Assessment, Treatment, and Management: Suicide Prevention Training Program for Washington Healthcare Professionals (6 Hours)
Online Continuing Education Course

Course Description
6-hour mandatory suicide prevention training for Washington. The following professions are required to take six hours on suicide assessment, treatment, and management: social workers, licensed mental health professionals, nurses, marriage and family therapists, naturopaths, osteopathic physicians/surgeons/physician assistants, physicians and physician assistants, psychologists, and retired active licensees of the above professions. Wild Iris Medical Education, Inc.'s training approval number is TRNG.TG.60722274-SUIC. This course is also approved for pharmacists.
If you are in a crisis, call or text 988, call 911, or go to the nearest emergency room.
Course Price: $60.00
Contact Hours: 6
Course updated on
October 3, 2025
"This course provided new information and interventions that I had not previously known. This topic is not an 'easy' one in practice, yet the overall presentation of the topic was easy to follow and comprehend." - Nancy, RN in Washington
"This is a well-integrated educational piece. I found it very useful, with content worth keeping on hand." - Geralyn, RN in Washington
"Very good and current reference information." - Robin, RN in Washington
"Surprisingly good, well-written information." - Michael, MD in Washington
Assessment, Treatment, and Management: Suicide Prevention Training Program for Washington Healthcare Professionals (6 Hours)
Copyright © 2025 Wild Iris Medical Education, Inc. All Rights Reserved.
LEARNING OUTCOME AND OBJECTIVES: Upon completion of this continuing education course, you will demonstrate an understanding of the complex nature of suicide, how to assess and determine risk for suicide, and appropriate treatment and management for at-risk individuals. Specific learning objectives to address potential knowledge gaps include:
- Review the language and common beliefs regarding suicide.
- Discuss the epidemiology and etiology of suicidal behavior.
- Summarize the risk and protective factors for suicide.
- Describe the process of assessment and determination of level of risk for suicide.
- Outline the management and treatment modalities that may be used for persons at risk for suicide.
- Identify public health approaches for suicide prevention.
- Discuss ethical dilemmas that arise in relation to suicide prevention and intervention efforts.
TABLE OF CONTENTS
- Understanding Suicide
- Epidemiology
- Suicide Etiology and Risk Factors
- Suicide Screening and Assessment
- Models of Care for Patients at Risk for Suicide
- Management of the Patient at Risk for Suicide
- Treatment Modalities for Patients at Risk for Suicide
- Suicide Prevention Strategies
- Ethical Issues and Suicide
- Conclusion
- Resources
- References
UNDERSTANDING SUICIDE
Suicide, the taking of one’s own life, has been the subject of deliberation throughout history, and making a judgment about whether life is or is not worth living is a question that underlies philosophical thought. Suicide is always controversial, raising questions of rationality and morality. Depending on one’s philosophical point of view, it is either acceptable at any time, acceptable under certain circumstances, or never acceptable.
The will to live arises from instinctual self-preservation, and it takes a great deal of willpower to overcome this natural instinct. Humans are motivated by the pursuit of pleasure and the avoidance of pain, and suicide is usually prompted by a desire to be rid of unbearable pain or distress, which can be ended by an impulsive act. Suicide is the culmination of many and varied interactions between biological, social, and psychological factors that operate at the levels of the individual, the community, and society.
Healthcare professionals play a critical role in the recognition, prevention, and treatment of suicidal behaviors, and the attitudes of these providers are paramount in how patients are treated. Historically, the stigma associated with suicide affects the attitudes of those who manage and treat these individuals.
Talk of suicide must always be taken seriously, recognizing that people with suicidal ideation are in physical and/or psychological pain and may have a treatable mental disorder. The vast majority of people who talk of suicide do not really want to die. They simply are in pain and want it to stop. Suicide is an attempt to solve this problem of intense pain when problem-solving skills are impaired in some manner, in particular by depression.
Many healthcare professionals express concern that they are ill prepared to deal effectively with a patient has suicidal thoughts. By developing adequate knowledge and skills, these professionals can overcome feelings of inadequacy that may otherwise prevent them from effectively responding to the suicide clues a patient may be sending, thereby allowing them to carry out appropriate interventions. They can also develop a better understanding of this choice that ends all choices.
