treatment it is 50%.
| (Minnaganti, 2024; CDC, n.d.-b; WHO, 2022) | |
| Signs/symptoms |
1–3 days after inhalation:
|
|---|---|
| Treatment |
|
| Personal protective equipment |
|
Septicemic Plague
Septicemic plague can occur as the first symptoms of plague or may develop from untreated bubonic plague. This form results from bites of infected fleas or from handling an infected animal. Septicemic plague is frequently associated with delayed diagnosis, and has a higher fatality rate than primary bubonic plague.
| (Minnaganti, 2024; CDC, n.d.-b; WHO, 2022) | |
| Signs/symptoms |
Acute onset of:
May progress to include:
|
|---|---|
| Treatment |
|
| Personal protective equipment |
|
SMALLPOX
The variola virus causes smallpox in two forms. Variola major is the most common and most severe. It has a historic fatality rate of approximately 30%. Variola minor is less common and less severe, with a historic fatality rate of ≤1%.
Smallpox eradication, one of the greatest successes of modern public health, was officially declared worldwide in 1980. The last known case of naturally occurring smallpox was reported in 1977 in Somalia. The last known case in the United States occurred in 1949. Today the smallpox virus is known to exist only in secured research laboratory stockpiles in the United States and Russia. However, advances in synthetic biology have made it possible to create smallpox. Therefore, there is concern that it could someday be used as a biological warfare agent.
Smallpox can be transmitted directly and indirectly from person to person and via contaminated items. Transmission begins with virus particles being sloughed from the oropharyngeal lesions of an infected person. Inhalation of airborne droplets of this saliva introduces the disease to a new host.
The most important way to prevent transmission of smallpox is by vaccination (Mayo Clinic, 2022; Simonsen & Snowden, 2023).
| (Mayo Clinic, 2022; Simonsen & Snowden, 2023) | |
| Signs/symptoms |
|
|---|---|
| Treatment |
|
| Personal protective equipment |
|
Category B Diseases with Potential for Use as Bioweapons
Ricin and abrin are both biological toxins derived from plants; they are classified as either a biological or chemical weapon. Ricin comes from the beans of the castor plant and abrin comes from jequirity (rosary) peas. One molecule of either toxin is capable of poisoning all of the ribosomes in a cell, leading to cell death. Abrin is more lethal than ricin.
Ricin has been used in injectable form in assassination attempts, but mass casualties would probably involve inhalation of aerosolized toxin.
| (Madsen, 2024; Stoppler & Shiel, n.d.) | |
| Signs/symptoms |
Inhalational exposure: Latent period of 4–8 hours, followed by:
Ingestion exposure:
|
|---|---|
| Treatment |
First responder:
First receiver:
|
| Personal protective equipment |
|
CHEMICAL TERRORISM PREPAREDNESS AND RESPONSE
Chemicals are part of our daily lives, existing in the products we use every day. All chemicals can result in problems if used improperly and can be destructive when used as an agent of terrorism.
Chemical weapons cause injury or death by means of their high toxicity, usually when inhaled or in contact with the skin. The first widespread use of chemical weapons was in World War I. By the end of the war, 17 different toxic agents had been used to kill 100,000 soldiers and civilians and injure at least a million more.
In 1925 the Geneva Protocol prohibited the use of chemical and biological weapons in war, and at a subsequent United Nations Conference in 1997, a Chemical Weapons Convention banned the use of chemical weapons as well as their development, production, stockpiling, and transfer. Destruction of these weapons, however, has been slow, and there are tens of thousands of tons still stockpiled in arsenals around the world.
Agents used in chemical terrorism include poisonous vapors, aerosols, liquids, or solids, all of which are volatile and have toxic effects on either humans, animals, or plants. Some of these chemical agents can be undetectable, as they may be odorless and tasteless, and they can have an immediate or a delayed effect. However, chemical agents dissipate quickly in open air and can be difficult to deliver in lethal concentrations. They are also difficult to produce (Williams et al., 2023; Arms Control Association, 2024).
Weaponization of Chemical Agents
Several factors must be considered when deciding how to deliver a chemical agent to a target. These include lethality, persistency, and physiologic effect.
The amount of agent needed to produce incapacitation or death varies with the type of agent. Older agents require burdensome amounts of chemical on a target. The creation of nerve agents allows for an increase in lethality and decrease in quantity that needs to be delivered.
Some agents are persistent, remaining in effect for extended lengths of time, and others are nonpersistent, dissipating in minutes or a few hours. Persistent agents are most dangerous to the skin, and nonpersistent are more dangerous to the lungs (WPNAC, n.d.).
Dispersal of Chemical Agents
Toxic chemicals can enter the body in several ways, most importantly through inhalation or absorption through the skin. In general, the effect of an agent in contact with the skin is much slower than when inhaled.
Chemical agents can be dispersed in gas, liquid, and solid forms by aerosolization, an exploding device, or contaminating food or water. They can be released by bombs; sprayed from aircraft, boats, or vehicles; or used in liquid form to create a hazard to people and the environment.
These weapons can be unitary or binary. Unitary weapons are effective on their own and do not require mixing with other agents. They are stored in ready-to-use form and pose a considerable risk to those working with them.
Binary weapons development began in the 1960s and involves the use of toxic agents and nontoxic precursors. When these weapons are deployed, the precursors mix with and develop the agent. Binary agents are safe to handle and store and are harder to detect (Velez-Daubon et al., 2021; WPNAC, n.d.).
Categories of Chemical Weapons
There are five major types of chemical agents:
- Vesicants (blister agents)
- Lung-damaging (pulmonary) agents
- Blood agents
- Nerve agents
- Incapacitating agents/riot control agents
(Williams et al., 2023; WPNAC, n.d.)
VESICANTS (BLISTER AGENTS)
A vesicant, or blister agent, is named for its ability to cause severe and painful chemical water blisters on the bodies of affected persons. Vesicants have medical uses but are fatal if small amounts are ingested. Casualties generally result from absorption through the skin and require three weeks to three months for recovery.
Vesicants are oily reactive chemicals that combine with DNA and proteins to cause cellular changes within minutes to hours after exposure. Some agents have characteristic odors (e.g., sulfur mustard has been described as smelling like mustard, garlic, horseradish, or asphalt, and lewisite smells like geraniums). These agents include:
- Distilled mustard
- Mustard gas
- Mustard/T
- Sulfur mustard
- Nitrogen mustard
- Mustard/lewisite
- Lewisite
- Phosgene oxide
Factors that contribute to the time of onset and the severity of illness include the:
- Amount and route of exposure to the vesicant
- Type of vesicant
- Baseline health condition of the exposed person
(Williams et al., 2023; WPNAC, n.d.)
| (Madsen, 2024) | |
| Signs/symptoms |
Mustard compounds target the skin, eyes, respiratory tract, and bone marrow, causing:
Lewisite causes:
Phosgene oxime causes:
|
|---|---|
| Treatment |
First responder:
First receiver:
|
| Personal protective equipment |
|
CHOKING AGENTS
Choking/lung/pulmonary agents are chemicals that cause severe irritation or swelling of the respiratory tract (lining of the nose, throat, and lungs). Chemicals such as ammonia, chlorine, and phosgene cause eye, nose, and throat irritation, cough, wheezes, and dyspnea, which is known as irritant gas syndrome.
