Ostomy Care
Colostomy, Ileostomy, Urostomy
Online Continuing Education Course

Course Description
Enhance your knowledge and clinical competence in ostomy care. Focusing on colostomy, ileostomy, and urostomy, this continuing education course provides essential insights into the comprehensive care and support required for patients with ostomies across all stages of treatment and recovery. Learn to identify the different types of ostomies, understand the principles of perioperative care, and implement effective home care strategies. The course also covers common ostomy-related complications, their prevention and management, and equips clinicians with the tools to support patients in adapting to life with an ostomy. By addressing key knowledge gaps, this course empowers healthcare professionals to deliver more confident, compassionate, and informed care. Applicable for nursing, occupational therapy, and physical therapy.
Ostomy Care
Colostomy, Ileostomy, Urostomy
Copyright © 2025 Wild Iris Medical Education, Inc. All Rights Reserved.
LEARNING OUTCOME AND OBJECTIVES: Upon completion of this course, you will have increased your understanding of the care and support of patients who have ostomies. Specific learning objectives to address potential knowledge gaps include:
- Identify the types of ostomies.
- Discuss perioperative care for patients undergoing ostomy surgery.
- Summarize the elements of effective home care for ostomies.
- Describe potential ostomy complications and their treatment.
- Outline strategies to adapt successfully to living with an ostomy.
TABLE OF CONTENTS
INTRODUCTION
Caring for and understanding the needs of a patient with an ostomy is a critical area of healthcare. To be successful, ostomy care requires the input of skilled and knowledgeable clinicians.
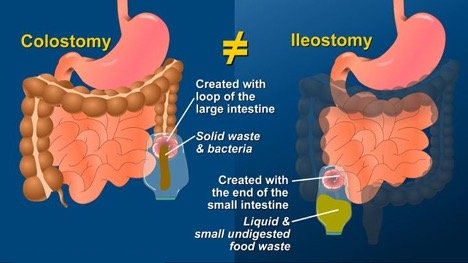
An ostomy is a surgically created opening into the abdominal cavity that allows for the connection of an internal organ, such as the colon (colostomy), ileum (ileostomy), or ureters (urostomy), to the skin level to provide a diversion for elimination of stool or urine. The opening of the ostomy at the skin level is referred to as a stoma, which is derived from a Greek word that means “opening” or “mouth” (Cowell et al., 2019; UOAA, 2024a).
An ostomy, regardless of the type, is an incontinent diversion and requires wearing a pouching system on the abdominal surface. However, a continent diversion, which can be either bowel or bladder, creates a reservoir for waste within the patient’s body and in some instances requires catheterization for emptying (UOAA, n.d.-a).

Colostomy stoma on the abdomen. (Source: Reprinted courtesy of Hollister Incorporated, Libertyville, Illinois.)

Colostomy stoma with pouch. (Source: Reprinted courtesy of Hollister Incorporated, Libertyville, Illinois.)
Currently, over 750,000 individuals in the United States have ostomies, and around 130,000 individuals have a new ostomy created annually (AGA, 2023). The average age of a person with an ostomy is slightly over 68 years. However, the need for ostomy creation occurs over the continuum of life. Fecal and urinary diversions are also created in the pediatric population. For instance, over half of all stomas are surgically created in the neonatal phase and a further one quarter in newborns under 1 year of age (WOCN, 2022).
TYPES OF OSTOMIES
There are several different types of ostomies and continent diversions. The type of ostomy created is highly individualized and depends on several factors, including the condition and circumstances that warrant the creation of the ostomy. The most common types of ostomy surgery include colostomy, ileostomy, and urostomy. An ostomy can either be temporary or permanent.
(Source: Kennan Motley. CC Share Alike 2.0 Generic.)
Colostomy
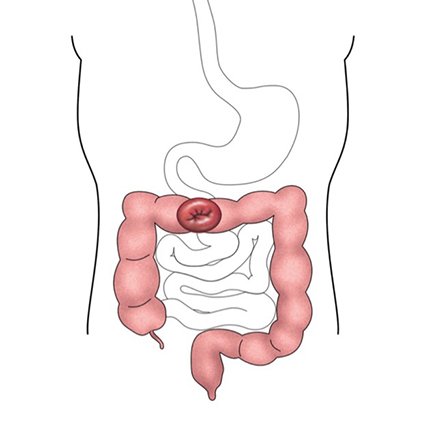
Colostomy is an opening into the large intestine. After a diseased or damaged part of the intestine is surgically removed, the healthy end of the remaining portion of the large intestine is brought through the abdominal wall to form the stoma opening on the exterior surface of the abdomen (ACS, 2019a; UOAA, n.d.-c). Colostomy is the most frequently performed ostomy surgery worldwide.
Despite the advances in minimally invasive surgery (MIS), which include laparoscopy and robotic surgery, open surgery continues to be a common intervention for colectomies, notably in high-risk populations, such as those requiring emergency surgeries. This is due in part to the prohibitive costs and specialized training requirements associated with robotic surgery (Laredo et al., 2025).
A permanent colostomy is created to provide for the elimination of waste when a portion of the large intestine must be surgically removed due to disease or can no longer function or when the anal sphincter process must be resected. The type of ostomy created when a permanent colostomy is required is usually an end or sigmoid colostomy.
A temporary colostomy is created when a distal portion of the large intestine must be kept free from stool. This may be due either to an obstructive mass in the distal colon or to allow for the healing of a distal anastomosis (the surgical reconnection of the two ends of the intestine) (WOCN, 2022).
A colostomy can be created at almost any area along the large intestine. Colostomies are further divided into several types, which are described below.
ANAL SPHINCTER PROCESS
The anal sphincter process plays an essential role in maintaining continence. The anal canal, which is only 3–4 cm in length, is equipped with two sphincters: the internal anal sphincter and the external anal sphincter. The internal anal sphincter is an involuntary smooth muscle that prevents gas and stool from being expelled unexpectedly. The external anal sphincter is under voluntary control.
The muscles of the colon contract and move stool to the rectum in a process known as peristalsis. The influx of stool causes stretching of the rectum and results in the activation of the defecation reflex. The defecation reflex happens when the internal anal sphincter relaxes and the external anal sphincter contracts. At this stage, the individual decides if it is appropriate to defecate or not.
When the anal sphincter process must be surgically removed due to disease, continence and voluntary defecation is lost. When a patient is diagnosed with a low rectal malignant tumor, the primary surgical treatment is an abdominoperineal resection, which removes the distal colon, the rectum, and the anal sphincter process and results in the creation of a permanent colostomy (WOCN, 2022; Wei et al., 2024).
ASCENDING COLOSTOMY
An ascending colostomy is performed on the ascending portion of the large intestine, and the stoma is placed on the right side of the abdomen. This is a relatively rare ostomy, and the surgical preference is usually to create an ileostomy rather than an ascending colostomy (Johns Hopkins, 2024).
TRANSVERSE COLOSTOMY
A transverse colostomy is created in the middle (or transverse) section of the large intestine. The stoma from a transverse colostomy is situated on the upper abdomen. The location may be in the upper right or left quadrants or mid-abdomen, depending on the area of the transverse colon where the stoma is constructed.
Surgical creation of a transverse colostomy can be further divided into two types:
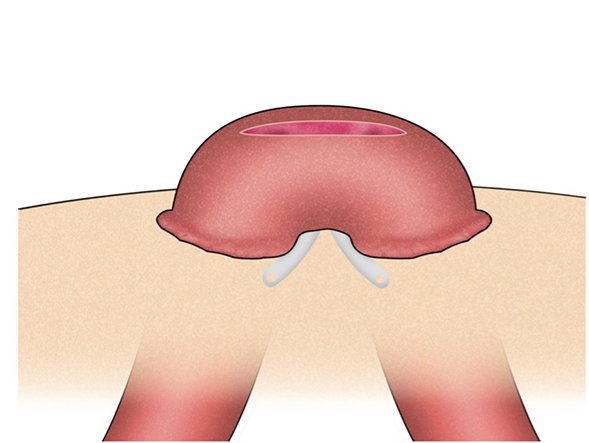
- Loop transverse colostomy: In this surgery, a loop of the bowel is pulled through the abdominal wall and secured in place with an external device. The loop transverse colostomy has two openings in a single stoma, one to evacuate stool and the other to expel mucus only.
- Double-barrel transverse colostomy: In this surgery, the large intestine is divided into two separate openings, and each is a separate stoma. The first is to evacuate stool and the other to expel mucus. The latter is usually a smaller stoma and referred to as a mucus fistula.
(ACS, 2019a)
Transverse colostomies are frequently a temporary procedure and reversed at a later stage (Johns Hopkins, 2024).
Transverse colostomy. (Source: Reprinted courtesy of Hollister Incorporated, Libertyville, Illinois.)
Loop stoma. (Source: Reprinted courtesy of Hollister Incorporated, Libertyville, Illinois.)
DESCENDING COLOSTOMY
The site for a descending colostomy is the descending part of the large intestine, with the stoma placement on the left side of the abdomen. However, in some patients, due to body shape, stoma placement is in the left upper quadrant (WOCN, 2022). The rectum or anus may be removed during surgery or simply disconnected and left in place (Johns Hopkins, 2024).
END OR SIGMOID COLOSTOMY
When a sigmoid colostomy is created, the last part of the colon is removed. Stoma placement is normally in the left lower part of the abdomen. Similar to descending colostomy, the rectum and anus may be surgically removed or disconnected and left in place (St. Luke’s Health System, n.d.).
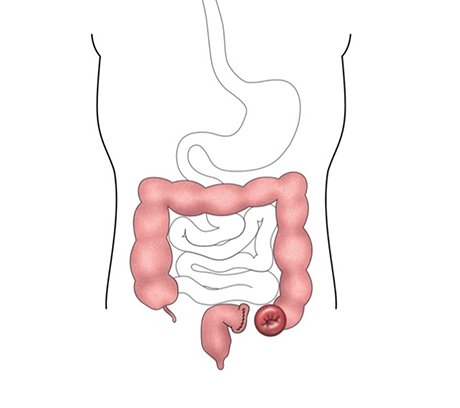
End or sigmoid colostomy. (Source: Reprinted courtesy of Hollister Incorporated, Libertyville, Illinois.)
End stoma. (Source: Reprinted courtesy of Hollister Incorporated, Libertyville, Illinois.)
CONDITIONS LEADING TO COLOSTOMY CREATION
The most common patient conditions that lead to the creation of a colostomy are:
- Colorectal cancer
- Diverticulitis
- Bowel obstruction
- Volvulus
- Injury
CURRENT PRACTICES IN OSTOMY SURGERY
There has been a significant decline in the number of permanent colostomy surgeries done; while at the same time, there has been a significant increase in the number of temporary ileostomy surgeries. The decrease in the number of permanent colostomy surgeries is attributed to the advances in colorectal cancer surgeries, specifically the increase in sphincter-sparing surgeries for malignancies located distally in the anorectal area. These surgeries allow for the removal of the cancerous tumor while maintaining continuity to the anus. In these instances, a temporary ileostomy is performed.
Ileostomy
Ileostomy is a surgically created opening into the small intestine. The most common site for an ileostomy is the distal section of the ileum, usually sited in the right lower quadrant of the abdomen. The ileum is brought through the surgically created abdominal opening and secured in place at skin level. An ileostomy maybe permanent or temporary and is often associated with removal of a section of the colon or the entire colon.
An ileostomy has a smaller diameter compared to a colostomy. This is due to the fact that the lumen of the small intestine is smaller than that of the large intestine (WOCN, 2022).
A temporary ileostomy is created to allow healing time to a surgical site in a distal part of the intestines. Surgical procedures that may require a temporary ileostomy include:
- Colorectal surgery for cancer removal
- Diverticulitis surgery
- J-pouch construction for conditions such as ulcerative colitis or familial polyposis (discussed below)
Permanent ileostomies are created when the large intestine is surgically removed and reconnecting the intestinal tract to the anus is not possible. The most frequent type of permanent ileostomy is known as the standard, or Brooke, ileostomy. During construction, the end of the ileum is brought out through the wall of the abdomen and then folded back and sutured to the patient’s skin, creating a round, even stoma. The Brooke ileostomy stoma is normally sited in the right lower quadrant of the abdominal wall. The output from the stoma is not regulated, and the patient is required to wear an ostomy pouching system (Lucchetti, 2024).
