Pediatric Abusive Head Trauma
Child Abuse Prevention: Shaken Baby Syndrome
Online Continuing Education Course
Course Description
Recognize and prevent pediatric abusive head trauma (AHT), including shaken baby syndrome. Child abuse prevention CEU course covers definitions and terminology, risk factors, presentation, assessment, diagnosis, intervention and prevention strategies, and reporting.
Course Price: $24.00
Contact Hours: 3
Course updated on
March 18, 2025
"Very good, as usual. Lots of facts I didn't know." - Bette, EMT in Missouri
"The preventative information was particularly helpful for me. I work in pediatric home health and often find myself working with foster children or children involved in CPS as well as children with special needs." - Lynnette, OT in Arizona
"This course contained many updates to my prior training. Very beneficial for early intervention providers." - Deborah, OT in New York
"This was monumentally helpful for pediatric nurses to use." - Emily, RN in Virginia
Pediatric Abusive Head Trauma
Child Abuse Prevention: Shaken Baby Syndrome
Copyright © 2025 Wild Iris Medical Education, Inc. All Rights Reserved.
LEARNING OUTCOME AND OBJECTIVES: Upon completion of this course, you will be better prepared to recognize and help prevent pediatric abusive head trauma (AHT). Specific learning objectives to address potential knowledge gaps include:
- Define pediatric “abusive head trauma” (AHT).
- Recognize the risk factors for head injuries resulting from abuse.
- Describe the mechanisms of injury, clinical presentation, history gathering, physical assessment, and diagnosis of pediatric AHT.
- Distinguish between accidental and abusive head trauma in the pediatric population, including controversies surrounding diagnosis.
- Identify immediate and long-term treatments and interventions for children presenting with pediatric AHT.
- Summarize primary, secondary, and tertiary resources for prevention of pediatric AHT.
- Discuss reporting requirements for suspected child abuse and neglect.
TABLE OF CONTENTS
INTRODUCTION
Child abuse and neglect continue to pose serious threats to the health and well-being of children. In 2022, child protective service (CPS) agencies received approximately 3 million referrals from across the country alleging maltreatment. The largest referral sources were legal and law enforcement (21.2%), education personnel (20.7%), and medical personnel (11.2%). These reports found there to be approximately 558,899 victims of child abuse or neglect, or 7.7 per 1,000 children in the population. This included an estimated 1,990 children who died from abuse or neglect. Children younger than 1 year old had the highest rate of victimization, at 22.2 per 1,000 children of the same age in the national population (Children’s Bureau, 2024).
According to the CDC (2024), abusive head trauma (AHT) is a severe form of child abuse that results in a brain injury. It is often caused by violent shaking (referred to as shaken baby syndrome) or blunt impact. The resulting injury can cause bleeding around the brain or behind the eyes. AHT includes a range of injury mechanisms and clinical outcomes, from subtle presentations to infants with severe and life-threatening injuries.
The diagnosis of AHT should be made by a team of specialists from different medical disciplines, who will consider all available evidence, including physical examinations, imaging tests (radiographs), lab results, and the child’s developmental stage, to ensure the findings cannot be explained by a plausible, nonabusive cause. If necessary, further consultation with specialists like radiologists, ophthalmologists, neurosurgeons, neurologists, and pediatric surgeons should be involved to thoroughly evaluate the case and reach an accurate diagnosis (AAP, 2020; Choudhary et al., 2018, O’Meara et al., 2020).
AHT continues to be a leading cause of physical abuse–related death in children and the leading cause of death from injury in infants. Nearly all victims of abusive head trauma suffer serious, long-term health consequences, including vision problems, developmental delays, physical disabilities, and hearing loss. As many as 1 of every 4 babies who experience abusive head trauma dies from this form of child abuse (CDC, 2024). (See also “Risk Factors” below.)
For children in the first year of life, the majority of serious head injuries result from abuse, and this peak incidence and rapid decrease with age are thought to be related to episodes of prolonged, inconsolable, and unpredictable crying. Such crying can be both a developmentally typical way for infants to communicate their basic needs, but it also can be related to a variety of other health or developmental causes that can be identified through medical examination. Regardless of the etiology, it is important to aim prevention strategies toward supporting parents and caregivers in dealing with crying.
TERMINOLOGY
- Abusive head trauma (AHT)
- The Centers for Disease Control and Prevention (CDC) and the American Academy of Pediatrics (AAP) have recommended using the term abusive head trauma for injuries due to shaking, blunt impact, suffocation, and strangulation, recognizing that inflicted head injury to children can involve a variety of biomechanical forces.
- Pediatric acquired/traumatic brain injury (PA/TBI)
- This term includes traumatic causes such as those sustained as a result of motor vehicle accidents, sports-related injuries, blast injuries from war, assaults or child abuse, gunshot wounds, and falls.
- Shaken baby syndrome (SBS)
- SBS refers to a form of abusive head trauma caused by shaking and with a characteristic pattern of injuries that may include retinal hemorrhages, certain fractures (in particular, ribs and the ends of long bones), and recognizable patterns of brain injury, often including thin subdural hemorrhages and sometimes diffuse axonal injury.
The change in terminology (from shaken baby syndrome to abusive head trauma) was misinterpreted by some in the legal and medical communities as an invalidation of the diagnosis and the mechanism of shaking as a cause of injury. However, the AAP continues to affirm the dangers and harms of shaking infants and embraces the “shaken baby syndrome” diagnosis as a valid subset of an AHT diagnosis and for parental education and community preventative efforts to caution against the detrimental effects of infant shaking (AAP, 2020).
RISK FACTORS FOR ABUSIVE HEAD TRAUMA
Anatomy- and Physiology-Related Risk Factors
There are specifics risks to a young infant due to their anatomy and physiology. These include the combination of a disproportionally larger head, soft and rapidly growing brain, thin skull wall, and lack of mobility and control of the head and neck that makes infants extremely vulnerable to injury from shaking actions.
The anatomic characteristics of a child’s brain render it more susceptible than the adult brain to certain types of injuries following head trauma. The head is larger in proportion to the body surface area, and stability is dependent on the ligamentous rather than bony structures (Verive, 2023). Because the brain grows rapidly during infancy, infants have proportionally larger heads than adults in relation to their body size. (The relation between head and body size continuously declines with increasing age.) Therefore, the head is relatively heavy compared to the rest of the body, which results in different dynamics of head acceleration due to external forces, making the infant head more vulnerable to trauma (Araki et al., 2017).
Additionally, the infant’s brain has higher water content and less myelination than an adult brain, is more gelatinous, and is easily compressed and distorted within the skull during a shaking episode. The infant’s blood vessels around the brain are more susceptible to shearing, and tearing can lead to brain hemorrhages. Because of their minimally developed anatomy, infants are also at increased risk for death and permanent disability.
It is also important to consider that the immature brain requires a different balance of neuro transmission, blood flow, and energy requirements that may predispose it to a poorer injury phenotype. Trauma during this period may also interfere with ongoing developmental events such as neuronal migration and axonal and dendritic growth by altering the proteins that guide these processes (O’Meara et al., 2020).
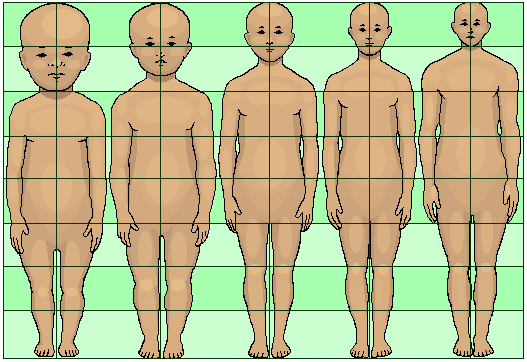
Diagram showing the proportionally larger head of an infant relative to an adult. (Source: Journal of Heredity, 1921.)
Parent / Caregiver Risk Factors
Understanding the risks of AHT from various caregivers may help to inform current prevention strategies. A critical risk factor is the occurrence of shaking used either to attempt to calm infants and children or as a means of discipline. Other risk factors include socioeconomic status, societal and family stress, prematurity, multiple births, developmental delay, and childhood history of abuse in the parent or caregiver.
There are few statistics for risk factors specific to abusive head trauma. Among the limited studies, it is commonly reported that parents were more likely to be perpetrators of the confirmed or suspected child abuse. However, children injured by a parent’s partner—a group that was overwhelmingly male—were more likely to be more severely injured, to experience severe head injuries, and to require intubation compared with children who were abused by a parent.
Laurent-Vannier and colleagues (2021) examined 91 cases of AHT and found that all of the abusive events occurred inside a home (parent’s or childcare provider’s), never outdoors or in a public place, and always in the presence of only one adult. One third of perpetrators were male (n = 32) and two thirds female (n = 59), of which 49 were the childcare provider (“nanny”) and 10 were the infant’s mother. Another study found the percentage of women that shake infants might be higher than previously thought.
Intimate partner violence and adverse childhood experiences (ACEs) are also key risk factors for shaking and harmful parenting behaviors in general (Berthold et al., 2024). These may include traumatic events, such as violence, abuse, or neglect, that occur in childhood and negatively affect a child’s brain development. These disruptions increase the risk of poor physical health, coping skills, or other long-term cognitive impairments (CDC, 2024c).
Risk factors for child abuse in general are described below.
(See also “Protective Factors” later in this course.)
INDIVIDUAL RISK FACTORS IN CAREGIVERS
- Drug or alcohol issues
- Mental health issues, including depression
- Not understanding children’s needs or development
- Abuse or neglect as children
- Being young, single, or having many children
- Low education or income
- Experiencing high levels of parenting stress or economic stress
- Using spanking and other forms of corporal punishment for discipline
- Not being a child’s biological parent
- Holding attitudes accepting of or justifying violence or aggression
(CDC, 2024b)
RELATIONSHIP / FAMILY RISK FACTORS
- Having household members in jail or prison
- Being isolated from and not connected to other people (extended family, friends, neighbors)
- Experiencing other types of violence, including relationship violence
- High levels of conflict
- Negative communication styles
(CDC, 2024b)
COMMUNITY RISK FACTORS
- High rates of violence and crime
- High rates of poverty and limited educational and economic opportunities
- High unemployment rates
- Easy access to drugs and alcohol
- Neighbors who don’t know or look out for each other
- Low community involvement among residents
- Few community activities for young people
- Unstable housing and residents who move frequently
- Frequent food insecurity
(CDC, 2024b)
It is also important to note that there is limited and inconsistent evidence on the validity and reliability of risk assessment instruments in primary care settings. The literature describes that the use of such instruments may cause harm, including social stigmas and effects on family functioning and dynamics, due to inaccuracies in screening questions and ethnic bias (Hart et al., 2024).