Changing the Language
The term committed suicide suggests that a person was involved in a criminal act. It implies that the person was a perpetrator and not a victim of a pathology that led to death. It ignores the fact that suicide is often the consequence of an unaddressed illness, such as depression, and it perpetuates a harmful stigma. It also implies that suicide is an act of free will, a choice one makes to live or die.
There is a great deal of evidence indicating that thought processes are gravely impaired at the time of death by the effects of trauma, mental health conditions, or substance use, and many have reported experiencing something akin to command hallucinations right before attempting to kill themselves. So, if a person cannot rationally choose due to impairment of the mind, the decision is not a choice.
Stigma surrounding mental illness, and suicidality in particular, has been documented as an immediate and profound barrier to help-seeking behavior. The following table provides recommendations for changing the language that surrounds the topic of suicide in order to remove the harmful stigma that can profoundly affect both the person with suicidal thoughts or behaviors and those closest to them.
| Inappropriate | Appropriate | Why |
|---|---|---|
| (Canadian Psychiatric Association, 2022) | ||
| Commit/committed suicide |
|
“Commit” implies suicide is a sin or a crime, reinforcing stigma. |
|
|
|
|
<Name> has suicidal thoughts or behavior/is thinking of suicide/has experienced suicidal thoughts | Avoids defining someone by their experience with suicide; a person is more than their suicidal thoughts. |
| Manipulative, suicidal gesture, cry for help | Describe the behavior (e.g., nonsuicidal self-injury) | Avoids dismissive labeling |
LEXICON OF SUICIDAL BEHAVIOR
Aborted attempt
An act in which a person initiates a suicidal act but stops before sustaining any injury
Cluster suicides
A group of suicides or suicide attempts, or both, that occurs closer together in time and space than would normally be expected in a given community
Contagion
Suicide risk associated with the knowledge of another person’s suicidal behavior, either firsthand or through the media
Copicide, death-by-cop, suicide-by-cop, officer-assisted suicide
Acting in a threatening way so as to provoke a lethal response by a police officer
Copycat suicide
A suicide that may be at least partially caused by contagion
Euthanasia
From the Greek, meaning “good death”; the intentional causing of a death, usually in an incurably or terminally ill individual, to relieve pain or suffering; a mercy killing
Interrupted suicide attempt
When an individual is stopped by an outside force (person or circumstance) before making an attempt
Mass suicide
The deliberate ending of the lives of all or most of the members of an intact social group or aggregate by the members themselves, either directly through self-injurious behavior or indirectly by choosing a course of action that will likely be fatal
Murder-suicide
When a person kills another person(s) and then kills themself
Non-suicidal self-injury
Deliberate, direct destruction or alteration of body tissue without a conscious suicidal intent, such as cutting, burning, or bruising oneself
Obligatory suicide
A suicide completed because the victim felt a personal duty to perform the act to honor the family, a cause, or a nation (e.g., Japanese kamikaze pilots)
Preparatory suicidal behavior
Activities such as assembling pills, buying a gun, attaching a rope, or visiting a bridge in preparation for suicide, but without initiating suicide
Suicide
Death caused by self-directed injurious behavior with evidence, either implicit or explicit, of intent to die as a result of the behavior
Suicide attempt
Any non-fatal potentially injurious behavior with intent to end one’s life
Suicide attack
A violent terrorist act in which the attacker intends to kill others or cause destruction expecting to die in the process, such as suicide bombers
Suicide contagion
Exposure to suicide or suicidal behavior within one’s family, one’s peer group, or through media reports that can result in suicide and suicidal behaviors (copycat)
Suicidal ideation
Thinking about dying by suicide
Suicide pact
An agreement between two or more individuals to die by suicide at the same time and/or place
(APA, 2022)
Suicide Myths and Misunderstandings
Myths and misunderstandings abound concerning the subject of suicide. In order for a provider to be effective in intervening with a person who has suicidal thoughts, these myths and misunderstandings must be replaced with facts. Following are ten common myths and associated facts:
| Myth | Fact |
|---|---|
| (Sharma, 2021; Samaritans, 2022) | |