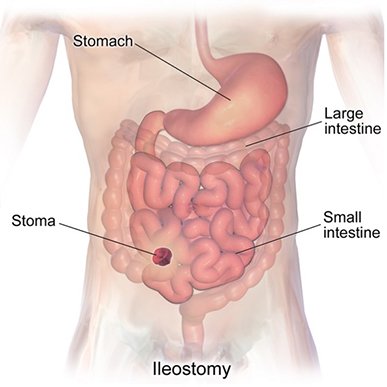
Ileostomy. (Source: BruceBlaus. CC Share Alike 4.0.)
CONTINENT ILEOSTOMIES
With a standard ileostomy there is frequent flow of effluent, whereas with a continent ileostomy, the effluent is contained with an internal (abdominal) pouch until the patient empties it. The advantages of a continent ileostomy are greater patient control over waste elimination, no external collection pouch, and improved quality of life (Mayo Clinic, 2022).
The J-pouch is now the most frequently used type. The creation of a J-pouch involves the surgical removal of the colon and most of the rectum. The distal part of the ileum is used to create a pouch. An opening is placed at the posterior end of the pouch, and this opening is attached to the anus, permitting the existing anal sphincter muscles to maintain continence. A temporary ileostomy is also created to allow for evacuation of fecal waste while the J-pouch anastomosis is allowed to heal. The temporary ileostomy will be reversed after approximately three months (Mayo Clinic, 2024a).
The Kock pouch is a high-volume, low-pressure internal reservoir in the abdominal cavity created using the terminal ileum in a double-folding technique, with the end of the small intestine opening into a buttonhole-size stoma on the surface of the abdomen. Currently, the creation of a Kock pouch is not done as often as in the past, but it is still regarded as an option for patients who are not candidates for other types of procedures (WOCN, 2022).
The Barnett continent intestinal reservoir (BCIR) is a variation on the Kock pouch. The goal of the BCIR is to decrease valve slippage and incidence of incontinence. A collar is created by wrapping a section of the small intestine around the top of the pouch and valve. In a BCIR, while the pouch is filling, the collar around the opening of the pouch is also filling, resulting in tightening that prevents the valve from slipping out of place (WOCN, 2022).
CONDITIONS LEADING TO ILEOSTOMY CREATION
An ileostomy may be required in the following conditions:
- Inflammatory bowel disease
- Ulcerative colitis
- Polyposis syndromes
- Post cancer surgery
Urinary Diversions
A urostomy is a surgically created opening into the abdominal wall for the elimination of urine after the bladder is removed. The goal of urinary diversion is to preserve kidney function. Urinary diversions can be divided into continent diversions and incontinent diversions. A continent diversion, such as neobladder construction, offers the advantages of both continence and maintained body image (Sperling et al., 2021).
The most frequently created urostomy is an ileal conduit. Other types of urinary diversions include the Indiana pouch and neobladder construction (WOCN, 2022).
CONDITIONS LEADING TO UROSTOMY CREATION
- Bladder cancer
- Neurogenic bladder disease
- Birth defects
- Chronic inflammation of the bladder
(ACS, 2019b)
ILEAL CONDUIT
Ileal conduit construction is the most frequent type of urinary diversion surgery globally (Haywood & Klein, 2020). Patient selection is important. When maintaining intestine length is of prime importance, an ileal conduit may be the best option. An ileal conduit creation requires about 10–12 cm of intestine, whereas a continent diversion requires the use of 50–60 cm of intestine (WOCN, 2022).
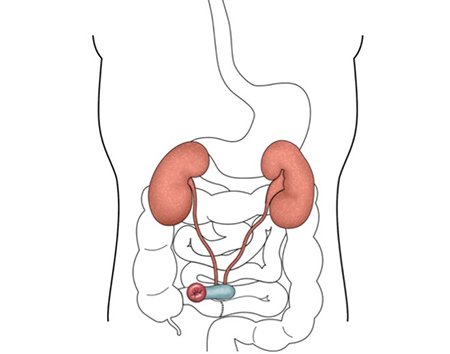
Ileal conduit, showing small piece of bowel used to carry urine. (Source: Reprinted courtesy of Hollister Incorporated, Libertyville, Illinois.)
The ileal conduit is created by joining the ureters to the proximal end of the harvested conduit with stent placement, which assists with healing. The distal end of the conduit is used to create a cutaneous stoma to provide for urine drainage to an external collection mechanism attached to the patient’s skin. The stoma for an ileal conduit has a raised rosebud structure that averts urine from coming into contact with the skin when the pouching system is in place (WOCN, 2022).
An ileal conduit is an appealing option for many patients. It is not time consuming or difficult to care for. Normally, the ostomy pouching mechanism needs to be changed only every three to four days. The downside to ileal conduit creation is the alteration in body image, since urine elimination is diverted to a stoma placed on the surface of the abdomen and the patient must wear a pouch continuously over the stoma to collect urine (WOCN, 2022).
INDIANA POUCH RESERVOIR
The Indiana pouch reservoir (invented at Indiana University) is the primary continent urinary diversion. It is a surgically created reservoir located inside the body. Urine is drained from the Indiana pouch by the process of self-catheterization. Patients with an Indiana pouch must be committed to performing catheterization every four to six hours, and this regime must be strictly adhered to on a daily basis. Patients who opt for an Indiana Pouch must also have the necessary cognitive and physical capacity to perform self-catheterization (IU School of Medicine, 2021).
The Indiana pouch is created from the terminal ileum, ileocecal valve, and right colon. It is imperative that the ileocecal valve is intact. The ileocecal valve is a one-way valve dividing the small intestine from the large intestine, and it functionally inhibits backflow from the large intestine to the small intestine.
During the surgical procedure, the right colon is transformed into a ball-shaped, continent reservoir with the ability to hold up to 600 ml of fluid. The ileocecal valve provides the continence structure, and the terminal ileum is used to create the catheterization conduit (WOCN, 2022; IU School of Medicine, 2021).
The ureters are introduced through the posterior wall of the newly formed reservoir and attached to its eternal surface. The stoma for the Indiana pouch is usually placed on the right lower quadrant of the patient’s abdomen (WOCN, 2022).
NEOBLADDER-TO-URETHRA DIVERSION
A neobladder creation is also referred to as orthotopic urinary diversion. This surgery creates a new, low-pressure, high-volume bladder in the pelvic cavity of the patient. It is surgically attached to the urethra and dependent on the patient’s urinary sphincter mechanism to provide continence (WOCN, 2022).
The neobladder is constructed from a segment of bowel, utilizing from 50–60 cm of the ileum. It can ultimately hold 400–500 ml of urine (Sperling et al., 2021; Smith et al., 2023).
The most important feature of a neobladder creation is that it provides the individual with continence along with intact body image (Janssen et al., 2021).
Ostomies in Neonates and Children
Ostomy creation has been used in the pediatric population since the inception of ostomy surgery. Some of the first survivors of ostomy creation were children who underwent this surgery to treat an imperforate anus. There were, however, significant complications related to surgery as well as high mortality rates.
Over the decades, ostomy surgery in the pediatric population has evolved, with enhanced surgical techniques and better stoma care. A more judicious use of ostomy creation is now the norm. Today, most pediatric ostomies are temporary, which alleviates many of the complications associated with permanent ostomy creation, such as problems with fluid and electrolyte imbalances (Minkes, 2022).
An ileostomy or colostomy may be required in children to manage the conditions listed below. The type of stoma created is decided upon according to the actual condition. Pouching systems can be used with children with ostomies, and pediatric pouching systems are available. However, depending on the age of the child, a diaper may be used to contain stool. This will require close attention to skin care to prevent irritation and breakdown (WOCN, 2022).
CONDITIONS IN NEONATES THAT MAY REQUIRE AN OSTOMY
- Necrotizing enterocolitis (NEC)
- Hirschsprung disease
- Meconium ileus
- Intestinal atresia and stenosis
- Malrotation and intestinal volvulus
- Anorectal malformations
- Trauma
(Minkes, 2022; WOCN, 2022)
Urostomies are rarely performed in children. Vesicostomy is a procedure that is performed to provide a passage for urine while protecting the upper urinary tract system (WOCN, 2022). During a vesicostomy, a small surgical opening is created from the bladder to the external surface of the lower abdomen, distal to the umbilicus, with placement of a stoma. With a vesicostomy procedure, urine is allowed to drain into the child’s diaper, with no need for a drainage bag.
A vesicostomy is performed when a child has difficulty emptying their bladder. It is most often a temporary procedure and is generally closed by the time the child is ready to start toilet training. This procedure may be required for children who have spina bifida. It may also be required if there is spinal cord injury (Cleveland Clinic, 2024b). This surgery can be done soon after the infant is born and left in place until the child reaches school age.
The major concern with a vesicostomy is protecting the peristomal skin and preventing the occurrence of moisture-associated skin damage. Skin protection is best achieved by using liquid skin barriers or petrolatum-based products. If skin irritation occurs because of urine exposure, the area can be treated with diaper rash ointment (WOCN, 2022; Cleveland Clinic, 2024b).
PERIOPERATIVE CARE
Preoperative care has been shown to play a significant role in patient recovery and the development of fewer postoperative complications (WOCN, 2022). Discharge planning and ongoing postoperative care are also essential components in successful outcomes for these patients.
Preoperative Care
Ideally, patients in the preoperative phase should be seen by a wound, ostomy, and continence nurse (WOCN). This also offers an opportunity to develop a relationship and a foundation for later postoperative teaching.
OSTOMY PATIENT BILL OF RIGHTS
The United Ostomy Associations of America has developed both an adult and pediatric ostomy patient “Bill of Rights” to help ensure a positive outcome post surgery. These documents outline evidence-based recommendations for quality care. Some of the preoperative standards in this Bill of Rights include:
- Preoperative stoma site marking
- Explanation of the surgical procedure and the rationale for surgery
- Education on living with an ostomy/continent diversion and self-care post discharge
- Information about the impact of surgery on daily activities (e.g., adapting physically and emotionally and lifestyle changes)
- Opportunity to talk with someone who has been through ostomy or continent diversion surgery
- Opportunity to discuss the emotional impact of surgery
(UOAA, 2021)
Standards in the pediatric Bill of Rights include:
- Collaboration with a child life specialist who can provide details about the upcoming surgery that mirror the child’s developmental stage
- Sibling involvement and education
- Education from an ostomy nurse explaining the impact of surgery on activities of daily living, including physical activity and clothing
- Preoperative stoma site marking
- Education on the type of stoma that will be created during surgery
- Mentorship with a family who has gone through ostomy surgery
- Communication about the psychological and developmental impact of surgery on the child and their family
(UOAA, 2018)
PREOPERATIVE PATIENT EDUCATION
Preoperative education is a crucial component in successful outcomes for patients undergoing ostomy surgery. It helps to alleviate patients’ fears and concerns and gives them an opportunity to ask questions about what to expect in the future.
For many patients, terms such as ileostomy, colostomy, or ileal conduit will be unfamiliar. Prior to surgery, patients’ attention may be completely focused on their primary diagnosis, and for those with malignancies, the only topic on their mind may be cancer. Such patients may not be able to receive education on an ostomy and may even react with dismay and anger post surgery when they realize that they have an ostomy. For other patients, ostomy creation may be part of an emergency surgery during which there is no opportunity for preoperative care and education.
Preoperative education focuses primarily on general knowledge, providing answers to patient and family questions and addressing patient and family concerns. Handouts, pictures, and videos can be used to introduce the patient and family to what an ostomy is and what a stoma will look like. It is important to point out that not all stomas end up looking perfectly round and budded as typically shown in illustrations. Prior to surgery, not all patients know whether they will end up with an ileostomy or a colostomy due to uncertainties about the complexity of the surgery, so education about the type and amount of fecal output must be general (WOCN, 2022).