Child Risk Factors
Children with disabilities or special healthcare needs—including those born prematurely or having developmental delays or disabilities—are at higher risk for AHT. A lack of understanding of premature infant development may lead to additional frustration, stress, decreased tolerance, and resentment among caregivers. Since premature infants have a higher rate of disabilities than full-term infants, their risk is even greater.
Infants experiencing neonatal abstinence syndrome (NAS) (i.e., babies in withdrawal) are at particular risk for child abuse, including abusive head trauma, due to the irritability and excessive crying that result from withdrawal from substance addiction. This can last for weeks and months, making such babies difficult to care for.
Additionally, the CDC (2024b) reports that the following characteristics increase an infant’s risk for being shaken, particularly when combined with a parent or caregiver who is not prepared to cope with caring for a baby:
- A history of previous child abuse
- Infant prematurity or disability
- Being one of a multiple birth
- Being less than 6 months of age
- Being perceived as inconsolable or crying frequently
CASE
Jasper is 3 and a half months old and was born prematurely at a gestational age of 34 weeks. He was admitted to the emergency department (ED) after his father called 911 because Jasper turned blue while being bottle fed. Emergency personnel had started CPR because Jasper was not breathing, and they were unable to get a pulse. Jasper had been seen by his primary care physician three times since his discharge from the neonatal intensive care unit and has been diagnosed with colic, feeding difficulties, and possible gastroesophageal reflux.
Jasper was initially resuscitated in the ED, and once he was stable, an evaluation revealed multiple injuries consistent with pediatric AHT. Jasper was transferred to a regional pediatric intensive care unit and was removed from life support three days later because he had irreversible brain stem dysfunction.
Jasper’s father later reported that Jasper’s mother had just returned to work after six weeks of parental leave. He had agreed to look after the infant, but he lost his temper and shook Jasper because he kept on crying and refusing the bottle.
ASSESSMENT AND DIAGNOSIS OF PEDIATRIC ABUSIVE HEAD TRAUMA
Mechanism of Injury
Abusive head trauma encompasses many mechanisms of injury. Children who present with AHT may have been injured due to shaking, blunt impact, suffocation, strangulation, and other causes. It is important to remember that no single injury is diagnostic of AHT (Choudhary et al., 2018).
Each type of imposed stress produces a characteristic pattern of injury:
- Acceleration and deceleration through an arc (shaking) produce thin subdural hemorrhage and, commonly, retinal hemorrhages.
- Impact is associated with skull fractures, contra-coup bruising, and unilateral subdural hemorrhage.
- Strangulation causes hypoxia and hypoxic ischemic encephalopathy.
These stresses may occur separately or in any combination.

When a baby is shaken, the neck snaps back and forth and the brain rotates, causing shearing stresses on the vessels and membranes between the brain and skull. (Source: Radiologyassistant.nl.)
Clinical Presentations
Healthcare professionals may first encounter young children with AHT in a range of clinical settings, including primary care, urgent care, and emergency departments. Since there are significant variations in the clinical presentation of children with AHT, it is important that professionals are trained to identify potentially life-threatening situations.
While there is an increased awareness about AHT and how it may present, it is still important to realize that AHT may present with subtle signs and symptoms. A history of trauma is rarely reported in the initial assessment stages, and if it is, it is usually reported as a fall from a distance of less than five feet (APA, 2020).
Less severely injured infants and young children may present with symptoms that are quite nonspecific and without a history of trauma provided by a caregiver. These symptoms may be transient and improve if the trauma is not repeated. They include irritability, vomiting, and apnea. These and other symptoms of AHT are also seen in other minor medical conditions and can easily lead to a mistaken diagnosis of those conditions instead. Healthcare providers may have difficulty recognizing that such symptoms are the result of abuse, and the infant may return to an abusive environment (see also “Differential Diagnoses” below).
More seriously injured children have symptoms that should lead to rapid diagnosis of intracranial trauma. The caregiver may report a dramatic change in level of consciousness, as in acute collapse, such as unconsciousness, apnea, or seizures. An episode of minor trauma may be given as an explanation for the injury. Examples include falls off beds, being dropped by caregivers, or other minor contact injuries to the head.
Presenting History
Any reported history or statements made by the caregiver regarding the injury should be documented accurately and completely. It is best to include the specific questions asked as well as the responses. Information should be gathered in a nonaccusatory but detailed manner.
There are two general portions of the presenting history that are important to document. The first is the history of the injury event, and the second is how the child responded or behaved after the injury.
Questions asked when taking a presenting history should include:
- What happened?
- Who was there when it happened?
- Where did it happen?
- When did it happen?
- What happened afterwards?
- When was the child noticed to be ill or injured? How did the child respond? When did symptoms start? How did you respond?
- What made you bring the child to the doctor (or hospital)?
- When was the last time the child was totally normal or well?
- What has the child been doing and how have they appeared during the last 24–48 hours?
Medical, Developmental, and Social History
Information that may be useful in the medical assessment of suspected physical abuse includes:
- Past medical history (trauma, hospitalizations, congenital conditions, chronic illnesses)
- Nutrition history
- Seizure history
- Medications and immunizations
- Family history (especially of bleeding, bone disorders, and metabolic or genetic disorders, which often appear as a history of early deaths)
- Pregnancy history (wanted/unwanted, planned/unplanned, prenatal care, postnatal complications, postpartum depression, delivery in a nonhospital setting)
- Familial patterns of discipline
- Child temperament (easy to care for versus fussy)
- History of past abuse to child, siblings, or parents, including history of CPS or police involvement
- Developmental history of child (language, gross motor, fine motor, psychosocial milestones)
- Substance abuse by any caregivers or people living in the home
- Social and financial stressors and resources (unemployment, divorce/separation, etc.)
- Violent interactions among other family members
(Christian & Levin, 2018)
The social history is a critical component of the evaluation. Asking parents about the household composition, other caregivers, siblings, substance abuse, mental illness, and social stressors can provide valuable information. It is preferable to interview caregivers separately; thorough and accurate documentation, including the use of quotes, is critical.
CAUSES FOR CONCERN
Examples of findings that are of concern for possible AHT include:
- Any infant or young child whose history is not plausible or consistent with the presenting signs and symptoms (i.e., explanation that is inconsistent with the pattern, age, or severity of the injury or injuries)
- History of behavior that is inconsistent with the child’s physical or developmental capabilities
- Presence of a new adult partner in the home
- History of delay in seeking medical attention
- History or suspicion of previous abuse
- Absence of a primary caregiver at the onset of injury or illness
- Physical evidence of multiple injuries at varying stages of healing
- Unexplained changes in neurologic status, unexplained shock, or cardiovascular collapse
Physical Assessment
There are various signs and symptoms of AHT that can be recognized in a physical assessment of the child. Depending on the severity of the clinical presentation, initial assessment is often focused on identifying and treating life-threatening issues. This initial assessment focuses on the airway, breathing, circulation, and neurologic status.
As noted above, the consequences of less severe cases may not be brought to the attention of healthcare professionals and may never be diagnosed. In the most severe cases, which usually result in death or severe neurological consequences, the child usually becomes immediately unconscious and suffers rapidly escalating, life-threatening central nervous system dysfunction.
Common presenting signs and symptoms of AHT are:
- Lethargy/decreased muscle tone
- Extreme irritability
- Decreased appetite, poor feeding, or vomiting for no apparent reason
- Grab-type bruises on arms or chest
- No smiling or vocalization
- Poor sucking or swallowing
- Rigidity or posturing
- Difficulty breathing
- Decreased level of consciousness
- Seizures
- Head or forehead appears larger than usual
- Fontanel (soft-spot) on head appears to be bulging
- Inability to lift head
- Inability of eyes to focus or track movement
- Unequal size of pupils
(NCSBS, n.d.-a)
Complete physical exam for any young child with suspected AHT includes:
- Inspection of all body parts, scalp, ears, and hair
- Inspection of the mouth (lip, tongue, buccal) to observe for frenula tears or dental injuries
- Palpation of legs, arms, hands, feet, and ribs to assess for crepitus or deformities
Nursing neurologic assessment of the child with head trauma includes evaluation of:
- Eye opening
- Arousability level or irritability/consolability
- Symmetry of facial expressions
- Movement of upper and lower extremities
- Increased weakness or pitch in cry/vocalizations
- Fontanels
- Each pupil separately for size, shape, equality of reaction to light
- Ability to track objects
- Muscle tone for rigid extension or flexion of extremities, flaccidity, or unusual posturing
Research has identified several specific types of injuries as being associated with AHT. These include retinal hemorrhage in 85% of cases, subdural hematoma in over 70%, and hypoxic-ischemic injury and cerebral edema as significantly associated with AHT (O’Meara et al., 2020).
RETINAL HEMORRHAGE (RH)
Retinal hemorrhage is bleeding in the back wall of the eye. Retinal hemorrhages are a common but not universal finding in AHT. Clinical and pathological studies have shown strong associations of severe RH and AHT, especially in infants. It is important to understand, however, that RHs can result from other causes, including medical disease (coagulopathy or leukemia) or accidental or birth trauma.
Retinal hemorrhages can vary in size, number, and location within the retina itself. An examination by using indirect ophthalmoscopy is required in the evaluation of AHT, preferably by an ophthalmologist with pediatric or retinal experience. Distinguishing the number, type, location, and pattern of RHs is important in evaluating a differential diagnosis. Hemorrhages that extend to the ora serrata and involve multiple layers of the retina are strongly associated with AHT. Because some RHs can be transient, it is important to conduct the eye exam as soon as possible if AHT is suspected (Christian & Levin 2018).
It has been widely assumed that the major cause of retinal injury (RI) is acceleration–deceleration forces repeatedly imposed during abusive shaking. However, Shahraki and Suh (2024) state that few investigations have sought to delve into the biomechanical or biochemical features of RI using realistic models and that knowledge regarding AHT/SBS-induced RI is still significantly lacking.