Clinically relevant routes of exposure include the mouth, nose, and mucosal membranes. The organ systems generally affected include the upper respiratory tract (airway and bronchi) and lower respiratory tract (air space and alveoli).
These agents include:
- Chlorine
- Phosgene
- Ammonia
(Lung, 2024; Madsen, 2024; WPNAC, n.d.)
| (Madsen, 2024; WPNAC, n.d.) | |
| Signs/symptoms |
Initial effects:
Upper respiratory effects (immediate):
Lower pulmonary effects (progressive):
Progression may include:
|
|---|---|
| Treatment |
First responder:
First receiver:
|
| Personal protective equipment |
|
BLOOD AGENTS
A blood agent is a toxic compound that affects the body by being absorbed into the blood and blocking the enzyme necessary for aerobic metabolism, depriving red blood cells of oxygen and causing asphyxiation. Blood agents are fast-acting, highly lethal toxins that are typically volatile colorless gases. They are usually either arsenic or cyanide based, and include:
- Hydrogen cyanide
- Cyanogen chloride
Hydrogen cyanide can be dispersed as a nonpersistent vapor and can break down gas-mask and vehicle filters. Hydrogen cyanide smells like peach pits or bitter almonds.
People exposed to a small amount of cyanide by breathing it, absorbing it through their skin, or eating foods that contain it may have some or all of the following signs and symptoms and will die within 1 to 20 minutes.
| (WPNAC, n.d.; Williams et al., 2023) | |
| Signs/symptoms |
|
|---|---|
| Treatment |
|
| Personal protective equipment |
|
NERVE AGENTS
Nerve agents are the deadliest chemical agents and difficult to produce. They interact with enzymes in the body that carry signals between nerves and muscles; ultimately, they paralyze the body’s nervous system, leading to respiratory failure and death by asphyxiation. Just a few droplets are capable of killing within minutes if inhaled or within hours if absorbed through the skin.
Nerve agents include:
- Sarin
- Soman
- Tabun
- VX
Sarin is rapidly dispersed by even moderate winds. VX is an oily liquid; it may remain in place for weeks or longer and is readily absorbed through the skin (Lung, 2024; WPNAC, n.d.).
| (Lung, 2024; WPNAC, n.d.; Williams et al., 2023) | |
| Presentation |
Overstimulation and eventual fatigue of the CNS, leading to:
Overstimulation and eventual fatigue of skeletal muscles, causing:
Overstimulation of exocrine glands, causing excessive:
Death, usually due to central apnea, but direct paralysis of the diaphragm, bronchospasm, and bronchorrhea can also contribute |
|---|---|
| Treatment |
First responder:
First receiver:
|
| Personal protective equipment |
|
CASE
A woman walked into a casino showgirls’ dressing room 30 minutes before the first show of the evening. In the controlled chaos, no one noticed her enter the room, pause by the door, or set the door lock. Her phone vibrated, signaling that her accomplice was going to throw the breaker for the lights in 10 seconds. The woman punctured the lid of a large food storage container and placed the container on the floor near the door. As the lights went out, she left the room, closing and locking the door behind her.
The 35 dancers in the dressing room panicked and in attempting to reach the door knocked over the container, dispersing sarin and causing the liquid to vaporize. The dancers began inhaling the agent. Several fell, and their skin was exposed to the remaining agent pooled on the floor in liquid form. All of the dancers began experiencing the symptoms of moderate exposure, with those nearest the door having a more immediate, intense reaction.
Their screams alerted other casino employees, who found a note on the locked door calling the dancers “Jezebels” and promising further “saran” attacks. Some employees called 911, while others broke down the door and began to assist their colleagues. Because all of the agent had not evaporated, some rescuers were also exposed and began to experience symptoms.
First responders arrived and identified the situation as a sarin gas exposure. Their assessment included the need to provide antidotes and possible ventilatory support for 40 or more victims. Shortfalls to providing this care were readily apparent.
- An on-site decontamination setup was needed to prevent any additional victims being generated.
- While atropine and diazepam were readily available in the first response vehicle and from their base station in adequate quantities to treat the number of victims, the necessary 2-PAM chloride was not.
The nearest hospital was notified, and it activated its disaster plan. However, it did not have adequate intensive care beds available to treat the number of victims anticipated to require ventilatory support.
The community emergency operations center was immediately contacted. The preprepared decontamination supplies and equipment were dispatched, and the emergency call roster was activated to staff the decontamination area. In accordance with the community plan, other hospitals were notified of the situation and alerted to the potential need to provide supportive care for a large influx of patients.
Previously identified sources for 2-PAM chloride were contacted, and emergent delivery was made to the release site and the facilities poised to receive victims.
INCAPACITATION/RIOT CONTROL AGENTS
Incapacitation and riot control agents are designed to be nonlethal but can cause injury or death because self-preservation behaviors in affected individuals may be overridden or inhibited. These agents produce temporary physiologic or mental effects that render people incapable of performing normal activities.
Incapacitation agents and riot control agents are separate classes of nonlethal agents—anticholinergics and lacrimators. Riot control agents differ from incapacitating agents in several ways. They possess a relatively shorter onset and limited duration of action. They induce short-term toxic effects that subside within minutes following termination of exposure. Incapacitating agents are chemicals that produce a disabling condition that persists for hours to days following exposure. These agents induce changes to the central nervous system without lethal effects.
Incapacitating agents include:
- BZ (3-Quinuclidinyl benzilate)
Riot control agents (often incorrectly referred to as tear gas) are dispersed as solid aerosols or as solutions and include:
- CN (chloroacetophenone, also known as Mace)
- CS (chlorobenzylidene malononitrile, also known as tear gas)
- DM (adamsite, a vomiting agent)
- OC (oleoresin capsicum, also known as pepper spray)
| (Lung, 2024; Madsen, 2024; ALA, 2023) | |
| Signs/symptoms |
Incapacitation agents:
Riot control agents:
|
|---|---|
| Treatment |
Incapacitation agents:
Riot control agents:
|
| Personal protective equipment |
|
Decontamination of Victims of Chemical Agents
Decontamination involves local or spot decontamination of any liquids on the skin, removal of clothing, and copious irrigation of the skin with lukewarm water and, if available, mild soap. Decontamination may be accomplished in the field and also in receiving facilities.
The most important and most effective decontamination of any chemical exposure is done within the first minute or two after exposure.
Field decontamination often consists of setting up stations for disrobing following showering or assisted decontamination. Patients may bypass field decontamination stations, however, and go directly to a medical facility for treatment.