Patients undergoing a urinary diversion require much of the same preoperative education and preparation as those undergoing a fecal diversion, but there are also some unique considerations. These include a comprehensive evaluation of baseline kidney function, since most patients will experience diminished long-term kidney functioning following the creation of a urinary diversion, which may be related to older age, coexisting health conditions such as diabetes, and hypertension (Sperling et al., 2021).
Preoperative education has been found to decrease postoperative complications, enable a more positive adjustment process, and increase parents’ ability to provide postoperative ostomy care (Uzsen et al., 2021).
STOMA BOOT CAMP
Begun in 2018, the University of Kansas Cancer Center Stoma Boot Camp (SBC) is a preoperative comprehensive stoma education program aimed at patients undergoing urostomy surgery due to bladder cancer, as well as their loved one or caretaker. SBC employs lectures, audiovisual learning, hands-on experience with ostomy supplies, and hearing the experience of a person who is living with a stoma. Topics covered during the session include teaching on ostomy creation, what to expect in the postoperative period, ostomy appliances, and returning to daily life. Evaluation has found the program to yield positive results, including decreased patient and caregiver anxiety and increased efficiency in postsurgical ostomy care, translating into improved quality of life. In 2020, a virtual opportunity was included in the program (Wulff-Burchfield et al., 2021).
STOMA SITE MARKING
A critical component of a preoperative visit is stoma site marking on the patient’s abdomen, indicating the ideal location for stoma placement, especially for patients who will have a permanent ostomy. Preoperative stoma site marking is included in the United Ostomy Associations of America (UOAA) Patient Bill of Rights (see above). The Wound Ostomy and Continence Society also endorses the practice of stoma site marking (WOCN, 2022).
Optimal placement of the stoma has been shown to have a direct impact on patient quality of life and is considered best practice. Preoperative stoma site marking may also improve the interval between pouching system changes, promote patient adaptation to the stoma, ease transition to independent self-care, and reduce healthcare costs and resource utilization.
General principles of optimal stoma site placement call for a flat skin surface with as few creases as possible and easy visibility to the patient so that they can perform stoma care without difficulty. Locating the stoma within the rectus abdominis muscle (“abs”) decreases the risk for a peristomal hernia or a stoma prolapse.
Even though stoma site marking is done by the professional ostomy nurse, all clinicians can explain to the patient the importance of stoma site marking and ensure a referral to the ostomy nurse (WOCN, 2021).
PELVIC FLOOR MUSCLE EXERCISES
Performing pelvic floor muscle (PFM) exercises prior to surgery is beneficial in maintaining continence post surgery. PFM exercises are also continued after the catheter is removed (UOAA, 2019).
Physical therapy (PT) interventions are considered a mainstay in correcting and managing pelvic floor muscle tone. PT treatments may include interventions such as manual therapy, neuromuscular electrical stimulation, biofeedback, and pelvic floor muscle exercises.
Limited research also demonstrates that occupational therapy (OT) treatments may have a positive impact on pelvic floor health. Interventions used by OTs to strengthen pelvic floor muscles include diaphragmatic deep-breathing exercises, developing awareness of pelvic floor muscles, and yoga. However, more research is needed (Schmitz, 2021).
Postoperative Considerations and Care
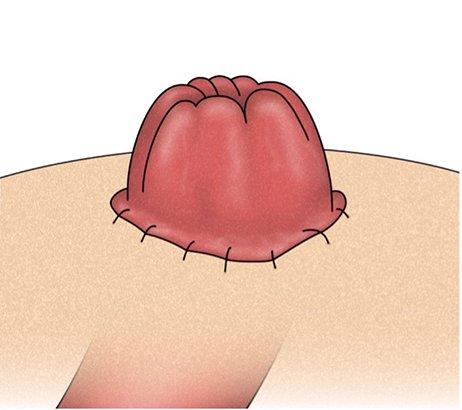
Following surgery, clinicians assess and monitor the condition of the stoma. A healthy, newly created ostomy will be bright red in color, moist and edematous, and with a shiny, taunt appearance. A urostomy stoma may be slightly different in color, typically pink. Stomas that appear darkish red or purple in color or are dry should be reported to the surgeon immediately, as this may be an indication of compromised blood flow.
Ideally, the stoma protrudes a minimum of 2 cm above skin level to facilitate pouching. A stoma that is flush with the abdominal wall or retracted can result in waste leaking under the seal and exposing the peristomal skin to damage once the pouching system is attached (WOCN, 2022). This may require adaptation in the pouching system use (discussed later in this course).
In some cases, the surgeon may have placed a support bridge or rod under the stoma to prevent retraction of the stoma and allow adequate time for it to adhere to the skin surface. A support bridge is sutured to the abdominal skin and usually left in place for five to seven days, as determined by the surgeon. A support bridge must fit within the pouching system. Rigid support bridges have been found to be more challenging in this respect, and there are concerns that they may hinder attachment of the faceplate around the stoma, causing undermining and leaking of feces onto the peristomal area.
URINARY DIVERSION
A urostomy begins to function immediately after creation. Initial output will be blood-tinged urine and mucus. Patients who have an ileal or colon conduit constructed will have stents that are placed at the time of surgery. The function of the stents is to protect the anastomosis joining the ureter with the conduit. Several factors determine the length of time the stents are left in place, including healing time and the surgeon’s preference.
Postoperatively it is recommended to connect the urostomy pouch to a drainage bag while the patient is in bed. The pouch can be disconnected from the drainage bag when the patient is up and ambulating. Immediate postoperative education for a patient with an ileal or colon conduit will focus on learning how to empty the pouch and using the adaptor that connects the pouch to the bedside drainage bag (WOCN, 2022).
Indiana Pouch
Stents placed during surgery are usually left in place for one to two weeks. A Jackson-Pratt drain is also placed proximal to the newly created reservoir and will be removed prior to discharge provided there is no leakage of urine.
During surgery, a 24-Fr Malecot (soft silicone) catheter is placed to drain the Indiana pouch in the immediate postoperative period (Cook Medical, 2025). Irrigation of the Indiana pouch is performed using sterile normal saline to remove mucus from the reservoir, with frequency determined by the amount of mucus present.
A 16-Fr Foley catheter is also positioned during surgery in the Indiana pouch to preserve the patency of the conduit; it is left in situ for a minimum of two to three weeks post surgery.
Neobladder
During surgery, urethral stents are placed to protect the anastomosis; these are passed out of the neobladder and permitted to drain via gravity. A drain (typically a Jackson-Pratt drain) is placed proximal to the reservoir to drain excess fluid that may accumulate. A 24-Fr Malecot catheter is positioned in the neobladder and secured to the patient’s skin. A 22-Fr Foley catheter is inserted into the neobladder reservoir and is used for irrigation in order to prevent the buildup of mucus in the reservoir, similar to the Indiana pouch.
COLOSTOMY
The first postsurgery pouch change is performed by the ostomy nurse or other skilled clinician. This may be performed the day after surgery. If possible, the patient’s family member or caretaker is present for the first pouch change. Observing this first pouch change gives them the opportunity to ask questions and can relieve a lot of anxiety for many patients and family members. Ideally, the patient and caretaker will receive instruction on how to change the pouch and perform a second pouch change later, before the patient is discharged (see below).
Discharge Planning and Patient Education
One of the most challenging times for patients is the transition from the healthcare facility to home.
Patient education begins as soon as the patient can focus on acquiring new skills. Pain must be well managed because a patient who is in pain has neither the desire nor the ability to learn anything new. Since hospital stays are becoming shorter, the clinician must prioritize what to teach the patient and caregiver.
The patient must be able to perform some basic care skills prior to discharge. Whether the patient has a colostomy or ileostomy, the first skill they must learn is how to successfully empty the pouch. Basic steps include:
- Opening the end of the pouch
- Allowing the effluent in the pouch to flow into a receptacle
- Cleaning the end of the pouch and closing securely
Patient education on changing the pouching system includes:
- Reviewing the supplies needed
- Carefully removing the pouching system
- Gently cleaning around the peristomal area
- Assessing the condition of the peristomal skin surface
- Applying the new pouching system, with the bottom end at the “six o’clock” position
For neonates and young children, parents or guardians are educated on how to empty and change the pouching system. Older children can be encouraged to participate in their own pouch change routine.
For patients going home with an ostomy (colostomy or ileostomy), an important consideration in discharge planning is putting in place home healthcare. Ideally, the home health nurse will visit the patient the day after discharge. Outpatient physical therapy or occupational therapy may be recommended for a home evaluation as well if there are concerns about the patient’s ability to safely manage functional mobility or activities of daily living in their home environment (Lane & Gracely, 2020; Mount Sinai, 2025; Keng et al., 2021).
(See also “Ostomy Care at Home” below.)
INDIANA POUCH CARE
The patient can use an overnight bag at home and will need instructions on how to connect the catheter to the drainage bag. During the daytime, a leg bag can be used, and the patient or caregiver is instructed to empty this every two hours. Drainage bags can be cleaned using mild soap and water.
Patients and caregivers should be made aware of the importance of ensuring that the catheter placed in the Indiana pouch remains unblocked and draining. If the catheter stops draining or cannot be flushed or there is concern that the Indiana pouch is distended, the patient or caregiver is instructed to call the surgeon’s office immediately (UR Medicine, n.d.).
Additional discharge instructions and education for the patient with an Indiana pouch include:
- To prevent tugging, secure catheter loosely to the body with a catheter-secure device, tape, or self-adhesive ace bandages.
- When ready to begin self-catheterization (usually two to three weeks post surgery), use clean catheterization technique to access the pouch every two to four hours.
- As soon as the patient has demonstrated proficiency in self-catheterization, the Malecot catheter will be removed and a discrete dressing placed over the catheterized stoma for protection.
- Acquire and wear a medical alert bracelet to alert emergency services personnel to the presence of the Indiana pouch.
The clinician also teaches the patient and caregiver how to perform irrigation prior to discharge. At home this can be done with 30 ml of sterile normal saline every four hours, allowing the fluid to flow back freely into the collection bag (WOCN, 2022; UR Medicine, n.d.).
NEOBLADDER
The patient or caretaker is instructed in performing irrigation post discharge.
Approximately three weeks after the creation of the neobladder, the Malecot catheter is capped, the urethral Foley catheter is taken out, and the patient is instructed to void every two to three hours for the next three weeks. The patient will more than likely experience urine leakage after the Foley catheter is removed, and wearing absorbent pads or briefs for the first few months post surgery may be necessary. The patient is instructed to sit on the toilet when emptying the neobladder, including male patients, since this position aids in relaxing the pelvic floor muscles (Memorial Sloan Kettering Cancer Center, 2025a).
The patient is instructed to return to their healthcare provider’s office about three weeks post discharge to have creatinine and blood urea nitrogen (BUN) levels checked and to have a postvoiding residual measured. At this visit, the Malecot catheter can be removed, but if the patient is experiencing problems emptying the neobladder, the catheter is left in place and unplugged (WOCN, 2022).
Additional discharge instructions to the patient with a neobladder include:
- Shower daily, but don’t take a bath for the first four weeks post surgery. When showering, don’t put soap on the surgical incision, and pat this area dry with a clean towel.
- The goal for fluid intake is eight to ten 8-ounce glasses of fluids daily, while avoiding alcohol and caffeine as much as possible. Sufficient fluid intake is indicated by urine with a light-yellow hue; dark urine is an indication of insufficient fluid intake.
- Always wear a Medic Alert bracelet or necklace. In emergencies this will alert providers that the patient has a neobladder diversion.
- Avoid lifting objects heavier than 10 pounds for a minimum of six to eight weeks.
- Do not engage in activities such as contact sports, running, or tennis for a minimum of three months.
- Participation in activities such as walking and stair climbing will assist the patient in gaining strength and increase overall wellbeing. A good routine includes walking two to three times a day for 20 to 30 minutes each time. However, each patient is advised to determine their activities based on their energy levels.
- Avoid driving for six weeks.