SUBDURAL HEMATOMA (SDH)
Subdural hematoma is bleeding inside the skull but outside the brain. SDH is found in the majority (up to 90%) of victims of pediatric AHT. Although SDH is not exclusive to abusive trauma, a number of studies have demonstrated a significant and strong association of SDH with abuse compared with accidental injury. This is because inflicted injuries with or without impact can lead to tearing of cerebral convexity bridging veins at the junction of the bridging vein and superior sagittal sinus and also because rupture of the arachnoid membrane allows cerebrospinal fluid to enter the subdural space (Choudhary et al., 2018).
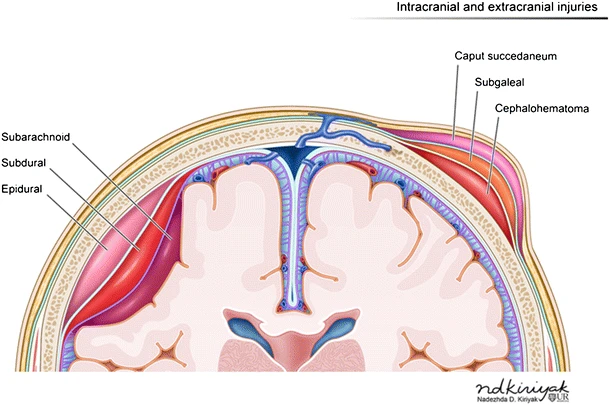
A subarachnoid hemorrhage can be seen in the subarachnoid space between the dura mater and pia mater layers of the meninges. (Source: ND Kiriyak, Creative Commons Attribution 4.0.)
FRACTURES
The possibility of concurrent fractures in other parts of the body is important to consider in children presenting with possible AHT. A multicenter study found fractures in 32% of AHT cases. The skull (43%) and ribs (48%) were affected most frequently, but only 8% of the cases showed classic metaphyseal lesions. In 48% of the cases, healing fractures were present (Feld et al., 2021).
Understanding the unique physiology of children’s skeletal injuries is crucial for correctly differentiating between injuries incurred from normal childhood trauma and those from abusive trauma in general. Fractures in children can be divided into the following three categories based on the relative likelihood of accidental versus abusive origin:
- Highly specific injuries include metaphyseal fractures (such as classic metaphyseal lesions [CMLs]), rib fractures (especially posterior), skull fractures, scapular fractures, sternal fractures, and outer-third clavicular fractures.
- Moderate-specificity fractures include multiple fractures (especially if bilateral), fractures of different ages, epiphyseal separations, vertebral body fractures, digital fractures, spinal humeral fractures, and complex skull fractures.
- Common but low-specificity fractures include middle clavicle fractures, long-bone shaft fractures, and linear skull fractures.
(Knipe, 2020)
Moderate- and low-specificity fractures become highly specific when a credible history of accidental trauma is absent, particularly in infants.
SKIN LESIONS AND BRUISING
Bruising is the most common injury from physical abuse and the most common injury to be overlooked or misdiagnosed before an abuse-related fatality or resulting in an error in medical decision-making that leads directly to poor patient outcomes. A multicenter study found skin lesions (hematomas and abrasions) in 53% of AHT cases, with the face (76%), scalp (26%), and trunk (50%) being the major sites. In 48% of cases, healing skin lesions were observed. Nearly 80% of the cases with fractures also showed skin lesions (Feld et al., 2021).
The mnemonic TEN-4-FACESp was developed as a bruising clinical decision rule for distinguishing abusive from nonabusive trauma in children based on the characteristics of their bruising. Any bruising on a child age 4.99 months or younger is considered an affirmative finding. Likewise, an affirmative finding in children age 4.99 years or younger for any one of the following three components indicates a potential risk for abuse and warrants further evaluation by the medical team:
- Is there bruising in the TEN (torso, ears, or neck) regions?
- Is there bruising or injury involving the FACES region (frenulum, angle of jaw, cheeks, eyelids, subconjunctivae)?
- Is the bruising patterned (P)?
(Pierce et al., 2021)
ORAL INJURIES
The mouth should be fully examined and any missing or abnormal teeth recorded. It is also very important to be aware of normal dentition in a child and to be alert to subtle changes (e.g., the most common oral injuries described are bruising or lacerations to the lips). Other possible oral injuries include unexplained bruising to the cheeks, ears, neck, or trunk in association with a torn frenum. A torn frenum may occur with force-feeding an infant.
SPINAL INJURIES
Evaluating for spinal injuries is a common practice in the diagnosis of AHT and is seen as both clinically and forensically valuable. Spinal injury has been associated with more severe injury, and spinal subdural hemorrhage might support a mechanism of severe acceleration–deceleration head injury and a diagnosis of AHT (Rabbitt et al., 2020).
ABDOMINAL INJURIES
Liver lacerations and other abdominal organ injuries are often seen in AHT cases but are commonly missed because these internal injuries are not visible to the naked eye. Blood tests (liver transaminase levels, pancreatic amylase and lipase) can immediately alert clinicians to the possibility of an occult abdominal injury.
Diagnostic Procedures
All infants and children with suspected AHT require cranial computed tomography (CT), magnetic resonance imaging (MRI), or both.
CT SCAN
A CT scan is usually the first modality of choice diagnostically in symptomatic children due to its availability, rapidity, and ability to look at brain parenchyma, vascular structures, bone, and scalp. The CT in AHT, usually performed without contrast media, may demonstrate intracranial bleeding, both parenchymal or extra-axial (between the brain and skull).
A CT of the head will identify abnormalities that require immediate surgical intervention and is preferred over MRI for identifying acute hemorrhage and skull fractures and scalp swelling from blunt injury. Three-dimensional (3D) image reconstruction is better than plain films in identifying and delineating skull fracture. Abdominal CT scan is the most sensitive imaging mode and is recommended when abdominal injury is suspected.
MRI
MRI is the optimal modality for assessing intracranial injury, including cerebral hypoxia and ischemia, and is used for all children with abnormal CT scans, asymptomatic infants with noncranial abusive injuries, and for follow-up of identified trauma (Christian, 2015). There is increasing data to support MRI of the spine, since spine MRI can identify ligamentous changes, spinal subdural hemorrhage, and other diagnostic evidence of abusive head trauma. Full spine is recommended rather than cervical spine alone because of the tendency of subdural blood to track down (Rabbitt et al., 2020).
SKELETAL SURVEY
Skeletal surveys are recommended as the universal screening/examination in cases of known or suspected physical abuse and in serious head trauma in children younger than 2 years of age because they can help detect otherwise occult trauma to the bones. Skeletal surveys are conducted per the American College of Radiology parameters (see below). Full-body “baby grams” (radiographs that include the whole body or the chest and abdomen on a single image) should be avoided in place of a skeletal survey since they are not sufficient to rule out fractures (ACR, 2021). Images are reviewed by someone with adequate expertise in the field (i.e., pediatric radiologist). If an adequate study cannot be readily obtained, transferring or referring a patient to a pediatric center with expertise in performing and reading skeletal surveys should be strongly considered.
While bony injuries are rarely life threatening, they can provide important evidence for the diagnosis of physical abuse. Skeletal surveys can help to identify characteristic injury patterns such as the classic metaphyseal lesion (CML) in long bones, sometimes referred to as “bucket-handle” and “corner” fractures according to their appearance, which are strongly suggestive of abuse. The femur, humerus, and tibia are the most common long bones to be injured in child abuse, and these long bone fractures in nonambulatory children, along with rib fractures, should cause high suspicion for abuse. CMLs are the most common long bone fracture found in infants who die with evidence of abusive injury. These fractures are thought to be caused when torsional and tractional shearing strains are applied across the metaphysis, as may occur with vigorous pulling or twisting of the infant’s extremity (Haney et al., 2025).
Fractures of the sternum, scapula, and pelvis are typically the result of high-energy trauma, such as a motor vehicle collision, pedestrian-struck, or a fall from a height. These fractures are also rare in children and should trigger concern for abuse in the absence of a verifiable traumatic incident (Haney et al., 2025).
Per the American College of Radiology parameters, skeletal surveys in cases of known or suspected child abuse should include all elements described in the table below.
| (ACR, 2021) | |
| Appendicular skeleton |
|
| Axial skeleton |
|
LAB TESTING
The standard workup for AHT (or any physical abuse) includes:
- CBC (complete blood count)
- Coagulation panel
- CMP (comprehensive metabolic panel)
- Lipase
- Urinalysis
- Von Willebrand’s panel or antigen (depending on availability)
- If any fractures are present:
- Calcium
- Phosphorous
- Alkaline phosphatase
- Parathyroid hormone (PTH)
- Vitamin D 25-hydroxy
NEUROLOGIC ASSESSMENT TOOLS
Pediatric neurologic assessment tools include a variety of scales healthcare professionals can use to assess and monitor level of consciousness in young children. The Glasgow Coma Scale (GCS) continues to be one of the most widely used to evaluate injury severity of young children presenting with altered level of consciousness. Any combined GCS score of less than 8 suggests severe brain injury and represents a significant risk of mortality (see table below).| Behavior | Response | Score |
|---|---|---|
| (Brainline.org, n.d.) | ||
| Eye opening | Does not open eyes | 1 |
| Opens eyes in response to painful stimuli | 2 | |
| Opens eyes in response to speech | 3 | |
| Opens eyes spontaneously | 4 | |
| Verbal response | No verbal response | 1 |
| Inconsolable, agitated | 2 | |
| Inconsistently inconsolable, moaning | 3 | |
| Cries but consolable, inappropriate interactions | 4 | |
| Smiles, orients to sounds, follows objects, interacts | 5 | |
| Motor response | No motor response | 1 |
| Extension to pain (decerebrate response) | 2 | |
| Abnormal flexion to pain for an infant (decorticate response) | 3 | |
| Infant withdraws from pain | 4 | |
| Infant withdraws from touch | 5 | |
| Infant moves spontaneously or purposefully | 6 | |
| Total score | Best response | 15 |
| Comatose client | 8 or less | |
| Totally unresponsive | 3 | |
SCREENING TOOLS
Screening tools continue to be researched for their validity in showing high prediction for AHT. While none are aimed to diagnose AHT, they may prompt clinicians to seek further clinical, social, or forensic information.