Upon notification of a chemical weapons release, receiving facilities should:
- Secure all entrances and hospital grounds
- Establish a security perimeter
- Set up a decontamination zone outside the clean areas of the facility
- Activate disaster plan
- Establish close communication with local emergency management authorities
Hospital decontamination consists of removal of all clothing and thorough washing of skin and hair with lukewarm water and soap before the patient is brought into the clean area of the emergency department.
Important aspects of planning involved in preparation for decontamination events include:
- Establishment of designated fixed or rapidly deployed decontamination facility
- Properly trained staff in donning and doffing of personal protective equipment
- A triage plan for medical and nonmedical decontamination
- Decontamination procedures that maintain privacy and avoid hypothermia
(Madsen, 2024)
NUCLEAR/RADIOLOGIC TERRORISM PREPAREDNESS AND RESPONSE
Nuclear, or radiologic, weapons are the newest member of the WMD “family.” So far, two nuclear weapons have been used, both by the United States near the end of World War II. These weapons resulted in the immediate deaths of approximately 120,000 people.
Nuclear terrorism might involve the acquisition of or the fabrication of a nuclear weapon such as a radiologic dispersal device (dirty bomb). A dirty bomb is a mix of explosives, such as dynamite, with radioactive powder or pellets. When explosives are set off, the blast carries radioactive material into the surrounding area. Other radiation emergencies may involve an incident at a nuclear power plant, which could release radiation over an area.
Creating a nuclear WMD requires a high degree of scientific knowledge (or the ability to interpret and apply information available on the Internet) as well as access to specific materials and facilities. These technical challenges for making a nuclear explosive, however, should not be regarded as insurmountable. Unlike state-sponsored nuclear weapons developers, terrorists have different requirements for safety, performance, and delivery. Also, the rapid availability of technologic knowledge can further advance terrorists’ weaponization attempts.
Despite thefts of small amounts of fissile material, however, there is no credible evidence that any terrorist group has succeeded in obtaining the necessary multi-kilogram critical mass of weapons-grade plutonium required to make a nuclear weapon (Williams et al., 2023).
NEVADA NATIONAL NUCLEAR SECURITY SITE
A national nuclear security site that uses and creates nuclear material is located just 60 miles from the Las Vegas urban area. Materials delivered to and from the site travel directly through the urban area, increasing the risk for a terrorist attack that could release radioactive materials into the community. To protect the community, agencies have developed a preventive radiologic nuclear detection program designed to prevent the illicit development, transport, or use of radiologic or nuclear materials anywhere in the Las Vegas urban area. This involves primary and advanced secondary radiologic screeners and related detection equipment (FEMA, 2023).
What Is Ionizing Radiation?
Ionizing radiation is a form of radiation that includes alpha and beta particles, gamma rays, X-rays, neutrons, high-speed electrons, and high-speed protons as well as other particles that can produce ions. Ionizing radiation has considerably more energy than non-ionizing radiation. When it moves through materials such as air or living tissue, electrons are displaced. Ionizing radiation can affect the atoms in living things, so it poses a health risk by damaging genetic tissue and DNA.
Sources of ionizing radiation include X-ray machines, cosmic particles from outer space, and radioactive elements such as plutonium. Radioactive elements emit ionizing radiation as their atoms undergo decay. This can be a positive attribute when it is used as a method of medical treatment or negative when it is harnessed into a weapon (NRC, 2021).
TYPES OF IONIZING RADIATION
There are several types of ionizing radiation, including:
- Alpha particles come from the decay of the heaviest radioactive elements, such as uranium. Due to their weight, they use up their energy over short distances. Exposure to alpha particles outside of the body is not a big concern since the particles cannot penetrate the outer layer of skin. However, they can be harmful inside the body and can be inhaled, swallowed, or enter the body via a cut.
- Beta particles are small negative electric charges emitted by certain unstable atoms. They penetrate the skin more easily than alpha particles but are less damaging to living tissue.
- Gamma rays are weightless packets of energy (photons). Gamma rays are pure energy and are often emitted with alpha or beta particles during the process of radioactive decay
(EPA, 2024)
MEASURING RADIATION
Because radiation cannot be detected by human senses, a device must be used to confirm or exclude its presence. In the case of a radiation terrorism incident, two general types of devices will be used, one to survey victims or healthcare workers and the other to monitor healthcare workers’ cumulative exposure.
Radiation Survey Meters
Colloquially known as Geiger counters, radiation survey meters identify the presence of radiation in the physical environment or on the surface of or within victims. Geiger counters can detect the presence of radiation but cannot determine the original source of the radiation, what type it is, or how much energy it contains. They are used during triage and decontamination of victims.

Geiger counter. (Source: Creative Commons Zero, Public Domain.)
Personal Dosimeters
A personal dosimeter detects and measures radiation that an individual has been exposed to. These devices detect high-energy beta, gamma, or X-ray radiation and are required for workers who operate X-ray machines, fluoroscopy units, and those working with radioisotopes or who are exposed to other sources of radiation. Passive dosimeters absorb radiation over time and are analyzed later in a lab to determine the level of radiation exposure, whereas active dosimeters provide real-time measurements.
Whole-body dosimeters are badges or pocket devices that can be worn anywhere on the body, including the head and neck. Whole-body dosimeters are used in a wide range of occupational environments, including in research, in healthcare, and by emergency response providers.
Electronic personal dosimeters (EPDs) detect and monitor exposure to X-ray, beta, and gamma radiation in real time. They are used for people who need real-time personal dose management such as nuclear medicine technologists and other high-risk workers.
Extremity dosimeters come in ring, wrist, and ankle models to measure exposure in those individuals who are at risk for extremity exposure. These may include researchers using radioactive materials, individuals who use X-ray machines, individuals who work with radiopharmaceuticals, and individuals who may be required to hold patients during X-ray procedures (Government of Canada, 2024).

Passive dosimeters: Optically stimulated luminescence (OSL) body dosimeter (left), thermoluminescent finger dosimeter (TLD) (right). (Sources: OSHA and U.S. DHS.)
Health Effects of Radiation
Exposure to radiation can cause two kinds of health effects:
- Deterministic effects are observable and can occur soon after receiving a large dose. These may include hair loss, skin burns, nausea, or death.
- Stochastic effects are long-term, such as cancer.
The radiation dose determines the severity of a deterministic effect and the probability of a stochastic effect. The goal of radiation control is to prevent any deterministic effects and minimize the risk for stochastic effects (CDC, n.d.-c).
TYPES OF RADIATION EXPOSURE
Radioactive contamination occurs when radioactive material is deposited on or in an object or a person. Radioactive materials released into the environment can cause air, water, surfaces, soil, plants, buildings, people, or animals to become contaminated. A person exposed to radiation is not necessarily contaminated. For a person to be contaminated, radioactive material must be on or inside the body.
There are four different types of injury that can be induced by radiation—irradiation, external and internal contamination, and incorporation of radioactive material.
- Irradiation or radiation exposure occurs when all or part of an individual’s body is exposed to penetrating radiation. An example of irradiation is the process involved with an ordinary chest X-ray. Following irradiation, the individual is not radioactive and cannot spread radioactive contamination.