(Memorial Sloan Kettering Cancer Center, 2025a)
Patients may have started instruction in pelvic floor physical therapy exercises prior to surgery, and this may continue with ongoing physical therapy visits for several months (WOCN, 2022). Patients who receive training in pelvic floor muscle exercises from a physical therapist after ostomy closure have been shown to have fewer problems with bowel emptying and an improved quality of life (Aktaş et al., 2024). Physical therapy may include training the patient in a new exercise routine or safely returning to the exercise routine they had prior to surgery. Strengthening the core/abdominal muscles helps to support the stoma, diminishes the possibility of hernias, allows the patient to maintain good posture, and may aid in overall recovery (Colorectal Cancer Alliance, 2025).
HERNIA PREVENTION
Hernia prevention is a main area of concern after abdominal surgery and ostomy creation. There are certain precautions that patients recovering from ostomy surgery need to be educated about and instructed to follow, especially during the first six to eight weeks after surgery. These include:
- Refrain from lifting objects over 10 pounds in weight.
- Avoid tasks such as grocery shopping, doing laundry, and vacuuming, since these push–pull activities increase abdominal pressure.
- With coughing or exertion, support the abdominal incision with one’s hands or a soft item such as small pillow.
(Page & Haberer, 2021)
Therapeutic breathwork, which can be taught by an appropriately trained physical or occupational therapist, is valuable to many patients post ostomy surgery. Breathing correctly lessens intra-abdominal pressure, which in turn lessens the possibility of hernia formation (Foley, 2021).
POST-OP INSTRUCTIONS FOR PEDIATRIC PATIENTS
A key education component for pediatric ostomy care is to apply as few products as possible to the patient’s skin to decrease the likelihood of developing allergic reactions. Gentle cleaning around the stoma with warm water is sufficient. “Baby wipes” are avoided because they contain moisturizers that can make it harder for the skin barrier to attach to the skin around the stoma Depending on the age of the child, it may be necessary to protect the pouching system from dislodging by the child themself. Clothing such as onesies, one-piece undershirts, and overalls may help prevent a child from pulling off the pouch (Convatec, 2025).
QUESTIONS PATIENTS MAY ASK
Q: How long will I have an opening on my belly before I return to regular bowel movements? My cousin had the same surgery, and his ostomy was closed after 6 weeks.
A: Ostomy closure is the goal, but every patient and every surgery are different. Some ostomies may be permanent, while others may be temporary. Your surgeon will be able to give you a better idea specific to your situation.
Q: Why do I need to know all these details about ostomies and their care when it’s only temporary?
A: Even a temporary ostomy can be in place for up to three to six months. You will have to live with and care for your ostomy at home during this time. If it would be helpful, this information can also be provided to a family member, friend, or other caregiver who will be assisting you with your ostomy care.
OSTOMY CARE AT HOME
The ability of a patient to care for their ostomy or continent diversion at home is critical in establishing successful outcomes. Both the patient and any caregivers must practice and perfect their skills in order to manage their self-care independently.
The clinician’s role is primarily education and troubleshooting, not taking care of the ostomy system or changing pouches. What clinician is suited to fill this role depends on the skill set of the clinician and the needs of the patient. For example, a new ostomy patient who requires extra teaching in areas of home management and activities of daily living may be best served by an occupational therapist who is proficient in ostomy care. Another important consideration is the patient and family’s preferences, since they may or may not be happy with home visits from multiple clinicians.
On their first home visit to the patient, the clinician generally performs the following:
- Changes the pouching system
- For a patient with a urostomy, ensures that the stents are in place
- For a patient with a urinary diversion, confirms that urine is draining freely into the pouch and that the patient is experiencing no discomfort
- Reviews with the patient and caretaker the discharge instructions they were previously given and reinforces teaching
- Observes and ensures the patient is emptying the pouch (or leg bag) correctly
- Confirms that adequate supplies are on hand
- Observes whether the home environment is safe and will support self-care by the patient
- Discusses the frequency of home care visits
- Confirms the patient’s follow-up appointment(s)
- Contacts or refers the patient to social services for assistance with transportation, supplies, or other resources, as needed
The basic areas of patient education include:
- Ostomy systems and accessories
- Emptying the pouch
- Removing and applying a new pouch
- Colostomy irrigation (if appropriate for the patient and ostomy type)
- Peristomal skin care
- Diet and fluid intake
- Managing gas and odor
Studies have shown that it can take considerable time for most patients to feel at ease with a new care routine and that challenges may continue long term. Ongoing access to an ostomy nurse or clinician is recommended as a way to mitigate problems that patients encounter and to improve and maintain their quality of life (WOCN, 2022).
SUPPORT SERVICES
Where available, ostomy outpatient clinics have been found to decrease ostomy complications and the need for hospital readmission. United Ostomy Associations of America (UOAA) provides a wide array of support services, including listings for peer support groups. Some ostomy support groups may offer an ostomy visitor program in which trained peers provide person-to-person support, reassurance, and practical information. Ostomy supply companies also provide resources for patients and clinicians. (See also “Resources” at the end of this course.)
Ostomy System and Accessories
A basic ostomy system is composed of two parts:
- Ostomy pouch: Used for collection of the stoma output. Open-end pouches come with a closure system. Closed-end pouches are for one-time use and cannot be emptied and reused.
- Skin barrier (or wafer): Adheres to the patient’s body.
In a one-piece system, the pouch and skin barrier cannot be separated. In a two-piece system, the pouch can be removed, emptied, and reattached to the skin barrier (Convatec, 2022).
| Flat | Convex |
|---|---|
| (WOCN, 2022) | |
|
|

One-piece ostomy system with an open-end pouch. (Source: Reprinted courtesy of Hollister Incorporated, Libertyville, Illinois.)

Two-piece ostomy wafer with the ostomy bag removed. (Source: Eric Polsinelli. CC 4.0 International.)
Examples of add-on ostomy products include:
- Ostomy belt: Fits around the patient’s body and attaches to loops on both sides of an ostomy pouching system; provides a more secure pouch seal and less risk of leakage; typically replaced two to three times a year (Hollister, 2025d; Pittman et al., 2022).
- Ostomy strips: Placed along the edges of the pouching system to keep it more firmly in place and decrease risk of leakage; unlike tape, do not cause skin stripping; usually have moisture-absorbing properties (WOCN, 2022; Medical Monks, 2022).
- Stoma powder: A pectin- or karaya-based hydrocolloid product that protects the skin from exposure to stomal discharge or assists with healing due to peristomal irritation (WOCN, 2022; Byram Healthcare, 2025).
- Paste and skin barrier strips: Similar to stoma powder but in flexible, moldable strip form; used to fill in uneven skin surfaces/crevices around the stoma to create a smooth, flat surface to secure the skin barrier; include karaya-based products that dissolve with contact to urine (WOCN, 2022).
- Skin adhesive: Adds extra security when attaching the ostomy system to the skin, but not used routinely due to skin irritation (WOCN, 2022).
- Pouch liner: A disposable liner placed inside the stoma pouch to collect the output while maintaining a clean pouch.
- Adapter: A small, reusable device that allows a urostomy pouch to connect to other drainage containers, such as a bedside urine collection bag (Hollister, 2025a).
- Urine drainage containers: A bedside or leg bag connected to the urostomy pouching system using an adapter; provides extra collection capacity for urine and decreases the frequency of pouch emptying; can be discreetly worn under clothing when it may not be possible to empty the pouch; to be cleaned daily.
For pediatric patients with stomas, especially those who require a permanent stoma, the scarcity of products to meet their needs may present a barrier to care. However, some companies have created ostomy systems for pediatric patients (e.g., Pouchkins and Little Ones pediatric care ostomy products).
QUESTIONS PATIENTS MAY ASK
Q: If the pouching system starts to leak, can I reinforce it with tape or adhesive strips, or should I change it?
A: A leaking pouching system should be changed to prevent skin damage. Reinforcing it with tape may prolong the wear time, but it does not protect the skin surface from redness and excoriation due to contact with drainage from the pouch.
COST OF OSTOMY SUPPLIES
Patients and families may have concerns about the cost of supplies. The nurse or social worker can help them to work with their healthcare insurance provider to determine what supplies are covered and if there are out-of-pocket costs (WOCN, 2022).
Medicare Part B covers up to three months of ostomy supplies at one time and pays for 80% of allowable charges for supplies after payment of the Part B deductible (MedicareFAQ, 2023). Medicaid generally covers ostomy supplies that are prescribed by a healthcare provider and are deemed medically necessary.
Some companies that produce ostomy supplies have assistance programs to help those who do not have insurance coverage for ostomy supplies. (See also “Resources” at the end of this course.)
Pouch Emptying
There is no one “right” way to empty an ostomy pouch, and over time patients will develop a system that best meets their needs. An initial technique typically includes emptying the pouch into the toilet, as follows:
- Place sheets of toilet tissue into the toilet bowel to avoid splash back.
- Sit on the toilet, with the pouch between the legs, or stand facing the toilet.
- Hold the end of the pouch facing upward and remove the clamp.
- Clean the bottom end of the pouch with toilet tissue, or fold the bottom edge of the pouch back on itself to create a cuff.
- For pouches with hook-and-loop closures, unroll the bottom edge of the pouch and pinch open the end of the pouch to empty.
- Once the pouch is empty, clean the bottom end of the pouch before reclamping or reconnecting the hook-and-loop closure.
For a patient with a two-piece pouching system, it may be more convenient to remove the pouch from the skin barrier, empty the pouch into the toilet, and then reattach the pouch to the flange. For a patient with a urostomy, open the tap on the end of the pouch and empty the urine into the toilet (WOCN, 2022).
The frequency of pouch emptying depends largely on the type of ostomy created. An ileostomy or urostomy pouch must be emptied more frequently than a colostomy pouch, usually from four to six times a day. Unlike with normal defecation or urination, the patient will not perceive stool or urine passing through the stoma into the pouch. Therefore, it is essential for the patient to develop the habit of regularly feeling the pouch to check how full it is.
At the outset, the pouch is emptied when it is one third to one half full, since a heavy, almost-full pouch can pull away from the seal, resulting in leaking and the possibility of peristomal skin damage. A pouch filled with gas can also break the seal, and so some pouches include a charcoal gas filter that permits gas to be expelled while also absorbing odor. If the pouch does not have a filter, the patient opens the end of the pouch and gently uses their palm to expel the gas (WOCN, 2022).
QUESTIONS PATIENTS MAY ASK
Q: Do I need to rinse out my pouch every time I empty it?
A: No, as long as the tail end of the pouch is cleaned after each emptying, there is no need to rinse out the pouch. Although some people feel more comfortable rinsing the pouch, it is important to keep in mind that this practice, if done on a regular basis, can weaken the adhesive seal and increase the risk of the pouch leaking. Ostomy pouches are created to be odor proof, which means that odors do not escape from the pouch.
Removing and Applying a New Pouch
All supplies should be on hand before removing a pouch system:
- Receptable (such as a bedpan) to empty the pouch into prior to changing
- Plastic disposal bag for the old pouch
- Washcloths, towels, or disposable paper towels for cleaning
- New pouching system
- Measuring guide, marker, and scissors
It is not necessary for the patient to wear gloves unless it makes them feel more comfortable. Handwashing is sufficient.
STEPS TO CHANGE A POUCH
- Empty the existing pouch.
- Hold the skin around the ostomy with one hand and gently peel off the pouching system with the other hand (sometimes referred to as the “push–pull” technique), starting at the top and working downward. The pouching system should never be ripped off, which can cause skin stripping and damage to the peristomal skin surface.
- Retain the clip used to close the end of the pouch. Dispose of the removed pouch.
- Carefully examine the peristomal area, which should appear similar to surrounding skin. Redness, skin irritation, and rashes are not normal. The stoma itself should be red, moist, and budded. It is normal for occasional flecks of blood to appear on the stoma, but bleeding should be reported to one’s healthcare provider.