Hymel and colleagues derived the PediBIRN four-variable clinical rule for predicting AHT. The objective of this tool is to detect AHT among acutely head-injured children admitted to the pediatric intensive care unit. Currently, the four variables include:
- Any clinically significant respiratory compromise before admission
- Bruising of the torso, ears, or neck
- Bilateral or interhemispheric subdural hemorrhages or collections
- Any skull fractures other than an isolated, unilateral, nondiastatic, linear, or parietal fracture
(Schermerhorn et al., 2024)
The Pediatric Brain Injury Research Network is also looking to validate a seven-variable tool that incorporates the (positive or negative) predictive contributions of patients’ completed skeletal surveys and retinal exams (PBIR, 2025).
The Predicting Abusive Head Trauma (PredAHT) tool was developed to help healthcare providers differentiate accidental head trauma from AHT. This tool estimates the probability of AHT in young children presenting with intracranial injuries and specific combinations of six features:
- Head or neck bruising
- Seizures
- Apnea
- Rib fracture
- Long-bone fracture
- Retinal hemorrhage
The estimated probability of AHT varies from 4% when none of the features are present, to >81.5% when three or more of these six features are present, to nearly 100% when all six features are present (Pfeiffer et al., 2020).
CHILD ABUSE PEDIATRIC (CAP) SPECIALISTS
Child Abuse Pediatric (CAP) subspecialists are responsible for evaluating, diagnosing, and treating the pediatric population for suspected child maltreatment. Arriving at a correct diagnosis has significant ramifications for the child and family. In addition to clinical care, CAP subspecialists act as a resource for their communities, providing education and guidance to medical and mental health providers, child protective services (CPS), law enforcement, and community agencies. They also participate in death reviews and provide testimony at court proceedings.
Despite the high rates of child abuse and neglect, CAP is one of the smallest pediatric subspecialties, considering it works with some of the most vulnerable children and families, and engages with a variety of other pediatric stakeholders. The CAP workforce faces numerous challenges, including few fellows entering the field, decreased financial compensation compared with other fields of medicine, and threats to workforce retention, including secondary trauma and harmful exposure in the media (Slingsby et al., 2024).
Distinguishing Between Accidental and Abusive Head Trauma
There are several challenges to differentiating between accidental (nonabusive/noninflicted) trauma or age-appropriate injuries and child abuse in infants and young children. This is especially true in children who are not yet verbal enough to explain what happened to them (i.e., infants, toddlers, and children with developmental delay or altered levels of consciousness).
Because of this, knowledge of typical developmental patterns of injury is helpful. That is, how does the presenting pattern(s) of injury and the child’s age and developmental level match up with the reported mechanism of injury?
DEVELOPMENTAL PATTERNS OF INJURY
Developmental patterns of injury seen in the 0- to 3-year-old range (the age range most frequently seen with AHT) include:
- Trauma from falls from furniture, down stairs, or being dropped by another person
- Traumatic delivery (e.g., forceps, vacuum extraction, or breech)
- Motor vehicle accidents
Head injury is frequently involved with these traumas because of several factors, including the larger head-to-body ratio and the inability to shield oneself during a fall.
Developmentally, this age range is at risk for accidental injury because the child’s developmental milestones include increasing motor skills and curiosity, allowing them a greater range and access to potential hazards. The advancing physical abilities of young children often precede their ability to understand the consequences of their actions. Thus, parent/caregiver knowledge of growth and developmental milestones may reduce the likelihood that they will misjudge the ability of the child and utilize an inappropriate supervision strategy. The mechanisms seen in accidental (noninflicted) injuries are generally different in these types of injuries as compared to AHT, as discussed below.
ASSESSMENT QUESTIONS
Because this situation is highly charged for both the family and all the healthcare providers involved, it is a good idea to have a checklist in place to both pose questions and evaluate responses in relation to the specific patient in question. Providers should objectively and clearly document the history as described by the parents or caregivers present.
The following are questions a clinician can ask themself to help separate the unintentional from the inflicted injury:
- What is the age of the child?
- What are the normal behaviors of a child at that age? Developmental stages of childhood determine what kinds of injuries are likely to be seen. The motor skills of the child determine what the child could have done to incur injury.
- Based on the child’s age, is the presenting injury plausible?
- Is the history plausible? Could this injury have been sustained in the manner described? Does the history change with changing information supplied to the caretaker? Adjustments in the account of the injury may be made by caretakers to fit the evolving information, indicating the tailoring of the history to fit new information. Does the history change when related in subsequent accounts by other family members?
- Was the injury witnessed? The lack of information as to how a serious injury has occurred should raise the index of suspicion for an abusive origin.
- Is the social situation in which the injury occurred a high-risk environment? The presence of community or intrafamilial violence, substance abuse, chaotic living arrangements, poverty, social isolation, transient lifestyles, mental health issues, and conflict among family members are red flags.
- Can the described mechanism of injury account for the observed injury? What else could produce the clinical picture?
- Can the history be independently verified (through photographs, scene investigation, etc.)?
Explanations that are concerning for intentional trauma include:
- No explanation or vague explanation for a significant injury
- An important detail of the explanation that changes dramatically
- An explanation that is inconsistent with the pattern, age, or severity of the injury or injuries
- An explanation that is inconsistent with the child’s physical or developmental capabilities
- Different witnesses who provide markedly different explanations for the injury or injuries
(Christian, 2015)
WHAT TO DO WHEN CONSIDERING A DIAGNOSIS OF AHT
- Call law enforcement directly from the point of care if there are any immediate concerns for the child’s safety.
- Call social services. They can assist in interviewing family members and in discussions with CPS.
- Call child protective services. They will take a report and decide whether to pursue an investigation. Often, CPS is involved in assisting with the disposition of the child if not admitted (i.e., they will make a safety plan) or when the child goes home from the hospital. CPS may also contact law enforcement.
- Call a child abuse consultant. These professionals are key in suggesting studies for workup as well as discussing appropriate disposition. Regional child abuse centers often have a consultant on call if there is not one available in one’s own system.
- General guidelines for discharge. If there is any question about the child’s injury or safety at home (e.g., unexplained injury) or further workup is required (e.g., skeletal survey), the child should be admitted to the hospital for observation and protection until the workup can be completed and a safe disposition decision can be made between admitting provider, child abuse consultant, social services, and CPS.
(See also “Reporting Child Abuse and Neglect” below for information on when a healthcare provider may be mandated to report suspected AHT.)
CASE
Anthony is an 11-month-old admitted to the ED with a history of altered level of consciousness and multiple facial, skull, and body soft tissue injuries after a reported “fall down the stairs while in a baby walker.” This occurred while he was at a family childcare home. He regained consciousness but was very irritable.
On arrival to the ED, the triage nurse assessed his airway, breathing, circulation, and level of consciousness. He received a prompt evaluation by the ED physician for head trauma because of the history. In this case, the details of the event and injury patterns seemed to match up. Anthony had a CT of the head and ophthalmologic evaluation, and both were found to be negative.
Anthony was discharged home from the ED after observation. The family childcare home was cited for a health and safety violation.
Differential Diagnoses
It is also important to rule out underlying conditions that may cause some of the same signs or symptoms associated with AHT or other abuse. Where indicated, medical professionals should inquire about the presence of any of the following conditions or practices:
- Congenital, metabolic, or neoplastic conditions (e.g., aneurysm, arteriovenous malformation, brain tumor, leukemia)
- Connective tissue disease or osteogenesis imperfecta, which may lead to fragile bones that fracture with less force than would be expected
- Acquired causes (e.g., meningitis, obstructive hydrocephalus)
- Undetected bleeding disorders that can lead to abnormal bleeding patterns (e.g., hemophilia, Von Willebrand’s disease, liver disease)
- Traditional or alternative healing practices, which may lead to unusual bruising and scarring patterns (e.g., coin rubbing, cupping, or burning herbs on the skin over acupuncture points)
(Waters-Tozier, 2020)
MEDICOLEGAL CONTROVERSIES SURROUNDING POTENTIAL MISDIAGNOSIS OF ABUSIVE HEAD TRAUMA
There has been significant medicolegal media attention related to the potential misdiagnosis of AHT (Colloff, 2024; Lennon, 2024). It is important that healthcare providers are aware of these controversies and keep current on the challenges of diagnosing AHT.
Because AHT is considered by some to be a commonly misdiagnosed condition, several systematic reviews have looked at the compiled research on diagnosis. Maiese and colleagues (2021) evaluated the current scientific evidence on best practices, including the importance of circumstantial evidence, clinical history, the use of postmortem radiological examinations (such as CT and MRI), and autopsy.
Tibballs and Bhatia (2024) reviewed AHT cases from Australia, the United Kingdom, and the United States. They reported “that on expert opinion alone, a ‘triad’ of clinical signs (severe retinal hemorrhages, subdural hematoma, and encephalopathy) is dogmatically attributed diagnostically to severe deliberate shaking with or without head trauma. However, the evidence for this mechanism is of the lowest scientific level and of low to very-low quality and therefore unreliable. Consequently, expert opinion should not determine legal outcomes in prosecuted cases. Expert witnesses should reveal the basis of their opinions and the uncertainties and controversies of the diagnosis.” This review suggested abandonment of the inherently inculpatory diagnostic terms shaken baby syndrome and abusive head trauma and their appropriate replacement with infantile retinodural hemorrhage.
An earlier review by Lindberg and colleagues (2019) reported that new science is changing accepted medical opinion about abusive head injury that has frequently made the medicolegal press involving abusive head trauma. The review analyzed published scientific articles about AHT to determine whether this new information has led to significant changes in the understanding, evaluation, and management of children with suspected AHT. They concluded that:
- The overwhelming weight of recent data does not change the fundamental consensus.
- Abusive head trauma is a significant source of morbidity and mortality in children.
- Subdural hematomas and severe retinal hemorrhages are commonly the result of severe trauma.
- These injuries should prompt an evaluation for abuse when identified in young children without a history of such severe trauma.
- Short falls, cerebral sinus thrombosis, and vaccinations are not plausible explanations for findings that raise concern for abusive head trauma.