| People who talk about suicide are seeking attention, aren’t serious, and won’t go through with it. Attempted suicides are often not seen as genuine efforts to end one’s life but as a way to manipulate other people into paying attention to them. | People who talk about suicide may be reaching out for help or support. They are looking for an escape and are unable to think of any other way than through death, and they do indeed, need attention. The majority of people who feel suicidal do not actually want to die; they just want the situation they’re in or the way they’re feeling to end. |
| Once a person has made a serious suicide attempt, that person is unlikely to make another. | The opposite is often true. A prior suicide attempt is the single most important risk factor for suicide in the general population. |
| People who attempt or die by suicide are selfish, cowardly, or weak. | Suicide is seldom about others. Indeed, it is selfish to make someone else’s suicide about you and demonstrates a lack of empathy and compassion for others. To overcome the instinct to live, one must be strong, not weak or cowardly. |
| All people with suicidal thoughts have access to help if they want it, but those who die by suicide do not reach out for help. | The truth is, it is necessary to ask whether the individual was able to ask for help. Many seek support and help but do not find it. This is often due to negative stereotyping and the inability and unwillingness of people to talk about suicide. Financial barriers may include lack of access to help, especially for those in rural areas who might not be able to easily travel to another community to seek help. Additionally, prejudices and biases among healthcare professionals can make the healthcare system unfriendly. |
| Only people who are crazy or have a mental disorder consider suicide. | One in five people have thought about suicide at some time in their life. Many people living with mental disorders are not affected by suicidal behavior, and not all people who die by suicide have a mental disorder. They may be upset, grief-stricken, depressed, or despairing, but extreme distress and emotional pain are not necessarily signs of mental illness. |
| Reaching out for help is the same as threatening suicide. | People with suicidal thoughts are hurting, not threatening, and should be provided with the tools, support, and resources they need. |
| Suicide always occurs without any warning signs. | There are almost always warning signs, such as saying things like “everyone would be better off if I wasn’t here anymore.” |
| Once people decide to die by suicide, there is nothing you can do to prevent it. | Suicide is preventable. Most people who with suicidal thoughts are ambivalent about living or dying. Most do not want death but simply want to stop hurting. Often, feeling actively suicidal is temporary. The impulse to “end it all,” however overpowering, does not last forever and can be overcome with help. |
| If you ask a person whether they are thinking about suicide or have chosen a method, it can be interpreted as encouragement or give them the idea. | Evidence shows that asking someone if they’re having suicidal thoughts can be protective by giving them permission to talk about how they feel. |
| When people with suicidal thoughts start to feel better, they are no longer suicidal. | A person with suicidal thoughts sometimes begins to feel better because they have reached the decision to die by suicide and may have feelings of relief that their pain will soon be over. |
EPIDEMIOLOGY
Suicide Globally
The World Health Organization reported in 2025 that an estimated 720,000 people die annually around the globe due to suicide. Suicide was the third leading cause of death among 15- to 29-year-olds in 2021. The five countries with the highest suicide rates per 100,000 population in 2021 were Greenland (59.6), Guyana (31.3), Lithuania (27.9), South Korea (25.8), and Russia (24.1) (WHO, 2025; World Population Review, 2022)
Suicide in the United States
In the United States, over 49,000 people died by suicide in 2023, or one death every 11 minutes. Among adults, 12.8 million seriously thought about suicide, 3.7 million made a plan for suicide, and 1.5 million attempted suicide. In 2022, suicide was the 11th leading cause of death for all ages in the United States (CDC, 2025b).
Some populations experience more negative social conditions and have higher rates of suicide or suicide attempts than the general U.S. population. The excess burden of suicide in some populations are called health disparities. Examples of groups experiencing suicide health disparities include veterans, people who live in rural areas, sexual minorities, middle-aged adults, people of color, and tribal populations (CDC, 2025c).
By geography: The highest suicide rate in 2023 was in Alaska (28.15 per 100,000), and the lowest rate was in Washington, DC (5.75 per 100,000) (CDC, 2025a).