- Clean the peristomal area with warm water and a clean washcloth or disposable towel, and pat dry. Soap is not recommended, as it can cause the buildup of oily residue that can hinder pouch adherence to the skin The stoma itself does not require cleaning; if there is stool present it can be wiped off with toilet tissue.
- Shave any hair in the area under the pouching system, taking precautions not to damage the skin surface.
- Use the measuring guide to correctly size the pouch opening. Since not all stomas are round, make adjustments to the measuring guide or create a new guide to accommodate the actual shape. If the skin barrier (or pouch wafer) is stiff, leave 1/8-inch clearance between the ostomy pouch opening and the stoma.
- Typically, the stoma is measured for the first four to six weeks post operatively until it shrinks to its final size.
- Trace the correct size and cut the new pouch opening, ensuring there are no ragged edges that could scratch the stoma. Take care not to cut too large an opening, which could allow the peristomal skin to come in contact with effluent and increase the risk for skin damage.
- Peel off the protective backing and place the opening over the stoma, with the bottom of the pouch at the six o’clock position.
- Clamp the end of the pouch and confirm it is securely in place.
- Place one’s hands over the opening, one on top of the other, since the heat generated by the hands helps to ensure a good seal.
(WOCN, 2022)
QUESTIONS PATIENTS MAY ASK
Q: Can a regular razor be used to shave abdominal hair in the area around the ostomy stoma?
A: It is advisable to use an electric razor to reduce the risk of accidentally cutting or injuring the stoma. If an electric razor is not available, using small scissors to clip the hair in the direction of the hair growth is another alternative.
FREQUENCY OF POUCH CHANGES
Frequency first depends on the type of ostomy. In general, an ileostomy requires pouch changes twice a week, a colostomy once per week, and a urostomy every three to four days. Manufacturers of ostomy pouching systems typically recommended a maximum pouch wear time of seven days. Beyond that period, the seal becomes less effective and more likely to leak. However, if a pouching system starts to leak, it must be changed immediately to maintain the integrity of the peristomal area. It may be helpful to write the date of the last pouch change on the pouch itself or on a calendar (Drugs.com, 2024).
Factors that influence pouch wear time include:
- Consistency of stoma excretion (e.g., liquid/soft or solid/formed)
- Protrusion of the stoma beyond skin level
- Patient activity level, environmental climate, and amount of perspiration
- Condition of the peristomal area
- Crevices, wrinkles, or skin folds in the peristomal area
- Type and appropriateness of the pouching system used
- Use of skin products under the skin barrier
Attention to good skin hygiene, correct fit, and a regular schedule for ostomy pouching changes will increase wear time (Hollister, 2025b).
OSTOMY EDUCATION FOR PEDIATRIC PATIENTS
Education for children and youth with ostomies is based on their developmental level:
- Toddlers and preschoolers: Education centers primarily on parents or guardians, but the child should be included as far as possible. To introduce an ostomy into the child’s life, items such as an ostomy doll, stuffed animals, coloring books, and story books can be used.
- School-age children (6–12 years): Ostomy education is tailored to the child’s developing independence; children at the upper end of this age group can become independent in their ostomy care. Concerns may include participating in age-associated activities such as sleepovers and camps.
- Teenagers (13–18 years): Teenagers may be fully independent in their ostomy care, with parents or guardians providing a backup role. Hygiene and ostomy care in social situations and in relation to sexuality are typical concerns to this age group. Since teenagers may be hesitant to bring up such topics, clinicians must often raise these topics and elicit the patient’s specific questions.
Maintaining good nutrition, good hydration, and safety issues (such as chewing food well to avert the possibility of an ostomy blockage) are important issues to include in education for all children with an ostomy.
It is important for parents to show empathy for a child with an ostomy. The challenge is to strike a balance between being helpful and overprotective. Usually, very young children who need a permanent ostomy will adapt more easily and grow up accepting the ostomy as part of their lives. However, for teenagers and young adults, who may be sensitive to body image, the creation of an ostomy can be exceptionally difficult. It is advisable that young people with ostomies have access to an ostomy clinician and be provided with an opportunity to meet with an ostomy visitor in their own age group.
(WOCN, 2022)
Colostomy Irrigation
Colostomy irrigation removes stool from the colon with water in place of wearing a colostomy bag all the time. Good candidates for ostomy irrigation include patients with the motivation, understanding, and ability to perform it. This excludes those with poor manual dexterity or eyesight (WOCN, 2022).
Irrigation is appropriate for patients with a permanent left-sided colostomy and when there is formed stool. It requires that the patient have most of the large intestine still in place. Irrigation has not been found to be safe or successful for patients with an ileostomy or right-sided colostomy. Other contraindications to ostomy irrigation include:
- Concurrent chemotherapy or radiation treatments
- Presence of stoma stenosis
- Large parastomal hernia or stoma prolapse
- Diagnosis of Crohn’s disease
- Diarrhea
- Poor prognosis
(WOCN, 2022)
The procedure can take up to one hour, including 5 to10 minutes for water to flow slowly into the stoma and 35 to 45 minutes for stoma output to flow into the toilet. Irrigation is typically done at the same time every one to two days; this can be around the time the patient usually had a bowel movement before surgery or after having a meal or a hot drink. Cramping, abdominal pain, or nausea during irrigation can occur if the water is instilled too quickly or is too hot or too cold. It typically takes six to eight weeks for the bowel to adjust to irrigations and to achieve a regular bowel pattern, at which time the patient can use a stoma cap instead of an ostomy pouch in between irrigations (WOCN, 2022).
Peristomal Skin Care
The peristomal skin should be carefully evaluated each time the pouching system is changed. The skin surface should be intact and free from irritation. Cleaning instructions include:
- Clean the peristomal area gently with warm water and a soft washcloth.
- Avoid aggressive rubbing.
- Pat the area all around, ensuring that it is fully dry.
- Avoid using alcohol or soaps with chemicals that could cause dryness and irritation of the skin.
- For body hair in the peristomal area, carefully clip or shave with an electric razor to prevent problems with attaching the pouching system.
(WOCN, 2022, UOAA, 2024b)
Monitoring Diet and Fluid Intake
Once bowel sounds return, which indicates that the bowel is active again, food intake can be resumed. The first intake may consist mainly of fluids and a low-fiber, low-residue diet (WOCN, 2022). Most persons can resume their regular, presurgery diet, with an emphasis on good nutrition and hydration (Burgess-Stocks, 2022). Eating smaller meals at regular intervals throughout the day may help with regulating ostomy output, but restricting intake and skipping meals should be avoided. Coffee, tea, and alcohol in moderation can all be reintroduced into the diet (UOAA, 2020).
DEHYDRATION
A good fluid intake must be stressed. Persons with an ileostomy are more susceptible to dehydration, since the mechanism for fluid reabsorption in the large intestine is no longer functioning (UOAA, 2020). Ileostomy patients must maintain an adequate fluid and electrolyte intake, in particular, sodium and potassium. Foods high in sodium include broths, tomato juice, canned soups, and vegetables. Those high in potassium include chicken, beef, apricots, bananas, orange juice, potatoes, peppers, and spinach. Hot weather and participation in exercise activities and sports will also require fluid adjustment; sports and electrolyte drinks can be useful in these situations. Patients and caretakers should watch for these signs and symptoms of dehydration:
- Tiredness
- Dizziness, feeling light-headed
- Dry mouth
- Excessive thirst
- Diminished urine output
- Urine that is a darker color than normal
- Abdominal or leg cramps
Dehydration can also be caused by an increase in ileostomy output or by more liquid in the stool. In all cases where the patient or caretaker suspects dehydration, they are instructed to contact their healthcare provider (Coloplast Care, 2020a).
INTESTINAL BLOCKAGE
Another concern for patients with ileostomies is intestinal blockage. This can happen where the intestine comes through the layers of the abdominal wall and is most prevalent during the first six to eight weeks post surgery, when the intestine is still edematous. This swelling leads to narrowing of the intestinal lumen and can prevent certain foods from passing through.
Foods most likely to cause a blockage include high-fiber foods, fruits, vegetables, nuts, and grains, including:
- Beans
- Corn
- Coconut
- Celery
- Coleslaw
- Grapefruit
- Bamboo shoots
- Water chestnuts
- Raisins
- Dried fruits
Other foods of concern for blockage are those with casings, such as sausages (Canadian Society of Intestinal Research, n.d.-a).
Signs and symptoms associated with intestinal blockage are feeling bloated, cramping, abdominal pain, loss of appetite, nausea, and vomiting. A change in ileostomy output may also occur, with watery stools and malodor. The patient or caretaker may notice that the stoma is swollen, and output is coming in noisy spurts. With a complete blockage there will be no output from the stoma.
If the patient or caretaker suspects a blockage, they must seek immediate medical attention. Symptoms that will necessitate urgent care include severe, unrelenting abdominal pain, vomiting, and a lack of stomal output for a period of 12 hours (Canadian Society of Intestinal Research, n.d.-b).
Managing Gas and Odor
Ostomy patients may experience issues with gas. Actions to improve or reduce the amount of gas include:
- Avoiding straws for drinking
- Avoiding eating or drinking too quickly
- Refraining from carrying on conversations while eating
- Not using chewing gum or sucking on hard candies
- Stopping smoking
(Canadian Society of Intestinal Research, n.d.-b)
Most ostomy pouches come with a venting system that allows gas to be expelled without an odor. Also, over-the-counter medications are available that help to reduce gas production. The patient should discuss this option with their healthcare provider to ensure there are no contraindications to their use.
The presence of an odor is another major worry for patients with ostomies. Clinicians can assure them that ostomy pouching systems are odor proof. Steps that can be taken to reduce the possibility of odor include:
- Ensuring that the skin barrier/wafer is securely adherent around the stoma
- Emptying the pouch frequently
- Placing special deodorant deterrents, liquids, or tablets in the ostomy pouch
- Using air deodorizers to eliminate odor during pouch emptying or changes
(WOCN, 2022)
Research has also demonstrated placing lavender or peppermint essential oil in stoma bags as successful in removing odor and in fostering better quality of life in patients with colostomy (Alptekin & Arslan, 2024).
OSTOMY COMPLICATIONS
Ostomy complications can occur at any stage, but evidence indicates that most complications occur during the first five years after ostomy surgery. Risk factors that increase the likelihood of postoperative complications include:
- Older age (≥65 years)
- Gender (women are at higher risk)
- Weight (BMI >25)
- Presence of diabetes mellitus
- Abdominal malignancy as the causative factor for the ostomy creation
(Zelga et al., 2021)
Complications can be divided into two main categories: peristomal skin complications and stoma complications.
Peristomal Skin Complications (PSCs)
PSCs are one of the most common complications in patients with stomas. Studies indicate that the frequency of peristomal skin complications ranges from 11% to 63%. They account for more than 30% of visits to outpatient stoma clinics (WOCN, 2022).
The causes of PSCs include damage to the peristomal area triggered by extended exposure to urinary or fecal discharge due to leakage under or around the skin barrier. Other factors that predispose a patient to PSCs include:
- Mechanical skin damage resulting from improper use of adhesive products
- Pressure injury related to improper use of appliances such as ostomy belts
- Bacterial or fungal infections
- Hypersensitivity or allergic reactions to ostomy products
- Autoimmune immune conditions such as pyoderma gangrenosum
The degree of PSCs fluctuates from mild redness to excoriated or ulcerated skin. It occurs in the area around the stoma that is covered by the adhesive barrier of the pouching system.
Usually, peristomal skin conditions are preventable, and key factors in prevention include patient education in ostomy self-care and emphasis on the importance of seeking treatment as soon as a problem with peristomal skin begins (WOCN, 2022).
ASSESSING THE PATIENT FOR PERISTOMAL SKIN COMPLICATIONS
Assessment begins by taking a full patient history, including the type of ostomy, time since surgery, any problems with self-care, caretaker concerns, and onset of the problem. Important questions for the clinician to ask are:
- What type of ostomy system is being used (i.e., one-piece or two-piece pouching system)?
- Has the patient recently changed the type of ostomy system?
- Since surgery, what has been the usual ostomy pouching system wear time? Has there been a new change in ostomy wear time?