INTERVENTION FOR PEDIATRIC AHT PATIENTS
Resuscitation (attention to airway, breathing, and circulation) and stabilization efforts for patients with traumatic brain injury take priority because of the often life-threatening presentation of the child with AHT. Intervention then focuses on detection of primary injury (as discussed above), treatment of that injury, and prevention or treatment of secondary brain injury.
Acute Management of Traumatic Brain Injury
Medscape publishes “Practice Guidelines” for pediatric head injury treatment and management based on a review of the current pediatric traumatic brain injury (TBI) literature. (A brief synopsis of the guidelines is discussed here; see Verive, 2023, in “References” at the end of this course to access the full guidelines.)
INITIAL MANAGEMENT
The initial management (first-tier therapy) of a child with a traumatic brain injury begins with strict attention to the maintenance and stabilization of the patient’s airway, breathing, and circulation (blood pressure), utilizing basic and advanced resuscitation algorithms (AHA, 2020).
Those with decreased consciousness (GCS <9), marked respiratory distress, or hemodynamic instability require advanced airway management to enhance oxygenation and ventilation and prevent aspiration of gastric contents. Early airway management involves providing proper airway position, removal of debris while maintaining cervical spine precautions, and orotracheal intubation. Adequate ventilation is needed to prevent both hypercarbia and hypoxia, as they are both potent cerebral vasodilators that result in increased cerebral blood flow and volume and, potentially, increased intracranial pressure (ICP) and intracranial hypertension (ICH).
Orotracheal intubation allows for not only airway protection in patients who are severely obtunded but also for better control of oxygenation and ventilation. Nasotracheal intubation should be avoided because of the risk of cervical spine injury and direct intracranial injury, especially in patients with basilar skull fractures.
Oxygenation is best monitored using pulse oximetry, with supplemental oxygen administered when necessary to ensure adequate oxygenation. For initial monitoring of ventilation of children with traumatic brain injury, capnography is recommended to monitor end-tidal CO2 to avoid excessive hyperventilation and resultant hypocapnia, thereby leading to vasoconstriction and decreased cerebral perfusion.
PREVENTING SECONDARY BRAIN INJURY
A primary goal in the acute management of the severely head-injured pediatric patient is to prevent or ameliorate the factors that promote secondary brain injury. Secondary brain injury involves an endogenous cascade of cellular and biochemical events in the brain that occurs within minutes and continues for months after the primary brain injury and that leads to ongoing or “secondary” traumatic axonal injury (TAI) and neuronal cell damage (delayed brain injury) and, ultimately, neuronal cell death.
The following treatable conditions can exacerbate secondary brain injury:
- Hypoxemia
- Hypotension
- Elevated intracranial pressure (ICP) leading to intracranial hypertension (ICH)
- Hypercarbia or hypocarbia
- Hyperglycemia or hypoglycemia
- Electrolyte abnormalities
- Enlarging hematomas
- Coagulopathy
- Seizures
- Hyperthermia
In order to prevent secondary brain injury, intracranial pressure management is crucial. Raising the head of the bed to decrease venous obstruction may help to control ICP. Traditionally, elevation of the head to 30° in the midline position was recommended, but titration of head elevation to achieve the lowest ICP is optimal.
Every effort should be made to avoid hypotension in these patients because hypotension has been shown to increase morbidity and mortality. Euvolemia should be maintained. However, isolated TBI rarely leads to severe hypotension. Other causes of trauma-related hypotension include but are not limited to:
- Intra-abdominal injuries
- Pericardial tamponade
- Hemothorax
- Pneumothorax
- Spinal cord injury causing spinal shock
Intracranial monitoring. For patients with severe TBI or a GCS score of ≤8 and suspected ICH, an ICP monitor may be placed. Intracranial hypertension is associated with poor neurologic outcome. The following treatments may also be considered by the neurosurgical team:
- Analgesia, sedation, and neuromuscular blockade
- Osmotic therapy
- Carefully monitored hyperventilation
- Temperature control (although therapeutic hypothermia remains controversial)
- Decompressive craniectomy
- Antiseizure prophylaxis
(Verive, 2023)
Nursing Care Planning
Nursing care planning for children with AHT and their families may be very complex and includes addressing the following diagnoses and issues:
- Risk for altered parenting (defined as inability of the primary caregiver to create, maintain, or regain an environment that promotes the optimum growth and development of the child)
- Risk for violence related to history of family violence
- Risk for injury related to physical or psychological conditions in the environment
- Hopelessness related to long-term family stress
- Post-trauma response related to physical or psychosocial abuse
Nursing care will generally involve significant discharge planning and referral to appropriate healthcare and social services. The treatment of child abuse is complex and often involves long-term psychotherapy for the parents or other perpetrators as well as the child. Most states require some kind of counseling for the parents (see also below under “Prevention Strategies”).
SECONDARY TRAUMA IN HEALTHCARE PROFESSIONALS
The development of secondary traumatic stress (STS) is a common occupational hazard for professionals working with traumatized children. The symptoms of secondary trauma may include feelings of isolation, anxiety, dissociation, physical ailments, and sleep disturbances and can be associated with a sense of confusion, helplessness, and a greater sense of isolation from supporters than is seen with typical job burnout. It is not uncommon for traumatized professionals to believe they can no longer be of service to their clients and end up leaving their jobs or the serving field altogether.
Protecting against the development of secondary traumatic stress includes factors such as longer duration of professional experience and the use of evidence-based practices while providing care. The most important strategy for preventing secondary traumatic stress is the triad of psychoeducation, skills training, and reflective supervision to both reduce risk and increase resiliency to secondary stress. Specific strategies may include:
Organizational Strategies
- Provide adequate clinical supervision, including reflective supervision
- Maintain trauma caseload balance
- Support workplace self-care groups
- Enhance the physical safety of staff
- Offer flextime scheduling
- Incorporate STS training for clinical staff
- Create external partnerships with STS intervention providers
- Train organizational leaders and nonclinical staff on STS
- Train organizational leaders on organizational implementation and assessment
- Provide ongoing assessment of staff risk and resiliency
Individual Strategies
- Use supervision to address STS
- Increase self-awareness of STS
- Maintain healthy work–life balance
- Exercise and implement good nutrition
- Practice self-care
- Stay connected
- Develop and implement plans to increase personal wellness and resilience
- Continue individual training on risk reduction and self-care
- Use employee assistance programs (EAPs) or counseling services as needed
- Participate in a self-care accountability buddy system
(NCTSN, n.d.)
Rehabilitation and Recovery
Because the brains of infants and young children are still developing, AHT can result in widespread impairment and dysfunction. AHT can impact the trajectory in all developmental domains. The long-term outcomes of AHT often include impairments in a child’s sensory motor, cognitive, behavioral, and emotional functioning. Together, these problems can cause long-term consequences in everyday functioning, social and academic areas, as well as participation in society and community integration. The recovery process is influenced by the child’s pre-injury status, the acute care period, and the responses of the patient’s family, school, and community.
HEALTH AND DEVELOPMENT CONDITIONS RELATED TO AHT
- Learning disabilities
- Physical disabilities
- Visual disabilities or blindness
- Hearing impairment
- Speech disabilities
- Cerebral palsy
- Seizures
- Behavior disorders
- Cognitive impairment
- Death
(NCSBS, n.d.-a)
Rehabilitation includes teaching strategies and providing supports to both the child and family to compensate for impaired or lost functions and to optimize abilities. Partnering with a child’s school, if applicable, is vital to making sure the child receives the services needed to achieve academically and socially in a safe and appropriate manner.
A multidisciplinary approach to both the inpatient and outpatient phases of rehabilitation care is essential. Interventions might include but are not limited to pharmacologic, physical, occupational, vision, hearing, speech–language, psychological, behavioral, or educational therapies. Rehabilitation continues working toward patient/caregiver goals in order to facilitate as much functional improvement as possible.
When interventions no longer yield improvements in function, the child transitions into a period of “habilitation” that addresses ways to support the child and family with activities of daily living. Professionals must now understand that recovery and supportive care may be a lifelong process for the child’s entire circle of family, friends, and healthcare providers.
Researchers have found that higher-quality early and later home environments and family functioning predict better outcomes for all children. This is especially essential for children with traumatic brain injury, including AHT. One study looked at the overall quality of the home environment as was measured according to eight different factors:
- Learning materials, provision of appropriate play materials
- Language stimulation
- Physical environment, including regularity and predictability of the environment
- Parental responsivity
- Learning stimulation
- Modeling of social maturity
- Variety in experience
- Acceptance of child (i.e., parental acceptance of suboptimal behavior and avoidance of restriction and punishment)
(Durber et al., 2017)
CASE
Nina is now a 6-year-old girl who suffered a traumatic brain injury due to AHT as an infant. Per court records, her mother came home from her second day back at work and found Nina, then a 3-month-old, with her arms twitching. Nina was being cared for by her father, the mother’s boyfriend. Her mother took Nina to the emergency department of the local hospital, but by the time they arrived, the twitching had stopped. After several hours of observation, they were sent home.
That evening Nina ate poorly and vomited. The next morning Nina’s mom found her unresponsive, with abnormal posturing. Her mother called 911. Nina was stabilized in the ED and transferred to a tertiary care pediatric medical center. She was in the intensive care unit for two weeks and the pediatric rehabilitative unit for three weeks. Nina was discharged to a foster home.
The father reported that he had accidently dropped Nina the day before, but the history and clinical presentation did not match up, and the father was arrested for child abuse. He was later convicted for child abuse because of the physical findings associated with Nina’s case.
Nina’s mother was able to regain custody of her after three months and a lengthy police and child welfare investigation. To regain custody of Nina, her mother was required to take parenting classes and was referred to public health nursing, Early Head Start, and early intervention services. The maternal-child health specialist, public health nurse, and early intervention service coordinator helped Nina’s mother learn how to organize Nina’s daily medical care and walked her through how to access and advocate for the variety of services and supports that the family was going to need to support Nina’s special needs.
Nina was diagnosed with cerebral palsy, neurologic (cortical) vision impairment, seizure disorder, and global developmental delay. She is technologically dependent on a gastrostomy tube for her nutrition needs. Nina continues to have severe developmental disabilities and delays (she is both nonambulatory and nonverbal) and receives special education and related services, including physical, occupational, and speech therapies. The school nurse, county health department public health nurse, Individualized Family Service Plan (IFSP), and Individualized Education Plan (IEP) team members work regularly with Nina’s family to ensure that her educational, therapeutic, and medical needs are met. Nina also has a home care nurse who provides respite care. It is predicted that Nina will need care for all of her activities of daily living for the rest of her life.