By race/ethnicity: Groups with the highest rates in 2023 were non-Hispanic American Indian and Alaska Native people and non-Hispanic White people.
| Race/ethnicity | Age-adjusted rate per 100,000 population |
|---|---|
| (CDC, 2025b) | |
| Non-Hispanic American Indian/Alaska Native | 23.8 |
| Non-Hispanic White | 17.6 |
| Non-Hispanic Native Hawaiian/Other Pacific Islander | 17.3 |
| Non-Hispanic Multiracial | 9.2 |
| Non-Hispanic Black | 9.1 |
| Hispanic | 8.2 |
| Non-Hispanic Asian | 6.5 |
By sex: The suicide rate among males in 2023 (22.7 per 100,000 population) was approximately four times higher than the rate among females (5.9 per 100,000 population). Males make up 50% of the population but nearly 80% of suicides (CDC, 2025b). Data indicate that 82% of transgender individuals have considered killing themselves and 40% have attempted suicide, with suicidality highest among transgender youth (Austin et al., 2022).
By age: Adults ages 35–64 years account for 46.8% of all suicides in the United States, and suicide is the 8th leading cause of death for this age group. When measured by age, all people 85 years and older had the highest rates of suicide in 2023. When also factoring in sex, men ages 75 and older had the highest rate (42.2 per 100,000) compared to other age groups among men. Non-Hispanic White men have the highest suicide rate compared to other racial/ethnic men in the 75+ age group (50.1 per 100,000).
The suicide rate for youth and young adults ages 10–24 years (11.0 per 100,000) is lower than other age groups. However, suicide is the second leading cause of death for this age group. In 2021, 9% of high school students reported attempting suicide during the previous 12 months. Suicide attempts were reported most frequently among girls compared to boys (12.4% vs. 5.3%) and among non-Hispanic American Indian or Alaska Native students (20.1%) (CDC, 2025c).
Among sexual minorities: Data are limited on frequency of suicide among people who identify as sexual minorities. However, research shows that high school students who identify as sexual minorities have a higher prevalence of suicide attempts compared to heterosexual students. In 2021, more than a quarter (26.3%) of high school students identifying as lesbian, gay, or bisexual reported attempting suicide in the prior 12 months. This was five times higher than the prevalence among heterosexual students (5.2%). Data from 2020 show the prevalence of individuals reporting suicide attempts in the prior 12 months among adult sexual minorities decreased with age, from 5.5% among people ages 18-25 to 2.2% among people ages 26-49.
Among U.S. Veterans and Active-Duty Military: In 2024, 472 service members died by suicide: 304 active-duty personnel, 63 reserve, and 105 national guard (U.S. DOD, 2025). In 2022, the suicide rate among U.S. veterans was 34.7 per 100,000 and totaled 6,407 (271 female and 6,136 male). Suicide was the 13th leading cause of death among veterans overall, and the second leading cause of death among veterans under age 45 (VA, 2024).
Suicide in Washington State
Suicide is a leading cause of death, particularly among young people, veterans, middle-aged men, and American Indian and Alaska Natives (AI/AN). Between 2018 and 2022, more than 1,200 Washington residents died by suicide each year, making it the eighth leading cause of death in the state. For nearly two decades, Washington’s suicide rate has consistently exceeded the national average. The economic and societal costs of suicide are also significant, estimated at over $12.8 billion annually in Washington alone (CDC, 2024).
By age: Suicide rates vary by age group. In 2022, suicide rates ranged from 1.75 per 100,000 among youth ages 10–14 years to 35.9 per 100,000 among people 85 years and older (WSDOH, 2025).
By race/ethnicity: Suicide rates by race and ethnicity point to additional disparities. Suicide rates ranged from 8.6 per 100,000 among non-Hispanic Asian populations to 22.0 per 100,000 among non-Hispanic American Indian and Alaska Native (AI/AN) populations. In 2022, 76% of suicides occurred among non-Hispanic White populations (WSDOH, 2025).