- Have there been problems with leakage? Is this new or ongoing?
- Is the patient experiencing pain, itching, or other sensitivities in the peristomal area and for how long?
(WOCN, 2022)
The clinician should observe the patient with the ostomy pouching system in place. This will allow the clinician to examine how the pouching system has been applied, how well it is adhering to the patient’s skin, and if there are any detectable sites of leakage, pressure, or tension.
Once the pouching system has been removed, the clinician examines the skin barrier, in particular the underside that adheres to the patient’s skin, looking for signs of leakage and where it is occurring. The clinician then gently cleanses the peristomal area while noting its presentation: Is there redness or warmth, skin excoriation, bumps, or areas of swelling? If there is a wound, the clinician measures its size and depth and where it is situated in relation to the stoma (WOCN, 2022).
TYPES AND TREATMENT OF PERISTOMAL SKIN COMPLICATIONS
A great number of peristomal skin complications can occur. The first element in treatment is to identify the cause of the problem, which in many cases is related to the pouching system. Leakage may be occurring because the ostomy pouch is allowed to become too full before it is emptied, thereby putting tension on the skin barrier and breaking the seal. A different size skin barrier may be required. Next is to review patient education on stoma care and the procedure for emptying and changing the ostomy pouch (WOCN, 2022).
Irritant Contact Dermatitis (Moisture-Associated Skin Damage)
Signs/symptoms
- Mild to severe skin breakdown
- Inflammation and erosion of skin surfaces close to the stoma
Common causes
- Skin contact with stool and urine due to leakage from the stoma
Interventions
- Identify underlying cause
- Apply skin barrier powder to denuded areas
- For areas of excessive weeping, apply thin hydrocolloid dressing around the stoma under the pouching system
- Educate patient to keep peristomal area clean and dry
Pseudoverrucous Lesions
Signs/symptoms
- Often a later-developing complication
- More common with urostomies
- Thick elevated areas (papules) around the stoma; grayish white, brown, or deep red in color
- Wart-like growths around the stoma; itchy and may bleed
- Tender to the touch or hard and coarse
Common causes
- Chronic exposure to stool or urine
- Urine alkalosis
Interventions
- Ensure stoma drainage does not contact peristomal area
- For nighttime, use a urine drainage bag
- Cauterize raised lesions with silver nitrate to create an even surface for application of the skin barrier
- Apply skin barrier powder to absorb moisture and provide a dry surface for pouching
- Culture and perform a skin biopsy if lesions don’t respond to standard care
Peristomal Trauma
Signs/symptoms
- Red, excoriated, weeping skin
- Partial- or full-thickness pressure injury directly under the area with excessive pressure
- Pain, moisture, or drainage that makes attaching the ostomy system difficult
Common causes
- Medical adhesive skin damage
- Pressure due to ill-fitting ostomy belts, binders worn too tightly, or use of convex barriers
Interventions
- Identify the source of pressure
- Apply skin barrier powder to improve adherence
- Modify the pouching system or change to different system
- Change to a different size/width ostomy belt
- Educate patient about gentle removal of the pouching system and careful examination of the peristomal area with each pouching change
Fungal Infections
Signs/symptoms
- Redness, maculopapular rash, and scattered lesions
- Burning sensation and intense itchiness
Common causes
- Moisture leading to infection under the adhesive barrier
- Candida albicans as the main causative organism
Interventions
- Gently clean the irritated skin surface, dry the skin, and apply topical antifungal medication
- Examine the pouching system to determine if ostomy discharge is coming in contact with skin
Folliculitis
Signs/symptoms
- Inflammation of the hair follicle
- Erythema and pustules surrounding hair follicles
- Soreness in the area
- Pain when removing the skin barrier
Common causes
- Hair(s) in the peristomal area that stick to the adhesive skin barrier
Interventions
- Clip hair in the direction of hair growth or use an electric razor to shave
- Clean with antibacterial soap
- Apply skin barrier powder and skin sealant to provide a dry surface for adherence
Stoma Complications
Stoma complications can be a significant problem for patients. Some of these occur early in the postoperative phase, while others occur at a later stage.
EARLY STOMA COMPLICATIONS
Early stoma complications typically develop in the first 30 days post surgery. They include mucocutaneous separation, stomal necrosis, and stomal retraction.
Mucocutaneous Separation
Signs/symptoms
- Separation of stomal tissue from the peristomal skin area (separation at skin level is “superficial”; separation into deep tissue that is “full-thickness”)
- Wound bed tissue is either necrotic or healthy and granulating
- Drainage, either serosanguinous, purulent, or containing fecal effluent
Common causes
- Compromised healing, tension, or infection
- Risk factors of diabetes, malnutrition, and steroid medications
Interventions
- For partial and superficial separation:
- Apply hydrofiber or calcium alginate dressings to absorb wound drainage
- Place a skin barrier over the area of separation and peristomal skin to prevent stoma drainage
- Change the pouching system more frequently to provide wound care and assess wound healing
- If infection is present, apply an antimicrobial dressing and consider systemic treatment
- For extensive mucocutaneous separation, consider surgical revision
Stomal Necrosis
Signs/symptoms
- Death of the stoma due to impaired blood supply
- Stoma color and texture advancing from pink to black and changing to flaccid
- Often apparent in the immediate postoperative phase
Common causes
- Insufficient mobilization of the bowel, resulting in tension on stoma
- Inadequate mesenteric circulation, both arterial and venous
- Trauma to stoma tissue during surgery
- High-risk complication in patients with obesity
Interventions
- Immediately report changes in color/texture to the surgical team
- If necrosis is above skin level, no intervention is usually needed beyond close observation (watch for outer, necrotic layer of stoma to shed, exposing a red, workable stoma underneath)
- If necrosis is below skin level but above fascia, observe for flaccid, malodorous tissue; debridement of necrotic tissue is usually recommended
- If necrosis extends below fascia, surgical revision is required
Stomal Retraction
Signs/symptoms
- Stoma that recedes below skin level
- Leakage of discharge under the skin barrier, resulting in poor adherence of the pouching system, skin irritation, and excoriation
Common causes
- Excessive tension on the stoma resulting from multiple factors, such as a short mesentery, adhesions, scar formation, and obesity
Interventions
- Depend on severity
- To increase stoma protrusion above skin level, use a convex skin barrier
- Include an ostomy belt to boost skin-to-barrier adhesion
- If interventions are unsuccessful, surgical revision may be required
(WOCN, 2022; Coloplast, n.d.; Brown, 2022)
LATE STOMAL COMPLICATIONS
Late stomal complications are those that occur beginning 30 days after surgery. They include stomal stenosis, stomal prolapse, and parastomal hernia. Risk factors include a history of Crohn’s disease, malnutrition, and immunosuppression.
Stomal Stenosis
Signs/symptoms
- Narrowing of the stoma passage that impedes flow of effluent
- Pain when effluent is passing through the stoma
- Small, narrow stools, or constipation with explosive passage of effluent
- Large amounts of gas passing from the stoma
- With urostomies, recurrent urinary tract infections, projectile jet of urine, possible flank pain
Common causes
- Development of scar tissue caused by frequent dilation of the stoma
- Crohn’s disease
- Malignancy
Interventions
- Depends on severity
- For mild fecal stenosis, change the diet (e.g., low-residue diet that reduces fiber to decrease bowel movements), increase fluid intake, use stool softeners
- For more severe cases, surgical revision is required
Stoma Prolapse
Signs/symptoms
- More frequent with colostomies than ileostomies
- Stoma that reaches above the skin level by 3 cm to 10 cm greater than anticipated
- Telescoping of the bowel through the stoma
- Risk for stoma edema, injury, and development of ischemia
- With severe or prolonged prolapse, possible incarceration and strangulation of the intestine, with subsequent ischemic changes
Common causes
- Initial construction of a wide stoma
- Increased intra-abdominal pressure
- Risk factors of obesity and older age
Interventions
- Depends on severity
- Assess degree of stomal prolapse with the patient in sitting, standing, and lying positions
- In most cases, reduce the prolapse by having the patient lie supine for a minimum of 10 minutes, applying gentle pressure over the stoma
- Apply ice packs over the pouching system before it is removed to reduce the size of the prolapse
- Adjust the pouching system to contain the extra length of stoma and prevent injury
- Use lubricant on the inside of the pouch to reduce likelihood of trauma to the stoma
- Educate patients to monitor the stoma for changes in color from pink to purplish/red, gray, or black; if changes are noted, seek immediate medical attention
- Surgery may be required to restore intestinal functioning
Parastomal Hernia
Signs/symptoms
- Incisional hernia due to deficiency in the abdominal fascia that permits the intestine to protrude into parastomal area
- Bulging in the area of the stoma
- Problems preserving pouching system seal, leading to leaking and inflamed peristomal skin
- Herniation, but not always apparent to patient
Common causes
- Obesity
- Slackness of the abdominal wall
- Use of steroids
- Disorders that cause an increase in abdominal pressure (e.g., chronic cough, ascites, constipation)
- Inappropriate ostomy site selection or too large of a fascia opening during surgery
Interventions
- Begin with conservative management
- Utilize a flexible pouching system
- Use a hernia support belt and hernia support garments for extra stability to the stomal area; apply while the patient is lying flat; place around the pouch and over the hernia
- Instruct patients to avoid constipation and monitor diet and fluid intake
- If stoma begins to darken in color or if patient experiences unrelieved pain, seek immediate medical attention
- Surgical repair is required in some instances
Pouchitis
Signs/symptoms
- Inflammation in the lining of the pouch
- More frequent passage of stool, bloody stools
- Fecal incontinence
- Abdominal pain, fever, malaise, and hematuria
- Most frequent complication with ileal pouch–anal anastomosis (IPAA)
Common causes
- Exact cause not known
- Risk factors include:
- Inflammatory bowel disease
- Nonsteroidal anti-inflammatory medications (e.g., ibuprofen, naproxen sodium)
- Pelvic radiation therapy
Interventions
- Antibiotic therapy is the primary intervention; ciprofloxacin and metronidazole are recommended
- Dietary interventions include the Mediterranean diet; use of probiotics is being studied
Stone Formation
Signs/symptoms
- Urolithiasis (formation of stones in the upper urinary tract or newly created pouch or conduit)
- High incidence with urinary diversions
Common causes
- Hyperchloremic metabolic acidosis (i.e., pH 7.35)
- Repeated urinary tract infections
- Chronic bacteremia
- Large amounts of mucus in the urine
Interventions
- Ensure good fluid intake, in particular water
- Small stones may pass without any intervention
- Larger stones may require treatment, including extracorporeal shock wave lithotripsy (high frequency sound waves to break up stones)
(WOCN, 2022; Prinz, 2022; Sharma et al., 2022; Murken & Bleier, 2019; Rabbenou & Chang, 2021; Shen, 2024; Mayo Clinic, 2024b; Barnes et al., 2024; Puca et al., 2024; Landmann & Cashman, 2025)
LIVING WITH AN OSTOMY
Successful adaptation to an ostomy is critical to the quality of life for the patient and their families. Areas of concern for the patient with an ostomy may include:
- Returning to work
- Alterations in clothing
- Sexual issues, including pregnancy
- Sleeping
- Sports and recreational activities
- Medications
- Travel
- Aging, illness, and end of life
Returning to Work or School
If the patient is returning to work or school post surgery, it is important to ensure they are ready. Addressing the following issues can be helpful:
- Is the patient able to empty the ostomy pouch without help?
- Is the patient confident they have sufficient energy to meet their work or study requirements?
- Is the patient comfortable about travelling to and from work or school?
- For a patient with a continent urinary diversion that requires regular catheterization, can they take breaks as needed to complete the process?
- Does the patient have a plan in place to address pouch leakages and possibly replace the pouching system?
- Is there an appropriate location available to change the pouching system?
- Is there a location to keep spare clothing at work or school in case of a pouch leakage?
(Hollister, 2025c)
The clinician can also discuss ostomy supplies for a patient who is returning to work or school. Advice includes:
- Carry an ostomy supply bag with spare pouches, catheters, wipes, or other supplies normally used at home.