PREVENTION STRATEGIES FOR ABUSIVE HEAD TRAUMA
There is an increasing focus on ways that healthcare providers have a unique opportunity to support families in forming and maintaining relational health, defined as safe and stable relationships that protect and nurture a child’s growth and development, thereby helping to prevent child abuse (Stirling et al., 2024).
Protective Factors
Research has shown that certain protective factors are linked to a lower incidence of child abuse and neglect in general. They are attributes that serve as buffers, helping parents who might otherwise be at risk of abusing their children to find resources, supports, or coping strategies that allow them to parent effectively, even under stress.
Individual protective factors in caregivers include:
- Creating safe, positive relationships with children
- Practicing nurturing parenting skills and providing emotional support
- Meeting basic needs of food, shelter, education, and health services
- Having a college degree or higher and having steady employment
Relationship/family protective factors include:
- Having strong social support networks and stable, positive relationships
- Being present and interested in the child
- Enforcing household rules and engaging in child monitoring
- Having caring adults outside the family who can serve as role models or mentors
Community protective factors include:
- Access to safe, stable housing
- Access to high-quality preschool
- Access to nurturing and safe childcare
- Access to safe, engaging afterschool programs and activities
- Access to medical care and mental health services
- Access to economic and financial help
- Access to work opportunities with family-friendly policies
CDC (2024b)
Alternative approaches are now being considered that support the above protective factors. These include:
- Creating and validating a broader array of family well-being outcomes that are correlated with child well-being (e.g., parental stress, access to resources)
- Expanding research on the drivers of, interventions for, and consequences of racial and ethnic bias in addressing child maltreatment
- Increasing study of risk factors that include adversity faced by families in the form of access to childcare, healthcare (particularly mental health and substance use treatment), housing, and food insecurity
- Considering population-level metrics for measurement of child maltreatment
- Increasing study of policy-level changes to improve the well-being of children, such as tax credits, expanded subsidies for childcare, and guaranteed paid parental leave
(Hart et al., 2024)
For example, research on state paid family leave (PFL) policies as a community/societal protective factor suggest that PFL has a beneficial effect on infant maltreatment rates and adds to the growing evidence that policies aimed to support household economic stability could be a vital child maltreatment prevention policy tool (Tanis et al., 2024).
SOCIAL-ECOLOGICAL MODEL
Social-ecological theory examines how people exist within and are shaped by their individual characteristics, families and other relationships, communities, and society. The overlapping rings of the graphic below illustrate how protective factors against potential child abuse at one level influence factors at other levels.
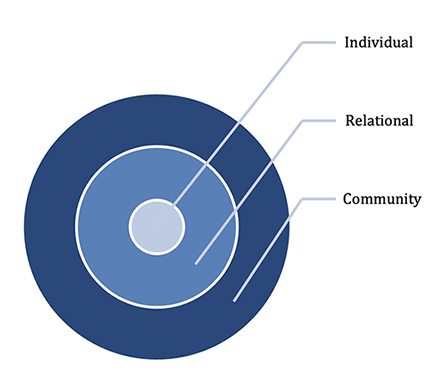
Community/society protective factors
- Community norms of shared responsibility for supporting parents and families
- Implementation of evidence-based practices
- Access to basic needs and specialized services
Relational protective factors
- Relationships with peers and reduced feelings of isolation
- Positive relationships within the extended family
- Ability to communicate emotions effectively
- Engagement in social institutions (e.g., schools, faith communities)
- Secure parent–child relationships
Individual protective factors
- Stress management
- Access to concrete support
- Hopefulness
- Problem-solving skills
- Resilience
- Parenting skills
(CWIG, 2020)
Prevention Continuum to Strengthen Families
Prevention and child welfare policies can be viewed across a spectrum of comprehensive supports. Primary prevention efforts address a broad segment of the population, such as all new parents. Secondary prevention efforts target a specific subset of the population considered to be at higher risk for child maltreatment. Tertiary prevention efforts target perpetrators of child maltreatment and seek primarily to prevent recidivism (CWIG, n.d.).
PRIMARY EFFORTS: GENERAL POPULATION AND PARENT EDUCATION
Many states have enacted programs aimed at preventing child abuse, including pediatric abusive head trauma, through a public health primary universal prevention strategy aimed at changing knowledge and behaviors of caregivers and society in general concerning normal development of infants and the significance of early increased infant crying. By increasing parental understanding of infant development, with a focus on infant crying and coping strategies to address it, such programs are thought to offer a “window of opportunity” for the prevention of AHT and, potentially, other forms of infant abuse.
Primary prevention activities are directed at the general population and attempt to stop maltreatment before it occurs. All members of the community have access to and may benefit from these services. Primary prevention activities with a universal focus seek to raise the awareness of the general public, service providers, and decision makers about the scope and problems associated with child maltreatment.
Healthcare professionals can provide the following messages to parents and caregivers during their everyday encounters:
- Remind parents and caregivers that crying is normal for babies.
- Explain to parents that excessive crying is often a normal phase of infant development.
- Ask parents how they are coping with parenthood and their feelings of stress.
- Assure parents that it is normal to feel frustrated at long bouts of crying and a sudden decrease in sleep but that things will get better.
- Give parents the number to a local helpline or other resource for help.
- Talk with parents about the steps they can take when feeling frustrated with a crying baby, such as putting the baby safely in a crib on their back, checking on the baby’s safety every 5 to 10 minutes, and calling for help or a friend.
- Let parents know what to check for when their baby is crying: signs of illness, fever, or other behavior that is unusual; discomfort like a dirty diaper, diaper rash, teething, or tight clothing; or whether the baby is hungry or needs to be burped.
(CBCS, 2021)
Period of PURPLE Crying
The Period of PURPLE Crying is an example of a primary-level program specifically geared to the prevention of AHT. The target population is all parents of new infants and society in general, with the goal of increasing their understanding of early infant crying and shaken baby syndrome. The Period of PURPLE Crying training, when taken by nurses, has also been shown to improve nurses’ short- and long-term understanding of AHT and their confidence in instructing parents and caregivers about its associated dangers and risks (Dias et al., 2021).
| (NCSBS, n.d.-b) | ||
| P | Peak of crying | Your baby may cry more each week, peaking at 2 months, then less at 3 to 5 months. |
| U | Unexpected | Crying can come and go, and you do not know why. |
| R | Resists soothing | Your baby may not stop crying no matter what you try. |
| P | Pain-like face | Your crying baby may look to be in pain even when they are not. |
| L | Long lasting | Crying can last as much as 5 hours a day or more. |
| E | Evening | Your baby may cry more in the late afternoon or evening. |
The PURPLE program includes a booklet plus either a smart phone “app” that parents can use to track crying and access other developmental and anticipatory guidance information or a DVD. The program is designed to help parents of new babies, caregivers, and the public to understand the typical crying curve and the dangers of reacting to an infant’s crying in frustration and shaking a baby. It is based on over 30 years of scientific research on the connection between the infant crying curve and the incidence of SBS and is delivered using a specific protocol (NCSBS, n.d.-b).
(See also “Resources” at the end of this course.)
SECONDARY PREVENTION EFFORTS
Secondary prevention efforts, such as home visitation programs, target a specific subset of the population considered to be at higher risk for child maltreatment due to factors such as poverty, parental substance abuse, young maternal age, parental mental health concerns, and parental or child disabilities. Approaches to prevention programs that focus on high-risk populations might include:
- Parent education programs located in high schools and focusing on teen parents or located within substance abuse treatment programs for mothers and families with young children
- Parent support groups that help parents deal with their everyday stresses and meet the challenges and responsibilities of parenting
- Respite care for families who have children with disabilities or special healthcare needs
- Family resource centers that offer information and referral services to families living in low-income neighborhoods
- Home visiting programs that provide support and assistance to expecting and new mothers in their homes
(CWIG, n.d.)
Home visiting is a mechanism to provide direct support and coordination of services for families, beginning prenatally or at birth. Visits are conducted by a nurse, social worker, or trained paraprofessional. Programs vary, and components may include:
- Education in effective parenting and childcare techniques
- Education on child development, health, safety, and nutrition
- Assistance in gaining access to social support networks
- Assistance in obtaining education, employment, and access to community services
The efficacy of home visiting programs continues to be challenging to evaluate, especially as they relate to child abuse prevention. Multiple studies have concluded that the strategy, when well implemented, produces significant and meaningful reduction in child-abuse risk and improves child and family functioning. Other studies are more limited in their conclusions (CBCS, 2021).
Nurse-Family Partnership
The Nurse-Family Partnership program provides home visits by registered nurses to first-time, low-income mothers, beginning during pregnancy and continuing through the child’s second birthday. It operates nationwide. The program has three primary goals: 1) to improve pregnancy outcomes by promoting health-related behaviors; 2) to improve child health, development, and safety by promoting competent caregiving; and 3) to enhance parent life-course development by promoting pregnancy planning, educational achievement, and employment. The program also has two secondary goals: 1) to enhance families’ material support by providing links with needed health and social services and 2) to promote supportive relationships among family and friends (NFP, 2023).
Health Access Nurturing Development Services (HANDS)
Kentucky’s HANDS program is an example of a program designed to assist overburdened first-time parents at critical development points. Frequent pre- and postnatal home visits by trained professionals are provided to first-time parents. These appointments assist new parents by sharing important information, problem solving, and helping them to meet basic needs such as housing, food, healthcare, and other required services. All of Kentucky’s 120 counties offer the HANDS program at no cost to families. Enrollment must be during pregnancy or when the infant is less than 3 months old, and referral to HANDS is made through the county health department (KY CHFS, 2025).
CASE
Martha is a 19-year-old who is currently six months pregnant. Her history is significant in that she was removed from her biological mother at 12 years of age because her mother was addicted to methamphetamine and Martha had been physically and sexually abused by her mother’s boyfriend. Martha has lived with two foster families and dropped out of high school at age 16. The father of her unborn baby is not involved, and Martha is currently living with her new 26-year-old boyfriend, who has a history of substance abuse but is now “clean and sober.”