- External contamination involves contamination with radioactive material, which can be in the form of dust, powder, or liquid, to the skin, hair, or clothing. External contamination requires removal of contaminated clothing and washing the material off.
- Internal contamination occurs when a person swallows or breathes in radioactive materials or when radioactive materials enter the body through an open wound or by absorption through the skin. Some types of radioactive materials stay in the body and are deposited in different body organs, while other types are eliminated through blood, sweat, urine, and feces. Once the material has been eliminated from the body, the individual does not pose a risk to others.
- The fourth type of radiation injury involves incorporation or uptake of radioactive materials by body cells, tissues, and target organs such as bone, liver, thyroid, or kidney. Radiation materials are distributed throughout the body based upon their chemical properties.
(ORI, n.d.)
RADIATION ILLNESS
Once a person has been exposed to radiation beyond a therapeutic dose, radiation-induced illness may occur. Two major categories have been identified: acute radiation syndrome and cutaneous radiation syndrome.
Acute Radiation Syndrome (ARS)
Acute radiation syndrome is caused by total or near-total body irradiation by a high dose of external, penetrating radiation over a very short period of time (minutes). Onset and severity of symptoms are related to the severity of exposure. Victims in close proximity to the detonation of either a nuclear device or a “dirty bomb” would receive the intense exposure that causes ARS. The major cause of this syndrome is depletion of immature parenchymal stem cells in specific tissues (CDC, n.d.-c.).
There are three classic acute radiation syndromes:
- Hematopoietic syndrome (bone marrow syndrome): Lymphocytes die from radiation-caused apoptosis, and precursor cells in the bone marrow are destroyed. This prevents production of leukocytes and platelets; gradually, circulating cells die and are not replaced. The syndrome progresses to infections and possible hemorrhage.
- Gastrointestinal syndrome: Irradiation causes mucosal stem cell death in the intestinal glands (colonic crypts), and new cells cannot be produced. This results in denudation of the gastrointestinal tract and the spread of bacteria. Death usually occurs in 3 to 10 days.
- Cardiovascular/central nervous system syndrome: Irradiation causes vascular damage resulting in significant cerebral edema and circulatory collapse. The patient develops nausea, vomiting, ataxia, hypotension, tachycardia, convulsions, and coma. No recovery is expected, and death usually occurs within 3 days of exposure.
(Williams et al., 2023; CDC, n.d.-c.)
Each of these syndromes go through four stages, as described in the table below.
| Stage | Characteristics |
|---|---|
| (CDC, n.d.-c) | |
| 1. Prodromal (early) |
|
| 2. Latent |
|
| 3. Manifest illness |
|
| 4. Recovery or death |
|
Acute Radiation Syndrome Treatment
Treatment for persons with internal exposure:
- Initial treatment includes lavage with fluids and charcoal to minimize absorption of radioactive materials.
- Radioactive iodine can be used with saturated solution of potassium iodide within a few hours to decrease the uptake of radionuclide in the thyroid. This may decrease the risk of malignancies in the future.
- Penicillamine is a chelating agent that binds to specific radioactive metals and results in decreased tissue uptake and increased excretion.
- Cesium exposure can be treated with ferric hexacyanoferrate, which will decrease gastrointestinal absorption.
- Treatment of exposure to americium, curium, and plutonium can include pentetate calcium trisodium (Ca-DTPA) and pentetate zinc trisodium (Zn-DTPA) injection.
Treatment for individuals with large-dose radiation exposure includes:
- Fluids and electrolytes are administered for managing nausea, vomiting, and diarrhea.
- Depending on the dose of radiation, antibiotics, cytokines, transfusions, and platelet transfusion should be considered.
- If absolute neutrophil count is <500 cells/mm, prophylactic antibiotics and antiviral, antifungal, and antipseudomonal coverage are considered.
- Filgrastim may be considered for treatment of hematopoietic syndrome.
(Williams et al., 2023; CDC, n.d.-c)
Cutaneous Radiation Syndrome (CRS)
CRS can occur without symptoms of ARS. This is especially true with acute exposures to beta radiation or low-energy X-rays, because these are less penetrating and less likely to damage internal organs than gamma radiation. Most cases of radiation-caused skin injury have occurred when people inadvertently came in contact with unsecured radiation sources. In addition, cases of CRS have occurred in people who receive radiation therapy for cancer.
Exposure to radiation can damage the basal cell layer of the skin. Early signs and symptoms of CRS inflammation include itching, tingling, and dry or moist desquamation. In addition, radiation damage to hair follicles can cause epilation.
Transient and inconsistent erythema (associated with itching) can occur within a few hours of exposure and be followed by a latent, symptom-free phase lasting from a few days to several weeks. After the latent phase, intense reddening, blistering, and ulceration of the irradiated site are visible. Depending on the radiation dose, a third and even fourth wave of erythema are possible over the ensuing months or possibly years.
In most cases, healing occurs by regenerative means; however, large radiation doses to the skin can cause permanent hair loss, damaged sebaceous and sweat glands, atrophy, fibrosis, decreased or increased skin pigmentation, and ulceration or necrosis of exposed tissue.
Cutaneous radiation burns should be treated similarly to thermal burns. Severe burns may require amputation, grafts, or vasodilator therapy (CDC, n.d.-c).
Management of Response to a Nuclear/Radiation Terror Attack
The initial care team should include staff with expertise in radiation safety as well as trauma-related injuries. The facility disaster plan should contain information on how to contact individuals with this type of experience. For facility staff, an up-to-date alert roster should be readily available. If this expertise is not available in-house, a consultative relationship with a larger institution may be obtained. This should be included in the disaster plan.
In the absence of either of these options, or to augment them, the Radiation Emergency Assistance Center is available 24/7/365 (see “Resources” at the end of the course). This agency’s functions include deploying to and providing emergency medical consultation for incidents involving radiation anywhere in the world (CDC, 2024a).
HOSPITAL TRIAGE
An ad hoc triage area should be established on location based upon a preestablished disaster plan and anticipated number of casualties, with a contaminated area and clean area separated by a buffer zone. Whenever possible, all triage participants should be volunteers. Healthcare providers should work in teams and a radiation safety officer should monitor them for exposure with dosimetry.
When a facility is expecting only one or two patients with possible radiologic contamination, triage can be done in the ambulance or ambulance bay. Moving triage outside of the facility during a mass casualty incident helps to prevent large numbers of patients from presenting directly to the ED.
The triage area should allow for rapid setup and have adequate staffing, supplies, and radiation monitoring capability to sort patients by medical severity. “DIME” is the standard NATO nomenclature recommended for triage:
- Delayed: May be life-threatening, but intervention can be delayed
- Immediate: Immediate attention required to prevent death
- Minimal: Ambulatory, minor injuries, can wait for definitive attention
- Expectant: Survival unlikely
Those patients with immediate life-threatening injuries should be brought directly to the emergency department prior to radiologic survey and decontamination. For stable patients with serious illness or injury, radiologic decontamination should be done prior to the patient being taken into the clean area of the emergency department.
