By Krystle Maynard, DNP, MSN, RN, SANE-A
Nursing is one of the most challenging and rewarding career paths. But working as a nurse can be exhausting due to understaffing, long working hours, and being overworked. Burnout and compassion fatigue are on the rise among nurses. To address this issue, it’s important to provide nurses with adequate resources to manage their mental health and stress levels. How can we help ease the burden on nurses in healthcare?
Nurses are the backbone of the healthcare team. They entered the profession wanting to help people. Though this motivation remains their driving force, nurses need support, better staffing, and more resources to be their best and to provide the best care to patients and their loved ones.
Staffing Ratios
Nurses are pivotal in providing safe, quality patient care. While primary care providers are responsible for making medical diagnoses and treatment decisions, their time with each patient is substantially limited. It’s the bedside nurse who most often performs physical assessments, administers medications, monitors vital signs and lab results, identifies symptoms of deterioration, and more. In this way, nurses are central to all patient care.
The ability to detect early signs of patient deterioration is only one of the nursing roles that can be severely impacted by inadequate staffing. Despite countless studies demonstrating the direct correlation between inadequate staffing ratios and increased patient safety events, errors, and mortality and morbidity rates, only two states have adopted mandated nurse-to-patient ratios. According to the American Nurses Association, only 16 total states address nurse staffing in some capacity through laws and regulations.

For many nurses, being assigned a large number of patients can easily lead to stress and anxiety as they envision a long day of running nonstop from patient to patient with no time for a break and barely enough time to document. Under such conditions, patient care can easily suffer.
Patient-Related Workload and Acuity
Mandated nurse-to-patient ratios are a goal worth fighting for, but nurses and healthcare allies cannot stop there. Ratios may limit the number of patients a nurse is responsible for, but another factor that must be considered is patient-related workload and acuity.
Research shows that many factors must be used to determine a patient’s acuity and the nursing time required to care for that patient. Such indicators include vital signs to be monitored (and their frequency), respiratory and cardiac assessment, fluid volume status, acid-base balance, oxygenation, drains/lines/tubes, complex wound management, isolation, mental status, communication barriers, and much more.
Each patient has varying degrees of disease complexity and, thus, may require different degrees of time and attention by each nurse. Imagine a nurse with five patients in a busy medical-surgical unit, each at a different acuity level and requiring a different workload.
Such high patient workloads are a common occurrence in healthcare, with a typical assignment on a medical-surgical unit being 4-6 patients per nurse. For each patient, the nurse must complete the following tasks each shift:
- Perform thorough physical assessments
- Administer all scheduled and PRN medications promptly
- Research and understand medication side effects and specifics necessary to ensure patient safety
- Monitor and trend all vital signs
- Monitor and trend all labs
- Recognize and report critical findings and changes
- Address each patient need and request
- Communicate and collaborate with interdisciplinary team members
- Document everything
When the expectation is that nurses are to round on each patient, it can be a real challenge to perform all these duties and ensure patient safety.
Effects of Short-Staffed Nursing Care