Martha is receiving prenatal care at Planned Parenthood, is signed up for Women, Infants, and Children (WIC), and is getting ready to take her high school equivalency exam so she can work once the baby can be safely cared for. Because of her risk factors, the nurse at Planned Parenthood provides Martha with written information and helps her download an app on her phone for the Period of PURPLE Crying program. The nurse also provides a referral to the local Nurse-Family Partnership program, where a public health nurse has been assigned to her case.
OTHER CHILD ABUSE PREVENTION PROGRAMS
The Child Welfare Information Gateway and the California Evidence-Based Clearinghouse for Child Welfare (CEBC) maintain databases on other evidence-based programs. Several child-abuse prevention and home-visiting programs have been reviewed and scientifically rated by the CEBC for use in children under 3 years of age. Rated programs must either have goals or objectives directly related to the prevention of child abuse or neglect or have published peer-reviewed research measuring outcomes directly related to the prevention of child abuse or neglect, such as data on reports of abuse or neglect behaviors through a standardized measure.
1–Well-supported by research evidence
- Nurse-Family Partnership
- Safe Environment for Every Kid (SEEK)
2–Supported by research evidence
- Child First
- Dads Matter HV
- Early Start
- Kinship Navigator Children’s Home Network (CHN-KN)
- SafeCare
- Triple P Positive Parenting
3–Promising research evidence
- ACT Raising Safe Kids
- Building Healthy Children
- Exchange Parent Aide
- Parents Anonymous
- Parents as Teachers (PAT)
- Period of PURPLE Crying
- Upstate New York Shaken Baby Syndrome Education Program
(CEBC, 2025a, 2025b, 2025c)
TERTIARY PREVENTION EFFORTS
Tertiary prevention activities focus on families where maltreatment has already occurred and seek to reduce the negative consequences of the maltreatment and to prevent recidivism. These prevention programs may include services such as:
- Intensive family preservation services with trained mental health counselors that are available to families 24 hours per day for a short period of time (e.g., six to eight weeks)
- Parent mentor programs with stable, nonabusive families acting as role models and providing support to families in crisis
- Parent support groups that help parents transform negative practices and beliefs into positive parenting behaviors and attitudes
- Mental health services for children and families affected by maltreatment to improve family communication and functioning
(CBCS, 2021)
SafeCare is one example of an evidence-based training curriculum for parents who are at risk or have been reported for child maltreatment. Parents receive weekly home visits to improve skills in several areas, including home safety, healthcare, and parent–child interaction (CEBC, 2023).
STATES’ EFFORTS TO REDUCE AHT
Many states have enacted legislation intended to reduce the incidence of AHT. For instance, states may require that, prior to discharge, each woman who gives birth in a hospital or a free-standing birthing clinic receive information or watch a presentation describing the nature of, dangers of, and methods for the prevention of AHT. Several states require childcare personnel to be trained in recognizing and preventing AHT and understanding early childhood brain development. Several states have established a statewide shaken baby syndrome prevention program that involves a multiyear, collaborative approach.
REPORTING CHILD ABUSE AND NEGLECT
Pediatric abusive head trauma is a form of child abuse, and all U.S. jurisdictions have statutes that mandate reporting of suspected child abuse and neglect for certain professionals. Familiarity with state laws will ensure that providers report to the appropriate agency within the required time frame. Some states have provided the option of making such a report through the Internet. Information on specific state laws is provided by the Children’s Bureau of the Administration for Children and Families, U.S. Department of Health and Human Services.
(For state-by-state information on mandated reporting, see “Child Welfare Information Gateway” in the “Resources” section at the end of this course.)
Who Must Report Abuse?
Anyone may report suspected child abuse at any time and is encouraged to do so (i.e., permissive reporters). Such reports are typically confidential and may be made anonymously by members of the public.
All U.S. jurisdictions also have laws that mandate reporting of suspected child abuse or neglect. Currently, 47 states, the District of Columbia, American Samoa, Guam, the Northern Mariana Islands, Puerto Rico, and the Virgin Islands designate specific professions whose members are mandated by law to report child maltreatment. The three remaining states (Indiana, New Jersey, and Wyoming) require all persons to report and do not enumerate specific professions as mandated reporters.
Individuals designated as mandatory reporters typically have frequent contact with children. The professionals most commonly mandated to report across the states include the following:
- Social workers
- Teachers, principals, and other school personnel
- Physicians, nurses, and other healthcare workers
- Counselors, therapists, and other mental health professionals
- Childcare providers
- Medical examiners or coroners
- Law enforcement officers
It is important that all professionals be informed of the laws that pertain to the jurisdiction of their own practice (CWIG, 2023).
What Situations Require That a Report Be Made?
State statutes vary, but generally a mandatory reporter must make a report when they suspect or have reasonable cause to believe that a child is abused or neglected. The reporter does not have to provide proof of the suspected abuse or neglect (CWIG, 2023).
REASONABLE CAUSE
There can be “reasonable cause” to suspect that a child is abused or maltreated if, considering the physical evidence observed or information that had been disclosed and based on the reporter’s own training and experience, it is possible that the injury or condition was caused by neglect or by nonaccidental means.
Certainty is not required. The reporter need not be certain that the injury or condition was caused by neglect or by nonaccidental means. The reporter need only be able to entertain the possibility that it could have been neglect or nonaccidental in order to possess the necessary “reasonable cause.” It is enough for the mandated reporter to distrust or doubt what is personally observed or information that had been disclosed to the reporter about the injury or condition.
In child abuse cases, many factors can and should be considered in the formation of that doubt or distrust. Physical and behavioral indicators may also help form a reasonable basis of suspicion. Although these indicators are not diagnostic criteria of child abuse, neglect, or maltreatment, they illustrate important patterns that may be recorded in the written report when relevant.
How Is a Report Made?
In most jurisdictions, a telephone report must be made immediately, often followed by a written report. States may provide standardized forms for this purpose, and many jurisdictions offer electronic reporting.
Most healthcare facilities also have policies and procedures in place regarding the reporting of suspected child abuse. Healthcare professionals and other mandatory reporters must know what guidelines are in place at their place of employment as well as state mandates.
At the time of an oral telephone report, frequently to a state-subsidized 800 number, a child protective services (CPS) specialist will typically request the following information:
- The condition of the child
- Names and addresses of the child and parents or other person responsible for care
- Location of the child at the time of the report
- Child’s age, gender, and race
- Nature and extent of the child’s injuries, abuse, or maltreatment, including any evidence of prior injuries, abuse, or maltreatment to the child or their siblings
- Name of the person or persons suspected to be responsible for causing the injury, abuse, or maltreatment (“subject of the report”)
- Family composition
- Any special needs or medications
- Whether an interpreter is needed
- Source of the report
- Person making the report and where reachable
- Actions taken by the reporting source, including taking of photographs or X-rays, removal or keeping of the child, or notifying the medical examiner or coroner
- Any additional information that may be helpful
A reporter is not required to know all of the above information in making a report; therefore, lack of complete information does not prohibit a person from reporting. However, information necessary to locate a child is crucial to ensuring the child’s safety.
Consequences for Failing to Report
Nearly every state imposes a penalty of a fine or incarceration for mandated reporters who willfully do not report suspected child abuse or neglect. Such mandated reporters may be charged with a misdemeanor or felony for the failure to report. In several states, mandated reporters can also be held liable by civil statutes for damages that result from their failure to report (CWIG, 2019).
Perhaps more importantly, failure to report can lead to more serious consequences for the child and family. CPS cannot act until child abuse is identified and reported—that is, services cannot be offered to the family nor can the child be protected from further suffering.
REDUCING IMPLICIT BIAS IN REPORTING
Research shows that bias can contribute to a lower threshold to suspect child abuse in Black children and adolescents and a higher threshold for White children and adolescents (Jackson, 2024). Therefore, it is important for professionals to be aware of the potential for implicit biases and to ensure that such biases do not impact their decision-making. Instead, decisions must be made based on the objective facts of a situation.
A proven strategy to reduce bias and increase awareness regarding one’s own beliefs is to ask oneself the question, would I make a different decision about reporting if the child or family in a situation of suspected child maltreatment or abuse were of a different:
- Race?
- Ethnicity?
- Gender?
- Gender identity?
- Sexual orientation or expression?
- Religion?
- Immigration status?
- Primary spoken language?
- Culture?
- Age?
- Neighborhood where they reside?
- Presence of a disability?
- Occupation?
- Socioeconomic status of the family?
If the answer is yes, bias may be impacting one’s decision to make a report.
Another strategy when assessing information received about a child and their family is to ask analytical and evaluative questions and use critical thinking. This includes:
- Identifying the specific concerns about the current situation
- Gathering adequate information about the current situation
- Analyzing that information to separate facts from assumptions
- Recognizing the possibility of bias in one’s personal opinions
- Developing multiple hypotheses that could explain the situation
- Determining whether making a report is legally required
- If not, determining whether an alternative option is better, such as connecting the individual or family to appropriate services in their community
(NYS OCFS, 2022)
CONCLUSION
Child abuse and neglect remains a serious problem across the country. Pediatric abusive head trauma is one of the most serious types of such abuse and the leading cause of death from injury in infants.
It is important for all healthcare professionals to be aware of the risk factors and signs and symptoms of AHT in the patients they care for, since a diagnosis depends on input from a multidisciplinary team. Any person suspecting this form of child abuse is required to report it immediately to the appropriate authorities.
Prevention education by healthcare professionals serves the important goal of reducing all child abuse and neglect, including abusive head trauma. Patients can be further directed to various resources to help prevent the behaviors that lead to AHT.
RESOURCES
Child Welfare Information Gateway
FRIENDS (Family Resource Information, Education, and Network Development Service)
Fussy Baby Network (Erikson Institute)
Infant Early Childhood Mental Health (IECMH) Guiding Principles (Zero to Three)
National Center on Shaken Baby Syndrome
Responding to Child Maltreatment: A Clinical Handbook for Health Professionals (World Health Organization)
REFERENCES
NOTE: Complete URLs for references retrieved from online sources are provided in the PDF of this course.