Whenever possible, patients who are stable but contaminated with urgent injuries should enter the facility through a separate entrance and be taken to a designated decontamination room separate from the rest of the ED. If a separate entrance is not available, the areas where contaminated patients walk should be taped off and labeled as radioactive (CDC, 2024a; Wingard & Dainiak, 2023).
STAFF PROTECTION GUIDELINES
Basic protective actions involve three factors: time, distance, and shielding. Radiation doses should be kept to a level that is as low as reasonably achievable. This is accomplished by:
- Minimizing time spent in the area of radiation; planning emergency response missions efficiently so that first responders enter and leave areas where they may be exposed or become contaminated as few times as possible and spend as little time as possible in the area
- Maximizing the distance between worker and source of radiation exposure; performing only lifesaving and other critical tasks near a dangerous radiation source
- Using proper hazard controls, including shielding workers from a radiation source and contamination and the use of personal protective equipment
- Reassigning pregnant workers to job duties that minimize radiation exposure
- Conducting hazard assessment for workers and monitoring workers’ radiation doses
- Establishing an on-scene decontamination facility
(OSHA, n.d.-b)
PERSONAL PROTECTIVE EQUIPMENT
In a radiation emergency, choice of personal protective equipment depends on the response role, specific tasks, and risk of contamination. It is important to be aware that there is no practical personal protective equipment that can protect responders from high-energy, highly penetrating forms of ionizing gamma radiation associated with most radiation emergencies.
Emergency responders arriving at a radiation emergency scene may not know they are being exposed to radiation unless they utilize a radiation detecting device. Monitoring devices are the only means to make certain that responders do not enter an area where exposure is excessive.
Level B PPE is used by first responders to prevent skin contamination by alpha and beta particles. Typical firefighter gear is considered adequate. Protection of internal organs from radioactive materials may be provided by wearing an appropriate particulate respirator. Protection against internal organ contamination can be provided by wearing an appropriate particulate respirator. SCBAs provide a high level of protections. Responders should use a full-face air-purifying respirator with a P-100 or HEPA filter.
Level C PPE is recommended for first receivers who are caring for victims highly suspected to be contaminated with radiologic material. This includes a hooded, NIOSH-certified powered air-purifying respirator including appropriate breathing filters. A non-powered air-purifying respiratory may be worn when data confirm that a negative-pressure respirator will adequately protect users from identified inhalation hazards.
Several types of PPE for personnel providing care for radiologically contaminated patients consists of modified Universal Precautions. Typically, these include:
- Shoe covers
- Zip-up coveralls (waterproof)
- Surgical cap
- Respiratory masks
- Face shield
- Inner pair of gloves
- Outer pair of gloves (different color than inner pair)
- Tape to secure outer coverings at junction of first pair of gloves with sleeves and shoe covers with coverall pants legs
- Personal radiation dosimeter worn so that a worker can easily see the readout and/or hear warning alarms
(REMM, 2024; Williams et al., 2023; Wingard & Dainiak, 2023)
Decontamination
Unless they have undergone a radiologic survey and decontamination prior to arrival at the receiving hospital, all patients are presumed to be contaminated. The patient is surveyed with a Geiger-Mueller probe for external contamination as well as for fragments of radioactive shrapnel embedded in wounds. Radioactive fragments are promptly removed with forceps and sealed in lead containers. Findings are documented on an anatomic chart.
PERFORMING A SURVEY FOR RADIATION CONTAMINATION
In the event of suspected radiation contamination, healthcare personnel use a radiation survey monitor to survey patients.
Prior to beginning the survey:
- Inspect the equipment.
- Perform a battery check.
- Conduct a source/operational check.
- Conduct a background reading.
When performing the survey:
- Start at the head on the front side of the body.
- Continue systematically over the body, including the feet and soles.
- Repeat on the back side of the body.
(REMM, 2024)
Decontamination includes removal of clothing and washing. This process is capable of removing 90%–95% of external contamination.
- Remove patient clothing carefully to avoid spread of contamination. Double-bag clothing per radioactive hazardous waste guidelines, label, and save as evidence.
- Cleanse contaminated area. Wash first with saline. If there is facial contamination, flush eyes, nose, and ears with saline and rinse the mouth.
- Cleanse skin with soap and water, beginning with the areas of highest contamination.
- Resurvey and note radiation levels.
- Repeat washing until survey indicates radiation level is no more than 2–3 times the background level or the level remains unchanged.
- Cover wounds with waterproof dressing.
- Dispose of waste water through normal channels.
(Wingard & Dainiak, 2023)
ADDRESSING INTERNAL CONTAMINATION
Internal contamination is considered if high survey readings persist following decontamination.
Nose or mouth contamination may indicate inhalation or ingestion. The patient is scanned and each nostril is swabbed separately to help estimate the level of internal lung contamination. A spot urine sample is also obtained for isotope measurement.
Internal contamination continues until the radioactive material decays, is flushed from the body by natural processes, or is removed by medical countermeasures. Decision to treat will depend on:
- Level of internal contamination
- Size of radiation event
- Availability of resources/personnel
- Likelihood the patient will survive
(REMM, 2024; Wingard & Dainiak, 2023)
CASE
A “dirty bomb” explodes in a crowded casino. Per local emergency response plans, all hospitals in the area are notified to expect the arrival of multiple casualties with both radiation exposure and traumatic injuries. ED staff and others involved in each facility’s emergency response team don appropriate PPE prior to the arrival of the first victims.
Per protocols, treatment is begun immediately for physiologically unstable patients prior to performing the initial survey or beginning initial decontamination. For those without life-threatening injuries, initial radiation surveys are performed. Care providers then remove contaminated clothing from the individuals and place each victim’s clothing and belongings in individual property bags that are then properly labeled. Once all clothing is removed and secured, the secondary survey is performed.
In victims who have been injured by shrapnel from the blast, ED staff remove the shrapnel to protect against possible internal contamination. They clean the wounds, carefully catching any water runoff. They also wash the patients’ bodies with soap and water to remove any external contamination. They then complete a second scan to determine the degree to which the decontamination process was successful.
Psychosocial Aspects of Radiation Terrorism
Major contributing elements to psychosocial stress involved in a nuclear or radiologic incident include the unknown nature of radiation and uncertainty related to the extent of risk for one’s health, the implementation of the protective actions, and the stigmatization of affected people.
Many of the psychosocial aspects of radiation emergencies are similar to those in other emergency situations. However, acute fear, psychological responses to somatic illnesses or injuries, and long-term development of medically unexplained symptoms are particularly likely in radiologic or nuclear emergencies. A range of psychosocial concerns are therefore taken into account when planning for radiation emergencies.