By sex: Suicide rates among females and males show large differences. In 2022, male age-adjusted suicide rates (23.6) were about four-fold higher than female rates (6.0) (WSDOH, 2025).
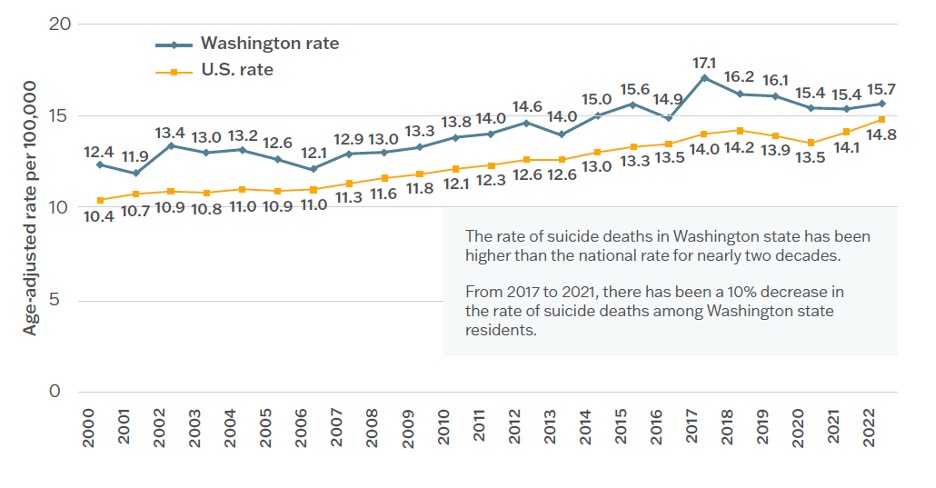
Age-adjusted suicide rates, 2000–2022, Washington and United States. (Source: WSDOH, 2025.)
SUICIDE ETIOLOGY AND RISK FACTORS
Suicide etiology and risk are complex and include family history, genetics, epigenetics, neurobiology, medication use, gender, mental health disorders, psycho-sociocultural factors, age, life experiences, and other considerations.
Family History and Genetics
One of the most prevalent risk factors for suicide is a family history that includes first- and second-degree biological relatives with histories of suicidal behaviors, as well as relatives with histories of neuropsychiatric conditions (Pollak, 2021).
In the largest genetic study of suicide attempts, a region of the genome on chromosome 7 containing four genes identified as heightening the risk of suicidal thoughts and actions. The study also found an overlap in the genetic basis of suicide attempts and related psychiatric disorders, especially major depression (Mount Sinai, 2021).
The gene with the strongest association with self-harm ideation is DCC, a protein coding gene involved in prefrontal cortex innervation and development. DCC has been linked to suicidal severity, and there is evidence of elevated DCC expression in the prefrontal cortex of post-mortem brains of those who died by suicide.
The estrogen receptor ESR1 has been identified as a causal genetic driver gene of posttraumatic stress disorder (PTSD) and depression, both of which increase the risk for suicide. Estrogen is suspected as a cause of gender differences in depression rates, and loss of ESR1 has been found to produce effects on brain tissue in men.
The dopamine receptor DRD2 has been found to be associated with suicide attempts, schizophrenia, mood disorders, ADHD, risky behaviors, and alcohol use disorder, all of which increase the risk for suicide.
Antisocial behavior, substance use, and ADHD are associated with TRAF3, a protein-coding gene, all of which increase the risk for suicidal behavior (Avery, 2022).
Epigenetics
Epigenetics refers to the impact of environmental influences on gene activity and expression. Epigenetic regulation of brain-derived neutrophic factor (BDNF), HPA axis components, and GABA-A receptors have all been found to be associated with the development of major depressive disorder and suicidal behavior. Also, in those who have died by suicide, researchers have found increased expression of DNA methyltransferase (DNMT)—the enzyme that methylates DNA in the frontal cortex—and total DNA hypermethylation in the Wernicke cortex and prefrontal cortex (Wislowska-Stanek et al., 2021).