- Do not leave a supply bag in the car since extreme temperatures can compromise their condition.
- Store an ostomy supply bag in a desk, locker, or other similar location and resupply as needed.
(Hollister 2025c)
A social worker can also assist a patient in understanding their legal rights regarding disability and time off.
Alterations in Clothing
Most ostomy patients have concerns about how an ostomy pouching system will fit under clothing, whether the pouch will be visible to others, or whether they will have to wear baggy clothing. Clinicians can reassure patients and educate them about specialized items for people with ostomies. These include:
- Undergarments with a high waist and an internal pocket for pouch placement
- Ostomy wraps and ostomy belts placed over the ostomy pouching system to provide comfort and concealment
- Shapewear garments
- Stoma guards for stomas placed at or above the belt line (however these may decrease pouch capacity)
(Vegan Ostomy, 2022)
(See also “Resources” at the end of this course.)
Sexual Issues
Several issues can impact relationships and intimacy after ostomy surgery. Effective patient care includes an open, honest discussion with the ostomy patient about their concerns. These may include:
- Body image
- How a partner or potential partner may react to the stoma and pouching system
- Odor, noise, and possible ostomy leakage during moments of intimacy
- Impacts on sexual organs and functioning
The ostomy professional can use the PLISST model to initiate this process:
- Permission
- Limited Information
- Specific Suggestions
- Intensive Therapy
Healthcare professionals should be aware of their own level of comfort discussing sexual functioning and recognize that referral to a specialist may be needed if a patient requires more detailed advice or intensive therapy in this area (WOCN, 2022).
Current recommendations are to allow three to eight weeks of healing time after surgery before resuming sexual activity, according to the needs of each patient. This time period may be extended, depending on the complexity of the surgery and the patient’s underlying condition or in cases of postsurgical chemotherapy or radiation treatment (UOAA, n.d.-b; Cancer Research UK, 2025).
General recommendations for successful sexual intimacy include emptying the ostomy pouch before sexual relations and having a clean, secure pouching system in place. A variety of pouch covers, smaller pouches, and underwear are designed for intimate moments for ostomy patients. Ostomy stomas must never be used for sexual activity due to the risk of damage to the stoma.
FEMALE SEXUALITY AND OSTOMIES
How ostomy surgery will impact sexual function depends on the type of surgery performed. In those with ileostomies or ileal pouch–anal anastomosis, contraceptive pills may be less effective since the medication may not be entirely absorbed. Other contraceptive options may be considered.
Individuals who have had ostomy surgery can become pregnant and experience a normal pregnancy. Those with an ileostomy may be counseled to wait for 12 months post surgery before becoming pregnant (WOCN, 2022).
Other pregnancy-related issues are discussed below:
- Those with an ileostomy may experience incidences of intestinal obstruction during pregnancy because an expanding uterus slows down or obstructs the passage of substances through the intestine and prevents discharge into the pouch.
- Patients with urostomies are more susceptible to kidney infections during pregnancy; they are instructed to maintain a good fluid intake and to seek immediate medical attention if a kidney infection is suspected.
- As the pregnancy advances and the patient’s abdomen enlarges, it may be difficult for the patient to see the stoma; a partner or caregiver may be required to perform pouching system changes.
- Since the size of the stoma may increase, a clinician may be required to assist with measuring the stoma and making recommendations for pouching system changes. Stomal prolapse is a complication that can occur during pregnancy.
- Hormonal changes during pregnancy can affect the peristomal skin and lead to areas of dry skin prone to itchiness and irritation. Patients are advised to clean the peristomal area with a mild, fragrance-free soap. If the area becomes moist and irritated, advice may include medicated soaks (e.g., Domeboro) or applying aluminum acetate to the area for 20 minutes, followed by careful drying before applying the pouching system.
- The type of delivery (vaginal or cesarean) should be explored with the healthcare provider, and if possible, the surgeon who performed the ostomy surgery. While some surgeons recommend cesarean delivery, there have been no large-scale studies of the advantages or disadvantages of one type of delivery over another.
(Hollister, 2019; WOCN, 2022; Cobb, 2021; UOAA, 2023)
MALE SEXUALITY AND OSTOMIES
Males also experience concerns related to sexual functioning after ostomy surgery, but they may be less likely to talk about it or to seek help compared to female ostomy patients.
Problems in the immediate postoperative period may include erectile dysfunction, problems with ejaculation, an inability to attain or sustain an erection, and loss of libido. Male fertility is rarely affected by ostomy surgery. Nerve damage and erectile dysfunction are more likely in cases of deep pelvic surgery or excision of part of the rectum.
In cases of bladder cancer, a radical cystectomy (removal of the urinary bladder) may include removal of the prostate, seminal vesicles, and a portion of the vas deferens, which may result in damage to the nerves responsible for erection, leading to impotence (Memorial Sloan Kettering Cancer Center, 2025b). When cancer is confined to one side of the bladder and there is no indication of high-morbidity prostate cancer, nerve-sparing surgery may be feasible (Black & Kassouf, 2024). Studies have shown that prostate capsule-sparing surgery as part of a radical cystectomy and the creation of an orthotopic neobladder can decrease the likelihood of erectile dysfunction (Dall et al., 2024).
Sports and Recreational Activities
Low-impact activities such as swimming and walking are recommended for a patient with a new ostomy who is resuming activity. Before resuming weight-bearing activities or exercise, an ostomy patient should participate in an exercise program to strengthen the core muscles. A physical therapist, sports therapist, or fitness instructor should be consulted (March, 2022).
For people who want to get back into team and contact sports after the creation of an ostomy, recommendations include:
- Check with the surgeon before resuming any contact sports and follow their recommendations.
- Return in gradual steps to the appropriate level of fitness needed to participate in the chosen activity.
- Keep the pouch securely in place; this may be achieved by using securely fitting waistbands or wearing running tights or well-fitting shorts.
- Empty the pouch before beginning the activity.
- Drink adequate amounts of fluids before and after engaging in sporting activities. (Hollister, 2025e)
Patients with ostomies can participate in swimming and water sports, with the following recommendations:
- Eat lightly prior to water activities.
- Empty the pouch prior to such activities.
- Check the seal of the ostomy wafer around the stoma.
- If the ostomy bag has a deodorizing filter, put a filter sticker over it while in the water; this can be removed when the activity is completed.
- Consider reenforcing the skin barrier by applying waterproof tape to the edges.
- For those who use an ostomy belt, leave the belt in place if they prefer.
(Healthline, 2023)
Sleeping
Clinicians can offer the following advice to help manage an ostomy when sleeping:
- Empty the pouch just before going to sleep.
- If necessary, set an alarm to wake up and empty the pouch, especially for ileostomies or urinary diversions that require catheterization.
- Wear an ostomy wrap or stretch top for extra security against a pouching system coming undone during the night.
- If sleeping alongside a pet, wear an ostomy wrap or belt with heavier fabric to keep the pouch snug against the body and protected against claws.
- Sleeping positions do not need to be altered due to the presence of an ostomy.
(Coulter, 2022)
Medications
Most medications are absorbed in the superior part of the small intestine, and extended-release medications are absorbed in the large intestine. Therefore, ostomy surgery can affect medication absorption, and this must be taken into account for patients with ostomies or continent diversions who are taking medications. Patients must be instructed to inform all healthcare professionals, including dentists and pharmacists, that they have an ostomy. Patients are also advised to watch for undissolved medications in their pouch when emptying it or changing the pouching system and to immediately report this to their healthcare provider (Erbe, 2020).
QUESTIONS PATIENTS MAY ASK
Q: Whom do I need to tell about my ostomy?
A: You only need to share this information with those that you feel need to know and those who you want to know. Decide why you are telling them, then when you want to tell them and how. A good tip is to keep the conversation about your ostomy simple and positive and not to overwhelm the listener with too much detail.
Traveling
Having an ostomy need not prevent a person from traveling, but it often requires preplanning. For an extended trip, planning includes determining whether ostomy supplies can be obtained at the destination; otherwise, supplies can be shipped in advance or packed in large-enough supplies to last the duration of the trip.
For air travel, information about airport screening is available from the Transportation Security Administration (TSA). It is advisable to pack ostomy supplies in at least two different pieces of luggage in case one is lost or delayed. Patients should also research and plan based on luggage restrictions for their means of travel. For example, when scissors are restricted, a convenient option is precut pouches. For liquid, gel, aerosol, cream, or paste, an ostomy patient may be allowed larger quantities due to their medical condition, but these must be declared at the security checkpoint and will require extra screening.
Other travel considerations include always emptying the ostomy pouch prior to travel and avoiding food or snacks that may increase stoma output or gas (UOAA, 2025).
AIR TRAVEL RESOURCES
- UOAA’s Travel Communication Card allows the ostomy patient to discreetly inform TSA agents that they have an ostomy. Another option is a note from the healthcare provider explaining the patient’s medical condition.
- UOAA’s Restroom Access Communication Card provides for access to restrooms during flight when it may otherwise be restricted, at the flight crew’s discretion. It is advisable to show this card to the flight crew before takeoff so that they are aware of the patient’s circumstances.
Aging, Illness, and End of Life
Aging may introduce new issues in ostomy care. Changes in physical abilities, arthritis, vision changes, and cognitive decline, including dementia, can all impact ostomy care. Patients with progressive diseases such as multiple sclerosis and Parkinson’s disease will eventually experience loss in motor skills and the ability to care for their own ostomy. Similarly, changes to body contours, weight, and skin texture can all lead to problems with the pouching system.
Patients are encouraged to continue their own ostomy care for as long as possible. When self-care is no longer possible, care will typically progress to standby supervision, prompting, and eventually hands-on assistance from a family member or caretaker.
For an ostomy patient with terminal cancer, metastasis to the liver can cause peristomal varices (enlarged veins in the peristomal area that can bleed easily). Mild acute bleeding can usually be treated by applying gentle pressure to the peristomal area; severe bleeding or bleeding that cannot be controlled may require hospitalization (WOCN, 2022). For these patients, a one-piece pouching system is recommended, and the caretaker is educated to carefully and gently remove the pouching system to prevent damage to the peristomal varices.
When a patient with an ostomy requires residential care, issues to be addressed with the facility include who will be providing ostomy care, what experience they have, and whether the facility contracts with a certified ostomy clinician who can be called upon for problems (Coulter, 2021).
End-of-life care for patients with urostomies can include attaching the pouch to a larger drainage system, which decreases the need for pouch emptying. For those with continent urinary diversions, the use of an indwelling catheter may be considered (WOCN, 2022).
CONCLUSION
Clinicians are involved in ostomy care from the outset. Once a diagnosis determines that an ostomy or a continent diversion is required, clinicians familiarize patients with the different types of surgeries, ensure that patients are informed of all the options available to them, and confirm that patients and caregivers understand the education they are receiving.
Beyond the acute care phase, clinicians play a pivotal role in the education, care, and on-going assessment of patients recovering from ostomy surgery and living with ostomies and continent diversions. Ostomy support groups can also be a good resource for patients.
For clinicians interested in ostomy certification, the Wound, Ostomy, and Continence Nursing Certification Board (WOCNCB) provides a national certifying exam. The National Alliance of Wound Care and Ostomy (NAWCO) also provides ostomy certification for many different healthcare professionals, including nurses, physical therapists, and occupational therapists.
RESOURCES
National Alliance of Wound Care and Ostomy (NAWCO)
Osto Group (donated ostomy supplies to the uninsured)
Ostomies (American Cancer Society)
Ostomy Home Skills Program (American College of Surgeons)
Support groups (United Ostomy Associations of America)
REFERENCES
NOTE: Complete URLs for references retrieved from online sources are provided in the PDF of this course.