Individuals who may require mental and psychosocial support may include:
- People in close proximity to the radiologic event
- First responders, healthcare personnel, cleanup workers, and other responders working under hazardous or stressful conditions
- Parents and future parents concerned about long-term genetic effects of radiation
- Evacuees and members of hosting communities
- Persons with preexisting mental health and psychosocial needs
- People with low literacy, who may struggle to follow advice and instructions provided by risk communicators
(NEA, 2024; WHO, 2020)
COMMUNICATION
Communication is vital in order to inform people of the health risks they face. Accurate information provided early, often, and in languages that the people understand and through channels people trust enables them to make choices and take actions to protect themselves.
Emergency risk communication is an important aspect of the response to a nuclear incident to help mitigate stressors. This involves the real-time exchange of information, advice, and opinions between experts, community leaders or officials, and the people who are at risk (NEA, 2024; WHO, 2020).
Reporting a Radiation Incident
To report an incident involving nuclear materials, contact the federal government’s centralized reporting center. The U.S. Nuclear Regulatory Commission should be notified of:
- Any accident involving a nuclear reactor, nuclear fuel facility, or radioactive materials
- Lost or damaged radioactive materials
- Any threat, theft, smuggling, vandalism, or terrorist activity involving a nuclear facility or radioactive materials
For guidance in the management of a nuclear emergency, the Radiation Emergency Assistance Center (REAC/TS) should be contacted to record the incident and to receive expert guidance on the medical management of radiation incidents. REAC/TS provides emergency response and subject matter expertise on the medical management of radiation incidents for the National Nuclear Security Administration’s (NNSA) Office of Counterterrorism and Counterproliferation.
(See also “Resources” at the end of this course.)
| Standard/Requirements | Rationale |
|---|---|
| * The hospital considers its prioritized hazards identified as part of its hazard vulnerability assessment when developing the plan. (Source: TJC, 2021.) |
|
| EM.09.01.01: The hospital has a comprehensive emergency management program that utilizes an all-hazards approach. | The critical components to the program include emergency policies and procedures; communication and coordination of response activities; education and training; testing and evaluating exercises; and resources. The structure should be designed to respond to any type of emergency (all-hazards approach) because of the wide array of possible emergencies and the impossibility of predicting all emergencies that could occur at an organization. |
| EM.10.01.01: Hospital leadership provides oversight and support of the emergency management program. | The identification of a qualified emergency management program coordinator is important to ensure that critical components of the program are addressed in the mitigation, preparedness, response, and recovery phases and integrated throughout the organization and within the larger community response network. A multidisciplinary approach makes certain that the emergency management program, the operations plan, policies and procedures, and education and training include the insights across disciplines and departments. |
| EM.11.01.01: The hospital conducts a hazard vulnerability analysis utilizing an all-hazards approach. | Organizations should continually evaluate their known risks and prioritize them to understand their vulnerabilities and prepare to respond to emergencies. |
| EM.12.01.01: The hospital develops an emergency operations plan based on an all-hazards approach.* | The hospital’s all-hazards emergency operations plan (EOP) guides the hospital in responding to and recovering from a variety of emergency or disaster incidents. The EOP identifies what services the hospital will continue to provide in the event of an emergency or disaster incident. An effective EOP also describes how the hospital leaders and staff will do the following:
|
| EM.12.02.01: The hospital has a communications plan that addresses how it will initiate and maintain communications during an emergency.* | The communications plan should account for the rapid evolution of an emergency or disaster and the need to consistently provide clear information regarding the emergency and the hospital’s ability to provide services both internally and externally. |
| EM.12.02.03: The hospital has a staffing plan for managing all staff and volunteers during an emergency or disaster incident.* | Hospitals should anticipate staffing shortages and be prepared to obtain staff from within their health care system, staffing agencies, or those who are federally deployed as part of disaster medical assistance teams. Hospitals should also meet the needs of the health care staff by supporting their emotional and mental health needs during an emergency or disaster. |
| EM.12.02.05: The hospital has a plan for providing patient care and clinical support during an emergency or disaster incident.* | Planning for patient clinical support focuses on equipment and resources that play a direct role in an incident response. The hospital’s emergency operations plan addresses patient care and clinical support activities, including transfer plans, continuity of care, and rapid acquisition of patient care supplies and health care records, especially when evacuation is imminent. |
| EM.12.02.07: The hospital has a plan for safety and security measures to take during an emergency or disaster incident.* | An emergency response plan should include the possible need for heightening security measures; tracking and accountability of patients, staff, and families; and minimizing exposures to hazards. |
| EM.12.02.09: The hospital has a plan for managing resources and assets during an emergency or disaster incident. | The hospital’s plan includes continual assessment on how to obtain, allocate, mobilize, replenish, and conserve its resources and assets during and after an emergency or disaster incident |
| EM.12.02.11: The hospital has a plan for managing essential or critical utilities during an emergency or disaster incident.* | The hospital must be prepared with alternate ways in which it will provide essential or critical systems to maintain functional operations. |
| EM.13.01.01: The hospital has a continuity of operations plan.* | The hospital’s executive leadership identifies and prioritizes those essential services that are deemed necessary to remain operational and makes certain that critical business functions continue working during an emergency or disaster incident. The executive leaders consider costs associated with acceptable and unacceptable levels of risk and prioritize where and when to focus resources, funding, and other assets. |
| EM.14.01.01: The hospital has a disaster recovery plan.* | Disaster recovery strategies focus on how and when the hospital will return to full functionality after an emergency or disaster. This includes proactively developing a disaster recovery plan. |
| EM.15.01.01: The hospital has an emergency management education and training program.* | The program provides disaster-related knowledge and training for its staff, individuals providing services under arrangement, volunteers, physicians, and other licensed practitioners that is consistent with their roles and responsibilities in an emergency. This provides a foundation for those assigned to disaster roles to function efficiently and effectively during an emergency or disaster incident. |
| EM.16.01.01: The hospital plans and conducts exercises to test its emergency operations plan and response procedures.* | Exercises are conducted to test the emergency operations plan through discussion-based or operations-based exercises. These exercises should be comprehensive enough to test the hospital’s emergency plans and response capabilities to failure and incorporate the six critical areas (communications, resources and assets, staffing, patient care activities, utilities, safety and security). |
| EM.17.01.01: The hospital evaluates its emergency management program, emergency operations, and continuity of operations plans.* | Hospitals that evaluate each event or exercise are better prepared for emergencies because they often find unknown risks or failures through these reviews. It is important to then update the emergency management program and emergency operations plan to correct these deficiencies. Improving the plan makes it more effective at sustaining critical operations and protecting lives. |
SURVEILLANCE SYSTEMS
Organized surveillance efforts provide the infrastructure for conveying information to facilitate a timely and appropriate response to a possible covert act of biologicalogic, chemical, or radiation terrorism.
Syndromic Surveillance System
The Syndromic Surveillance System involves the ongoing, systematic collection, analysis, interpretation, and application of real-time indicators for disease, allowing for detection before public health authorities would otherwise identify them.
Syndromic surveillance is an investigational approach in which health department staff, assisted by automated data acquisition and generation of statistical alerts, monitor disease indicators in real time or near-real time to detect outbreaks of disease earlier than would otherwise be possible with conventional reporting of confirmed cases (Kulessa et al., 2021).