Part of acknowledging the need for safer ratios and more balanced workloads is understanding the implications on patient care due to inadequate staffing. This is a problem that impacts nurses, patients, and healthcare facilities alike.
What can occur as a result of inadequate staffing?
- Delayed medication administration: When nurses must care for multiple patients with varying acuities and workload demands, it may not be possible for the nurse to reach each patient promptly to administer scheduled medications.
- Improper documentation: Nurses are expected to round and document each patient every 2 hours. More often than not, this is physically impossible, yet nurses may face disciplinary action if all tasks are not documented and/or performed.
- Unfinished tasks: Nurses often have a seemingly never-ending task list for each patient, and as much as they try, it may be impossible to accomplish everything. This may lead to leaving some tasks undone by the time the next shift begins.
- Unmet patient needs: Patients have many needs and requests each day. And aside from all the nursing-related activities, patients frequently need to be bathed and repositioned, receive PRN medications, undergo spirometry and/or lab testing, engage in physical activity, receive wound care, etc. For instance, one primary task that gets pushed to the side is regular patient ambulation. Nurses know that this is vital to the patient’s recovery, but there may not physically be enough hands or resources to carry out all these task as often as indicated.
- Increased patient safety occurrences: When a facility is short-staffed, nurses cannot answer call lights as frequently or as timely as needed, leaving patients at risk. For instance, a patient who needs assistance with toileting may press their call light, but if every staff member is busy with other patients, this poses a real challenge. The patient is forced to decide either to “hold it” or to get to the toilet themselves, which can often result in a fall. Similarly, in patients with mobility issues, it can be difficult to turn and reposition them every two hours.
Nursing Hours
Twelve hours is a long time, but it is the average nursing shift length. When factoring in commute time, incoming and off-going nurse reports, and the occasional emergency at shift change, the work day often ends up being 13–14 hours long.
Truthfully, there are pros and cons to such long days. Long shifts for nurses equate to working fewer days per week, which can be a huge selling point for nurses. As hard as their days may be, the job can be easier to manage when nurses only have to work three days a week.
But there is often discussion surrounding these 12-hour shifts and whether they positively or negatively impact job satisfaction and nursing shortages. Should healthcare change and require nurses to return to shorter shifts, there may be some resistance. On the plus side, the stresses felt each day as a nurse may take less of a toll on each nurse if they worked shorter shifts. The downside is that they would have to work more of them.
Case Scenario
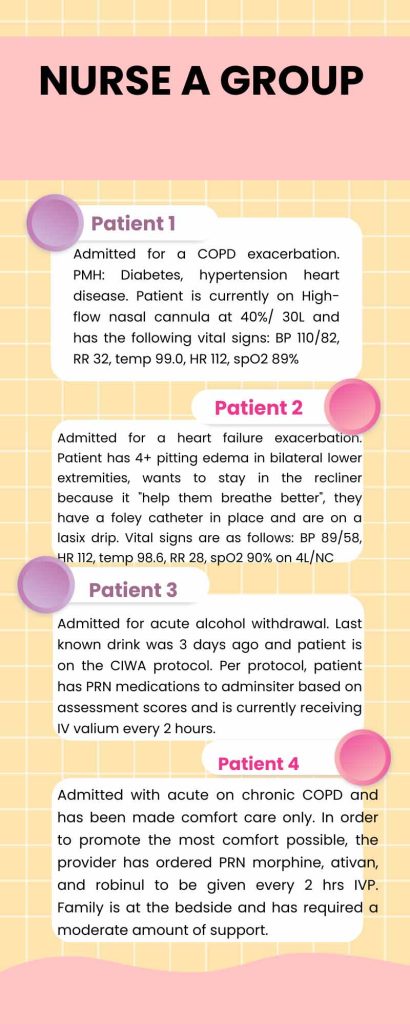
Nurse A arrives at work to realize they have been floated to another unit for the day. The nurse travels to the unit and discovers the group assignment below. Some may consider four patients a blessing, considering the patient load could be much higher. However, as the nurse reviews the anticipated workload of the patient group, they grow stressed and anxious. The nurse envisions having a day full of running nonstop, no break, and barely having time to document. If too much time is spent in one room, another patient has the potential to decline, and early warning signs may be missed.
Final Thoughts

Providing quality healthcare is continually a challenge to providers, staff, and patients. Nurses and patients sometimes suffer in high-stress environments with less-than-optimal staffing, demanding workloads, and long hours. Being a nurse is hard work, as they strive to provide safe and adequate care to their patients.
Sign up for our newsletter email list and like us on Facebook and Instagram to be among the first to know about all our special discounts and offers!
About Wild Iris Medical Education:
Wild Iris Medical Education, Inc., is a privately held, woman-owned company providing online healthcare continuing education. In 1998, we began offering online ANCC-accredited nursing continuing education courses and since then have expanded to provide CEUs for occupational therapists, physical therapists, paramedics, EMTs, and other healthcare professionals.
Accredited and Approved Nationwide.
High-quality CEU Courses since 1998.

Join Our More Than 750,000 Satisfied Customers Now!
High-quality, accredited, evidenced-based continuing education courses in an easy-to-use format designed for learning, from Wild Iris Medical Education. We’ve been providing online CE since 1998.