Neurobiology
The core element of suicide etiopathogenesis is believed to be neuroinflammation. Inflammatory mediators play a critical role in the pathophysiology of suicide, and patients with suicidal ideation display elevated markers of inflammation in the central nervous system and peripheral tissues, irrespective of their primary diagnosis, age, and gender.
These mediators subsequently stimulate the kynurenine pathway, causing subsequent serotonin and melatonin depletion. Serotonin deficits are implicated in the pathogenesis of depression and also in aggression, impulsivity, suicidal ideations, and suicide attempts. Mood spectrum disorders, including major depressive disorder, are observed in those with dysregulation in secretion of melatonin (Conte Center Suicide Prevention, 2021; Offord, 2020).
Suicidal behaviors also are associated with hyperactivity of the hypothalamic-pituitary-adrenal (HPA) axis, which controls the release of the stress hormone cortisol and is known to be upregulated in clinical depression. Increased cortisol levels may cause disturbance in the control of stress, impaired function of the hippocampus, and significant defects. Adrenal gland cortical hypertrophy has been found in patients who died by suicide.
Imbalances in the level of the neurotransmitters glutamate and gamma-aminobutyric acid (GABA) in the central nervous system have been implicated in different neurological and psychiatric disorders, including major depressive disorder. Existing data demonstrate that glutamate may play an important role in suicide-related personality traits, including impulsivity and aggression. Gamma-aminobutyric acid (GABA) plays an important role in behavior, cognition, and the body’s response to stress.
The frontal and prefrontal cortex play an essential role in suicidal behavior through its involvement in cognition, stress response, and suppression of impulsiveness. Patients with a history of suicide attempts have altered prefrontal area activation, patterns that are associated with impaired decision-making, risk-reward, and social assessment. The anterior cingulate cortex, responsible for negative self-thinking and processing emotional stimuli, is strongly implicated in suicidality (Wislowska-Stanek et al., 2021).
Medications
Antidepressants have an important role in the treatment of mood disorders. In rare cases, they can induce or exacerbate suicidal tendencies during the first weeks of treatment, especially in children and adolescents. Some of the selective serotonin reuptake inhibitors (SSRIs) may increase suicidal behavior by stimulating depressed patients to act on preexisting suicidal thoughts. That is, as depression starts to lift, patients may feel less helpless but still depressed enough to decide that suicide is a way out. Before they were too immobilized, but now they are capable of making and carrying out a suicide plan.
Patients taking anticonvulsant drugs, such as gabapentin, tiagabine, and oxcarbazepine, have been found to have approximately double the risk of suicidal behavior or ideation as compared with patients receiving a placebo (Moutier, 2022; Levin et al., 2023).
Gender
The rate of completed suicide in men is higher than in women. However, attempted suicide is more common among women than men. Studies have found that the reason women are not as suicidal is that they often have more psychological support, they more easily decide to seek help, and they find it harder to fall into a state of social isolation. Explanations for this include biological gender changes, different ways of expressing aggression, and diversity in learning social and gender roles.
Marriage and children have been found to be protective factors for women, but not for men. But studies have also found that divorced and widowed women have a four to five times higher risk of suicide and that women without children are more likely to commit suicide than those with children (Samaritans, 2021).
Over the past decade, nearly 9% of females of childbearing age (15–44) who died by suicide were pregnant or recently postpartum. Mental health conditions and substance use disorders were common preceding circumstances. Among those with co-occurring behavioral health issues, such as anxiety, depression, bipolar disorder, or substance use disorders, the increase in rates of suicidality was significantly higher (Akkas, 2022).
Men react more strongly to changes in socioeconomic conditions, so that employment stress, income, and wealth have a greater impact on them. Higher mortality in men can also be explained partly by a greater propensity for violent behavior and a more frequent choice of the most effective means of death by suicide (Maloku & Maloku, 2020; Samaritans, 2021).