The National Syndromic Surveillance Program (NSSP) collects, analyzes, and shares electronic patient encounter data received from emergency departments, urgent and ambulatory care centers, inpatient healthcare settings, and laboratories. The electronic data are integrated through the shared BioSense Platform. Over 6 million electronic health messages are received by the BioSense Platform every day (CDC, 2024b).
In the case of a covert act of terrorism, healthcare providers—including emergency department staff and acute care clinic physicians, nurses, assistive personnel, and infection prevention specialists—play a key role in initiating the response to an act of bioterrorism. These individuals must have the knowledge to identify and initiate a local response to an act of bioterrorism. Their knowledge of what is usual among their patient population will provide the starting point for syndromic surveillance, relying as much on objective knowledge of community trends as on the instinct most professionals develop about what is “normal” for their setting. Clinical features that may be noted include:
- A cluster of persons from a common geographic area with similar symptoms
- A rapid increase in patients presenting with similar signs and symptoms
- An increase in patients who die within 72 hours after hospitalization
- An unusual clinical presentation
- An increased number of dead animals
- Signs and symptoms of biologic warfare agents
- Sudden increases in the use of over-the-counter drug purchases
All of these factors indicate a change in health from the status quo in a community. A clinician with a sense of the community’s general normal health can make a big difference in how soon a response to the threat begins. Clinicians should be aware that if a person admits to no foreign travel in endemic areas of rare viruses, then the suspicion level is high and the local health department or CDC should be contacted (Williams et al., 2023).
BioWatch Program
Established in 2003, the Department of Homeland Security BioWatch Program provides air-monitoring analysis for biological agents likely to be used in a bioterrorism attack, notification procedures, and risk assessment to more than 30 major metropolitan areas across the country.
Currently the DHS is working to upgrade bio-detection technology with the intention of:
- Better addressing a wide range of bioterrorism threats
- Providing real-time data across the Homeland Security organization
- Improving information sharing between federal, state, and local operators
At the same time, the U.S. Department of Defense is evaluating devices to detect clouds of biological warfare agents in the air (CDC, 2024b; WebMD, 2024).
CDC Health Alert Network (HAN)
CDC’s Health Alert Network (HAN) is its primary method of sharing cleared information about urgent public health incidents with public information officers; federal, state, territorial, tribal, and local public health practitioners; clinicians; and public health laboratories. CDC’s HAN also collaborates with federal, state, territorial, tribal, and city/county partners to develop protocols and stakeholder relationships that will ensure a robust interoperable platform for the rapid distribution of public health information (CDC, 2024c).
Individuals can sign up on the CDC website to receive HAN email updates or subscribe to HAN RSS feeds. (See “Resources” at the end of this course.)
HAN MESSAGE TYPES
The CDC (2022) has established several types of alerts categorized by the level of urgency of the information.
- Health Alert: Provides vital, time-sensitive information for a specific incident or situation; warrants immediate action or attention by health officials, laboratorians, clinicians, and members of the public; conveys the highest level of importance
- Health Advisory: Provides important information for a specific incident or situation; contains recommendations or actionable items to be performed by public health officials, laboratorians, and/or clinicians; may not require immediate action
- Health Update: Provides updated information regarding an incident or situation; unlikely to require immediate action
- Info Service: Provides general public health information; unlikely to require immediate action
Nevada Health Alert Network (NVHAN)
The State of Nevada, Division of Public and Behavioral Health (DPBH), Public Health Preparedness Program (PHP) administers the Nevada Health Alert Network (NVHAN). NVHAN is administered via a program called EMI Resource. In addition to delivering NVHAN messages, the EMI Resource is a statewide bed-tracking, availability, and alerting system used in each hospital throughout the state. NVHAN relays important healthcare information received from the CDC and state and local agencies via Technical Bulletins (Juvare, n.d.; NV DPBH, n.d.).
State of Nevada employees, healthcare professionals, first responders/police/fire, or critical infrastructure agencies sign up to receive NVHAN alerts and information. (See “Resources” at the end of this course.)
IF YOU SEE SOMETHING, SAY SOMETHING
The Department of Homeland Security’s campaign “If You See Something, Say Something” offers a comprehensive description of suspicious activities that can be used by any member of the public to recognize and report suspicious terrorist activity. It also provides information on how to report a suspicious activity to local law enforcement or a person of authority. (See also “Resources” below.)
CONCLUSION
Since 9/11, the terrorist threat in the United States has shifted from mostly an external threat to an internal one, and the chances are great that more terrorist attacks will occur. Because of this increased potential of terrorism, extra burdens are placed on healthcare workers. Hospitals and hospital personnel must now be ready to react immediately to such incidents, and they must also implement measures in advance that will protect their own health while providing care to victims.
Terrorism may present in biological, chemical, or nuclear forms, and each has its own unique challenges and medical consequences. In today’s world, it is imperative that healthcare workers be prepared and trained to react effectively to these different types of terrorist attacks.
RESOURCES
Nevada
Nevada Division of Emergency Management / Homeland Security
775-687-0400 (nonemergency)
775-687-0498 (emergency)
Nevada Health Alert Network (NVHAN)
Radiation incidents and emergency response information (NV Division of Public and Behavioral Health)
To report suspicious activity (Nevada Department of Public Safety, Division of Emergency)
844-SEE-SAIT (844-733-7248)
National
Community Emergency Response Team (CERT)
Emergency Preparedness and Response (CDC)
If You See Something, Say Something (U.S. DHS)
Information on specific types of emergencies (CDC)
Radiation Emergency Assistance Center/Training Site (REAC/TS)
865-576-1005 (24-hour emergency hotline)
Radiation Emergency Medical Management (REMM) (U.S. DHHS)
Report a safety concern (U.S. Nuclear Regulatory Commission)
301-816-5100 (24-hour emergency hotline)
800-695-7403 (Nonemergency safety hotline)
Terrorism safety tips (American Red Cross)
REFERENCES
NOTE: Complete URLs for references retrieved from online sources are provided in the PDF of this course.