American Academy of Pediatrics (AAP). (2020). Policy statement: Abusive head trauma in infants and children. https://publications.aap.org
American College of Radiology (ACR). (2021). ACR-SPR practice parameter for the performance and interpretation of skeletal surveys in children. https://www.acr.org
American Heart Association (AHA). (2020). Part 4: Pediatric basic and advanced life support. https://cpr.heart.org
Araki T, Yokota H, & Morita A. (2017). Pediatric traumatic brain injury: Characteristic features, diagnosis, and management. Neurol Med Chir (Tokyo), 57(2), 82–93.
Berthold O, Fegert JM, Brähler E, Jud A, & Clemens V. (2024). Abusive head trauma: The body of the iceberg—A population-based survey on prevalence and perpetrators. Child Abuse & Neglect, 149, Article 106660. https://doi.org/10.1016/j.chiabu.2024.106660
Brainline.org. (n.d.). What is the Glasgow coma scale? http://www.brainline.org
California Evidence-Based Clearinghouse for Child Welfare (CEBC). (2025a). Home visiting programs for prevention of child abuse and neglect. http://www.cebc4cw.org
California Evidence-Based Clearinghouse for Child Welfare (CEBC). (2025b). Prevention of child abuse and neglect (primary) programs. http://www.cebc4cw.org
California Evidence-Based Clearinghouse for Child Welfare (CEBC). (2025c). Prevention of child abuse and neglect (secondary) programs. http://www.cebc4cw.org
California Evidence-Based Clearinghouse for Child Welfare (CEBC). (2023). SafeCare. https://www.cebc4cw.org
Capacity Building Center for States (CBCS). (2021). Working across the prevention continuum to strengthen families. Children’s Bureau, Administration for Children and Families, U.S. Department of Health and Human Services. https://capacity.childwelfare.gov
Centers for Disease Control and Prevention (CDC). (2024a). About abusive head trauma. https://www.cdc.gov
Centers for Disease Control and Prevention (CDC). (2024b). Risk and protective factors. https://www.cdc.gov
Centers for Disease Control and Prevention (CDC). (2024c). Adverse childhood experiences. https://www.cdc.gov
Child Welfare Information Gateway (CWIG). (2023). Mandatory reporting of child abuse and neglect. U.S. Department of Health and Human Services, Administration for Children and Families, Children’s Bureau. https://www.childwelfare.gov
Child Welfare Information Gateway (CWIG). (2020). Protective factors approaches in child welfare. U.S. Department of Health and Human Services, Administration for Children and Families, Children’s Bureau. https://www.childwelfare.gov
Child Welfare Information Gateway (CWIG). (2019). Penalties for failure to report and false reporting of child abuse and neglect. U.S. Department of Health and Human Services, Children’s Bureau. https://www.childwelfare.gov
Child Welfare Information Gateway (CWIG). (n.d.). Prevention continuum. https://www.childwelfare.gov
Children’s Bureau. (2024). Child maltreatment 2022. U.S. Department of Health and Human Services (USDHHS), Administration for Children and Families, Administration on Children, Youth and Families. https://www.acf.hhs.gov
Choudhary AK, Servaes S, Slovis TL, Palusci VJ, Hedlund GL, Narang SK, Moreno JA, et al. (2018). Consensus statement on abusive head trauma in infants and young children. Pediatric Radiology, 48(8), 1048–65. https://doi.org/10.1007/s00247-018-4149-1
Christian CW. (2015). The evaluation of suspected child physical abuse. Pediatrics, 135(5), e1337–54. https://pubmed.ncbi.nlm.nih.gov
Christian CW & Levin AV. (2018). American Academy of Pediatrics clinical report: The eye examination in the evaluation of child abuse. Pediatrics, 142(2), Article e20181411. https://doi.org/10.1542/peds.2018-1411
Colloff P. (2024, December 29). He dialed 911 to save his baby. Then his children were taken away. New York Times. https://www.nytimes.com
Dias MS, Cappos KM, Rottmund CM, Reed ME, Smith KM, deGuehery KA, & Wang M. (2021). Preventing abusive head trauma: Can educating parents reduce the incidence? Pediatric radiology, 51(6), 1093–6. https://doi.org/10.1007/s00247-020-04819-6
Durber CM, Yeates KO, Taylor HG, Walz NC, Stancin T, & Wade SL. (2017). Family environment predicts long-term academic achievement and classroom behavior following traumatic brain injury in early childhood. Neuropsychology, 31(5), 499–507. https://www.ncbi.nlm.nih.gov
Feld K, Ricken T, Feld D, Helmus J, Hahnemann M, Schenkl S, Muggenthaler H, et al. (2021). Fractures and skin lesions in pediatric abusive head trauma: A forensic multi center study. International Journal of Legal Medicine, 136(2), 591–601. https://link.springer.com
Haney S, Scherl S, DeMeglio L, Perez-Rossell J, Servaes S, Merchant N, et al. (2025). Evaluating young children with fractures for child abuse: Clinical report. Pediatrics, 155(2), Article e2024070074. https://doi.org/10.1542/peds.2024-070074
Hart LC, Viswanathan M, & Nicholson WK. (2024). Evidence from the USPSTF and new approaches to evaluate interventions to prevent child maltreatment. JAMA Network Open, 7(7), Article e2420591. https://jamanetwork.com
Jackson AM. (2024). Unmasking racial and ethnic disparities in child physical abuse identification. JAMA Netw Open, 7(12), Article e2451546. https://doi.org/10.1001/jamanetworkopen.2024.51546
Kentucky Cabinet for Health and Family Services (KY CHFS). (2025). Health Access Nurturing Development Services (HANDS). https://www.chfs.ky.gov
Knipe H. (2020). Suspected physical abuse. Radiopaedia. https://radiopaedia.org
Laurent-Vannier A, Bernard JY, & Chevignard M. (2021). Abusive head trauma through shaking: Examination of the perpetrators according to dating of the traumatic event. Child Abuse Rev, 30, 283–99. https://onlinelibrary.wiley.com
Lennon JJ. (2024, May 2). The horrible truth about shaken baby syndrome cases. Slate. https://slate.com
Maiese A, Iannaccone F, Scatena A, Del Fante Z, Oliva A, Frati P, & Fineshci V. (2021). Pediatric abusive head trauma: A systematic review. Diagnostics (Basel), 11(4), Article 734. https://pubmed.ncbi.nlm.nih.gov
National Center on Shaken Baby Syndrome (NCSBS). (n.d.-a). Learn more. https://www.dontshake.org
National Center on Shaken Baby Syndrome (NCSBS). (n.d.-b). Period of PURPLE crying. https://www.dontshake.org
National Child Traumatic Stress Network (NCTSN). (n.d.). Secondary traumatic stress. https://www.nctsn.org
New York State Office of Children and Family Services (NYS OCFS). (2022). 2022 NYS mandated reporter training syllabus.
Nurse-Family Partnership (NFP). (2023). Nurse-Family Partnership overview. https://www.nursefamilypartnership.org
O’Meara A, Sequeira J, & Ferguson N. (2020). Advances and future directions of diagnosis and management of pediatric abusive head trauma: A review of the literature. Frontiers in Neurology, 11. https://www.frontiersin.org
Pediatric Brain Injury Research Network. (2025). Evidence-based medical screening for pediatric abusive head trauma (AHT). https://www.pedibirn.com
Pfeiffer H, Cowley LE, Kemp AM, Dalziel SR, Smith A, Cheek JA, Borland ML, et al. (2020). Validation of the PredAHT-2 prediction tool for abusive head trauma. Emerg Med J, 37(3), 119–26. https://doi.org/10.1136/emermed-2019-208893
Pierce MC, Kaczor K, Lorenz DJ, et al. (2021). Validation of a clinical decision rule to predict abuse in young children based on bruising characteristics. JAMA Network Open, 4(4), Article e215832. https://doi.org/10.1001/jamanetworkopen.2021.5832
Rabbitt A, Kelly TG, Yan K, Zhang J, Bretl DA, & Quijano CV. (2020). Characteristics associated with spine injury on magnetic resonance imaging in children evaluated for AHT. Pediatric Radiology, 50(1), 83–97. https://www.ncbi.nlm.nih.gov
Schermerhorn S, Muensterer OJ, & Ignacio RC, Jr. (2024). Identification and evaluation of non-accidential trauma in the pediatric population: A clinical review. Children (Basel), 11(4), 413. https://pmc.ncbi.nlm.nih.gov
Shahraki K & Suh D. (2024). An update to biomechanical and biochemical principles of retinal injury in child abuse. Children, 11, 586. https://doi.org/10.3390/children11050586
Slingsby B, Bachim A, Leslie LK, & Moffatt ME. (2024). Child health needs and the child abuse pediatric workforce. Pediatrics, 153(Supplement 2), Article e2023063678F. https://doi.org/10.1542/peds.2023-063678F
Stirling J, Gavril A, Brennan B, Sege RD, Dubowitz H, American Academy of Pediatrics, Council on Child Abuse and Neglect. (2024). The pediatrician’s role in preventing child maltreatment: Clinical report. Pediatrics, 154(2), Article e2024067608. https://publications.aap.org
Tanis JM, Klein SM, & Boyke H. (2024). State paid family leave policies and infant maltreatment. Child Abuse & Neglect, 152, 106758. https://pubmed.ncbi.nlm.nih.gov
Tibballs J & Bhatia N. (2024). Medical and legal uncertainties and controversies in “shaken baby syndrome” or infant “abusive head trauma.” J Law Med, 31(1), 151–84. https://pubmed.ncbi.nlm.nih.gov
Verive M. (2023). Pediatric head trauma practice essentials. Medscape. https://emedicine.medscape.com
Waters-Tozier S. (2020). Cultural practices and values that can masquerade as child abuse: A literature review and recommendations for the forensic psychologist. Journal of Forensic Psychology, 5(2). https://www.walshmedicalmedia.com
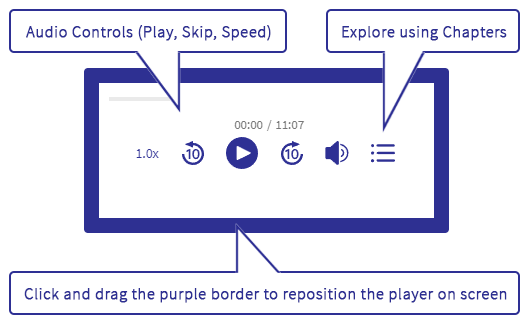






Customer Rating
4.9 / 173 ratings