Alptekin D & Arslan S. (2024). The effect of different essential oils used in stoma bags of individuals with colostomy removal of odor, life satisfaction and effect on stoma fit: Randomized control study. EXPLORE, 20(6), Article 103065. https://doi.org/10.1016/j.explore.2024.103065
Aktaş D, Koçaşlı S, & Baykara ZG. (2024). The effect of pelvic floor muscle exercises on bowel evacuation and quality of life in following intestinal ostomy closure: Randomized controlled trial. Journal of Wound, Ostomy, and Continence Nursing, 51(3), 221–34. https://doi.org/10.1097/WON.0000000000001084
American Cancer Society (ACS). (2019a). Types of colostomies and pouching systems. https://www.cancer.org
American Cancer Society (ACS). (2019b). Urostomy guide. https://www.cancer.org
American Gastroenterological Association (AGA). (2023). New clinical practice update: Management of ostomies. https://gastro.org
Barnes EL, Agrawal M, Syal G, Raffals LE, & Singh S. (2024). AGA clinical practice guideline on the management of pouchitis and inflammatory pouch disorders. Gastroenterology, 166(1), 59–85. https://www.gastrojournal.org
Black P & Kassouf W. (2024). Patient education: Bladder cancer treatment; muscle invasive cancer (beyond the basics). UpToDate. https://www.uptodate.com
Brown N. (2022). The retracted stoma. The Phoenix, 18(1), 53–5.
Burgess-Stocks J. (2022). Eating with an ostomy: A comprehensive nutrition guide for those living with an ostomy (2nd ed.). United Ostomy Association of America. https://www.ostomy.org
Byram Healthcare. (2025). Karaya 5 skin barrier powder. https://www.byramhealthcare.com
Canadian Society of Intestinal Research. (n.d.-a). Bowel blockage or obstruction. https://badgut.org
Canadian Society of Intestinal Research. (n.d.-b). Gas in pouch. https://badgut.org
Cancer Research UK. (2025). Your sex life and bowel cancer. https://www.cancerresearchuk.org
Cleveland Clinic. (2024a). Urinary reconstruction and diversion. https://my.clevelandclinic.org
Cleveland Clinic. (2024b). Vesicostomy. https://my.clevelandclinic.org
Cobb T. (2021). Pregnancy with an ostomy. The Phoenix, 16(4), 46–51.
Coloplast Care. (2020a). Ileostomy: Self-care and dietary guidelines. https://www.coloplast.us/Global/US/Ostomy/Professional/Wellness%20Articles/SelfCare_Dietary.pdf
Coloplast Care. (n.d.). Mucocutaneous separation. https://www.coloplast.ca
Colorectal Cancer Alliance. (2025). Physical activity with an ostomy. https://colorectalcancer.org
Convatec. (2025). Common questions about your child’s stoma. https://www.convatec.com
Convatec. (2022). Products basics. https://www.convatec.com
Cook Medical. (2025). Silicone Malecot catheter. https://www.cookmedical.com
Coulter L. (2022). Sleeping with pets. The Phoenix, 17(3), 14.
Coulter L. (2021). Dementia and an ostomy. The Phoenix, 16(1), 51–3.
Cowell JC, Bain KA, Hansen AS, et al. (2019). International consensus results: Development of practice guidelines for assessment of peristomal body and stoma profiles, patient engagement and patient follow-up. J Wound Ostomy Continence Nurs, 46(6), 497–504. https://pubmed.ncbi.nlm.nih.gov
Dall CP, Mason JB, Goldman CC, Fabrizio G, Alagha EC, Chou J, Kowalczyk KJ, et al. (2024). Functional and oncologic outcomes of prostate-sparing radical cystectomy: A systemic review and meta-analysis. Urologic Oncology: Seminars and Original Investigations, 42(5), 121–32. https://www.sciencedirect.com
Drugs.com. (2024). Urostomy care. https://www.drugs.com
Erbe J. (2020). Medication considerations for people with an ostomy. Wound Management and Prevention. https://www.hmpgloballearningnetwork.com
Foley C. (2021). Physical rehabilitation after surgery. https://www.ostomy.org
Haywood SC & Klein EA. (2020). Ileal conduit urinary diversion. https://abdominalkey.com
Healthline. (2023). Can you swim with a colostomy bag? https://www.healthline.com
Hollister. (2025a). Urostomy drain tube adaptor. https://www.hollister.com
Hollister. (2025b). Your ostomy pouching system and wear time. https://www.hollister.com
Hollister. (2025c). 4-point checklist for returning to work after ostomy surgery. https://www.hollister.com
Hollister. (2025d). Adapt ostomy belt. https://www.hollister.com
Hollister. (2025e). Contact and team sports with an ostomy. https://www.hollister.com
Hollister. (2019). Living with an ostomy: Sex & parenthood. https://www.hollister.com
Indiana University (IU) School of Medicine. (2021). 35 years of the Indiana pouch: How IU faculty developed a life-changing procedure used around the world. https://medicine.iu.edu
Janssen GWB, Ramkumar RR, Lee BH, & van der Heijden AG. (2021). Orthotopic urinary diversions after radical cystectomy for bladder cancer: Lessons learned last decade. Current Opinion in Urology, 31(6), 580–85. https://journals.lww.com
Johns Hopkins. (2024). Colostomy: What is a colostomy? https://www.hopkinsmedicine.org
Keng CJ, Lee J, Valencia M, McKechnie T, Forbes S, & Eskicioglu C. (2021). Transition home following new fecal ostomy creation: A qualitive study. J Wound, Ostomy, and Continence Nurs, 48(6), 537–43. https://pubmed.ncbi.nlm.nih.gov
Landmann RG & Cashman AL. (2025). Ileostomy or colostomy care and complications. UpToDate. https://www.uptodate.com
Lane G & Gracely A. (2020). Urostomy patient handbook. Department of Urology, Michigan Medicine, University of Michigan. https://www.med.umich.edu
Laredo JA, Torres-Small S, Patel D, Byerly S, Filiberto DM, & Wood EH. (2025). Recent patterns in minimally invasive colectomies: Where are we now? Laparoscopic, Endoscopic and Robotic Surgery, 8(1), 23–7. https://www.sciencedirect.com
Lucchetti L. (2024). Everything you need to know about Brooke ileostomy. MedicalNewsToday. https://www.medicalnewstoday.com
March A. (2022). Working out with weights: The right way to build strength and stability while avoiding injury. The Phoenix, 18(1), 32–3.
Mayo Clinic. (2024a). Ileoanal anastomosis (J-pouch) surgery. https://www.mayoclinic.org
Mayo Clinic. (2024b). Pouchitis. https://www.mayoclinic.org
Mayo Clinic. (2022). Continent ileostomy. https://medprofvideos.mayoclinic.org
Medical Monks. (2022). Ostomy barrier extenders: How to use them and why. https://medicalmonks.com
MedicareFAQ. (2023). Does Medicare cover ostomy supplies? https://www.medicarefaq.com
Memorial Sloan Kettering Cancer Center. (2025a). About your bladder surgery with a neobladder. https://www.mskcc.org
Memorial Sloan Kettering Cancer Center. (2025b). About your bladder surgery with an ileal conduit (urostomy). https://www.mskcc.org
Minkes RK. (2022). Stomas of the small and large intestine in children. Medscape. https://emedicine.medscape.com
Mount Sinai. (2025). Small bowel resection. https://www.mountsinai.org
Murken DR & Bleier JI. (2019). Ostomy-related complications. Clinics in colon and rectal surgery, 32(3), 176–82. https://doi.org/10.1055/s-0038-1676995
Page A & Haberer P. (2021). What is the right activity after surgery? The Phoenix, 16(4), 38–9.
Pittman J, Colwell J, & Mulekar MS. (2022). Ostomy complications and quality of life of ostomy belt/garment wearers. J Wound, Ostomy, Continence Nurs, 49(1), 60–8. https://pubmed.ncbi.nlm.nih.gov
Prinz A. (2022). Ask nurse Anita. The Phoenix, 17(2), 18.
Puca P, Del Gaudio A, Becherucci G, Sacchetti F, Sofo L, Lopetuso LR, Papa A, Cammarota G, & Scaldaferri F. (2024). Diet and microbiota modulation for chronic pouchitis: Evidence, challenges, and opportunities. Nutrients, 16(24), Article 4337. https://pmc.ncbi.nlm.nih.gov
Rabbenou W & Chang S. (2021). Medical treatment of pouchitis: A guide for the clinician. Therapeutic Advances in Gastroenterology, 14, Article 17562848211023376. https://doi.org/10.1177/17562848211023376
Schmitz JR. (2021). Thesis: Women’s experience receiving occupational therapy for pelvic floor dysfunction: A case series. Department of Occupational Therapy, Colorado State University, Fort Collins, Colorado.
Sharma S, Hashmi MF, & Aggarwal S. (2022). Hyperchloremic acidosis. StatPearls Publishing. https://pubmed.ncbi.nlm.nih.gov
Shen B. (2024). Management of acute and chronic pouchitis. UpToDate. https://www.uptodate.com
Smith DA, Kashyap S, & Nehring SM. (2023). Bowel obstruction. https://www.ncbi.nlm.nih.gov
Sperling CD, Lee DJ, & Aggarwal S. (2021). Urinary diversion: Core curriculum 2021. American Journal of Kidney Diseases, 78(2), 293–304. https://www.ajkd.org
St. Luke’s Health System. (n.d.). What is a colostomy? https://www.saintlukeskc.org
United Ostomy Association of America (UOAA). (n.d.-a). Continent diversions and other ostomy types. https://www.ostomy.org
United Ostomy Association of America (UOAA). (n.d.-b) Sexual well-being and intimacy after ostomy surgery. https://www.ostomy.org
United Ostomy Association of America (UOAA). (n.d.-c). Colostomy facts. https://www.ostomy.org
United Ostomy Association of America (UOAA). (2025). Air travel tips from UOAA and the TSA. https://www.ostomy.org
United Ostomy Association of America (UOAA). (2024a). New ostomy patient guide. https://www.ostomy.org
United Ostomy Association of America (UOAA). (2024b). Basic ostomy skin care. https://www.ostomy.org
United Ostomy Association of America (UOAA). (2023). Labor and delivery. https://www.ostomy.org
United Ostomy Association of America (UOAA). (2021). Ostomy and continent diversion patient bill of rights. https://www.ostomy.org
United Ostomy Association of America (UOAA). (2020). Ostomy diet guidelines after surgery. https://www.ostomy.org
United Ostomy Association of America (UOAA). (2019). The ins and outs of continent diversions for the bladder: What you need to know. https://www.ostomy.org
United Ostomy Association of America (UOAA). (2018). Pediatric ostomy patient bill of rights. https://www.ostomy.org
UR Medicine. (n.d.). Radical cystectomy and Indiana pouch: A patient’s guide. https://www.urmc.rochester.edu
Uzsen H, Yaz SB, & Gumus M. (2021). The effect of ostomy on pediatric patient and family in nursing: A systematic review. Journal of Pediatric Surgical Nursing, 10(4), 153–8. https://doi.org/10.1097/JPS.0000000000000313
Vegan Ostomy. (2022). Dressing with an ostomy: A clothing guide for men (with video). https://www.veganostomy.ca
Wei R, Crook C, & Bamford R. (2024). Abdominoperineal resection. StatPearls Publishing. https://www.ncbi.nlm.nih.gov
Wound, Ostomy, and Continence Nurses Society (WOCN). (2022). Core curriculum ostomy management (2nd ed.). Wolters Kluwer.
Wound, Ostomy, and Continence Nurses Society (WOCN). (2021). WOCN Society, AUA and ASCRS position statement on preoperative stoma site marking for patients undergoing stoma surgery. https://member.wocn.org
Wulff-Burchfield EM, Potts M, Glavin K, & Mirza M. (2021). A qualitative evaluation of a nurse-led pre-operative stoma education program for bladder cancer patients. Supportive Care in Cancer, 29(10), 5711–19. https://doi.org/10.1007/s00520-021-06093-0
Zelga P, Kluska P, Zelga M, Piasecka-Zelga J, & Dzika A. (2021). Patient-related factors associated with stoma and peristomal complications following fecal ostomy surgery. J Wound, Ostomy Continence Nurs, 48(5), 415–30. https://pubmed.ncbi.nlm.nih.gov