American Lung Association (ALA). (2023). What are toxic air pollutants? https://www.lung.org
Arms Control Association. (2024). The chemical weapons convention (CWC) at a glance. https://www.armscontrol.org
Britannica. (2024). Terrorism. https://www.britannica.com
Centers for Disease Control and Prevention (CDC). (2024a). CDC’s response to nuclear or radiological emergencies. https://www.cdc.gov
Centers for Disease Control and Prevention (CDC). (2024b). National syndromic surveillance program. https://www.cdc.gov
Centers for Disease Control and Prevention (CDC). (2024c). Health Alert Network (HAN). https://emergency.cdc.gov
Centers for Disease Control and Prevention (CDC). (2022). HAN message types. https://emergency.cdc.gov
Centers for Disease Control and Prevention (CDC). (2020a). Bioterrorism. https://emergency.cdc.gov
Centers for Disease Control and Prevention (CDC). (2020b). Bioterrorism: A brief history. https://www.selectagents.gov
Centers for Disease Control and Prevention (CDC). (2018). Bioterrorism agents/diseases. https://emergency.cdc.gov
Centers for Disease Control and Prevention (CDC). (n.d.-a). Clinical care of anthrax. https://www.cdc.gov
Centers for Disease Control and Prevention (CDC). (n.d.-b). About plague. https://www.cdc.gov
Centers for Disease Control and Prevention (CDC). (n.d.-c). Radiation emergencies. https://www.cdc.gov
DeNolf R & Kahwaji CI. (2022). EMS mass casualty management. StatPearls Publishing. https://www.ncbi.nlm.nih.gov
EMS1. (2023). Mass casualty incidents. https://www.ems1.com
Environmental Protection Agency (EPA). (2024). Radiation basics. https://www.epa.gov
Federal Bureau of Investigation (FBI). (n.d.-a). Terrorism. https://www.fbi.gov
Federal Bureau of Investigation (FBI). (n.d.-b). Amerithrax or anthrax investigation. https://www.fbi.gov
Federal Emergency Management Agency (FEMA). (2023). Nevada: Grant effectiveness case study: Las Vegas. https://www.fema.gov
Federal Emergency Management Agency (FEMA). (2019). CERT basic training: Unit 8. https://www.ready.gov
Government of Canada. (2024). National dosimetry service (NDS) products. https://www.ca
Hayoun M & King K. (2024). Biologic warfare agent toxicity. StatPearls Publishing. https://www.ncbi.nlm.nih.gov
Joint Counterterrorism Assessment Team (JCAT). (n.d.). Counterterrorism guide. https://www.dni.gov
Journal of Emergency Medical Services (JEMS). (2024). Mass casualty incidents. https://www.jems.com
Juling D. (2023). Future bioterror and biowarfare threats for NATO’s armed forces until 2030. Journal of Advanced Military Studies, 14(1), 118–43. https://doi.org/10.21140/mcuj.20231401005
Juvare. (n.d.). EMResource. https://www.juvare.com
Kulessa M, Mencia E, & Fürnkranz J. (2021). A unifying framework and comparative evaluation of statistical and machine learning approaches to non-specific syndromic surveillance. Computers 10, 32. https://doi.org/10.3390/computers10030032
Lung D. (2024). Caustic ingestions. https://emedicine.medscape.com
Madsen J. (2024). Chemical terrorism: Rapid recognition and initial medical management. UpToDate. https://www.uptodate.com
Mauroni A. (2021). Addressing biological threats in the DPD CB Defense Program. http://www.airuniversity.af.edu
Mayo Clinic. (2023a). Anthrax. https://www.mayoclinic.org
Mayo Clinic (2022). Smallpox. https://www.mayoclinic.org
Merriam-Webster. (2024). First responder. https://www.merriam-webster.com
Minnaganti V. (2024). Plague. Medscape. https://emedicine.medscape.com
Nevada Division of Public and Behavioral Health (NV DPBH). (n.d.). Nevada health alert network (NVHAN). https://dpbh.nv.gov
Nuclear Emergency Agency (NEA). (2024). Practical guidance for mental health and psychosocial support in radiological and nuclear emergencies. https://www.oecd-nea.org
Oak Ridge Institute for Science and Education (ORISE). (n.d.). Types of radiation exposure. https://orise.orau.gov
Occupational Safety and Health Administration (OSHA). (n.d.-a). Anthrax. https://www.osha.gov
Occupational Safety and Health Administration (OSHA). (n.d.-b). Radiation emergency preparedness and response. https://www.osha.gov
Radiation Emergency Medical Management (REMM). (2024). Personal protective equipment (PPE) in a radiation emergency. https://remm.hhs.gov
Rathish B, Pillay R, Wilson A & Pillay V. (2023). Comprehensive review of bioterrorism. StatPearls Publishing. https://www.ncbi.nlm.nih.gov
Ray M. (2022). Boston marathon bombing of 2013. Britannica. https://www.britannica.com
Shertz J. (2024). What is a “first receiver”? https://www.crisis-medicine.com
Simonsen KA & Snowden J. (2023). Smallpox. https://www.ncbi.nlm.nih.gov
Stoppler MC & Shiel WD. (n.d.) Ricin poison symptoms. https://www.medicinenet.com
The Joint Commission (TJC). (2021). R3 Report: Requirement, rationale, reference. https://www.jointcommission.org
UF/IFAS Extension. (2024). Preventing foodborne illness: Clostridium botulinum. https://edis.ifas.ufl.edu
United Nations (UN). (n.d.). Chemical, biological, radiological, and nuclear terrorism. https://www.un.org
United Nations Office of Counter-Terrorism (OCT). (2022). Protecting vulnerable targets from terrorist attacks. https://www.un.org
U.S. Army Cyber Command. (2022). Antiterrorism awareness. https://www.arcyber.army.mil/Resources/Fact-Sheets/Article/2057258/
U.S. Department of Defense (U.S. DOD). (2021). DOD dictionary of military and associated terms. https://www.jcs.mil/Portals/36/Documents/Doctrine/pubs/dictionary.pdf
U.S. Department of Health and Human Services (U.S. DHHS). (2024a). Personal protective equipment (PPE) classification systems. https://www.remm.nlm.gov
U.S. Department of Health and Human Services (U.S. DHHS). (2024b). PPE image gallery. https://remm.hhs.gov
U.S. Department of Homeland Security (U.S. DHS). (2022). Biological attack fact sheet: Human pathogens, biotoxins, and agricultural threats. https://www.dhs.gov
U.S. Nuclear Regulatory Commission (NRC). (2021). Ionizing radiation. https://www.nrc.gov
Velez-Daubon L, Caneva D, & Keyes D. (2021). CBRNE—Nerve agents, binary—GB2, VX2. Medscape. https://emedicine.medscape.com
WebMD. (2024). Biological and chemical weapons. https://www.webmd.com
Williams M, Armstrong L, & Sizemore D. (2023). Biological, chemical, and radiation terrorism review. StatPearls Publishing. https://www.ncbi.nlm.nih.gov
Wingard JK & Dainiak N. (2023). Management of radiation injury. UpToDate. https://www.uptodate.com
Wisconsin Project on Nuclear Arms Control (WPNAC). (n.d.). Chemical weapons primer. https://www.wisconsinproject.org
World Health Organization (WHO). (2022). Plague. https://www.who.int/news-room/fact-sheets/detail/plague
World Health Organization (WHO). (2020). A framework for mental health and psychosocial support in radiological and nuclear emergencies. https://www.who.int/publications/i/item/9789240015456
Zhang X & Wang J. (2022). Atmospheric dispersion of chemical, biological, and radiological hazardous pollutants: Informing risk assessment for public safety. Journal of Safety Science and Resilience, 3(4), 372–97. https://doi.org/10.1016/j.jnlssr.2022.09.001






Customer Rating
4.9 / 625 ratings