Mental Health Disorders and Suicide Risk
Three clinical groups have been identified to be at significant risk for suicidal behavior. These groups include patients with:
- Neurodevelopment disorders: Attention-deficit/hyperactivity disorder (ADHD), autism spectrum disorder, and specific learning disorders, all of which are highly associated with elevated rates of cognitive/neuropsychological impairment
- Neuropsychiatric disorders: Including, but not limited to, major depression, bipolar disorder, schizophrenia and related psychotic disorders, obsessive-compulsive disorder, posttraumatic stress disorder, and borderline personality disorder
- Acquired cognitive/neuropsychological impairment: Including impairment that results from a multiplicity of medical conditions, such as brain injury, brain neoplasm, central nervous system infection, cerebrovascular disease, seizure disorder, multiple sclerosis, neurodegenerative brain disease, and exposure to neurotoxins and an assortment of medications and substances
The patients who are among these three clinical groups experience challenges that negatively impact their psychosocial development, executive functioning, and quality of life. Additional difficulties can result from one or more components of negative affectivity, including irritability, lability, anxiety, and depression. In addition, a large number of patients who fall into one or more of these groups have a reduced ability to profit from experience, which can increase the risk for suicidal behaviors (Pollak, 2021).
Psycho-Sociocultural Factors
Psycho-sociocultural factors refer to a person’s ability to consciously or unconsciously interact with the social and cultural environment. They involve past experiences; the environment in which a person lives; relationships with and support from others; cultural norms; and cognitive abilities, intellect, personality, and other psychological factors that cause individuals to respond to their environment in a unique way. Such factors may be:
- Personality characteristics: May include, but are not limited to, paranoid personality features, histrionic and/or borderline personality features, obsessive-compulsive and dependent personality features, and impulsive or aggressive traits
- Developmental factors: May include substance use, cognitive deficits, behavioral disinhibition, and negative effects, which refer to the subjective experience of a group of negative emotional states such as anxiety, depression, stress, worry, guilt, shame, anger, and envy
- Interpsychic conflicts: A range of longstanding internalized psychological conflicts that contribute to a patient feeling emotionally trapped in response to certain stressors or triggers
- Psychological markers: Feelings of hopelessness, rage, anxiety, loneliness, and desperation
- Life experiences: Early-life adversity, history of trauma or abuse, and previous suicide attempt
- Environmental factors: May include job or financial loss, relational or social loss, stigma associated with help-seeking behavior, certain cultural and religious beliefs, barriers to accessing mental health care and substance abuse treatment, and exposure to the influence of others who have died by suicide, including media exposure
(Nevada DPBH, 2021; Garcia, et al. 2021)
BULLYING AND SUICIDE
There is a general consensus that exposure to bullying is associated with an increased risk for experiencing suicidal thoughts and behaviors. Additionally, those who are exposed to bullying behavior also engage in higher rates of self-harming behavior independent of the desire for suicide. Bullying victims are between two to nine times more likely to consider suicide than non-victims, and 10- to 14-year-old girls may be at an even higher risk for suicide. Nearly 30% of students are either bullies or victims of bullying.
Researchers have found that workplace bullies can drive their targets to suicide. Bullying in this setting is defined as harassment, badgering, and “freezing out” that occurs repeatedly over a period of time and involves two parties in which one has a higher ranking than the other.
Adults usually use verbal as opposed to physical bullying, with the goal to gain power over another person and be dominant. However, adults may also use physical abuse to reach this goal. Domestic violence is such an example, which often involves both verbal and physical bullying (MBF, 2023; Leach, et al., 2020).
SOCIOCULTURAL FACTORS
The degree to which a person’s surroundings exert a positive or negative influence on suicidal behavior depends on factors such as demographic characteristics, life stressors, coping skills, biological factors as well as whether an individual’s family, community, and country are supportive or stressful. Research has shown that social support can help prevent someone moving from suicidal ideation to suicide attempts.
Identity is inherently social, and a social network of relationships is an important part of and foundation for many people’s sense of self-esteem and self-efficacy. People with close relationships with others cope better with stressors and have better overall psychological and physical health. This can include a great array of relationships, such as spouses or life partners, parent-child, friend-friend, relative-relative, and fellow group members.
Social networks provide opportunities for emotional release and feeling a connection to others. Isolation, on the other hand, can lead to feelings of alienation and depression that may ultimately lead to suicidal thoughts and behaviors.
Social and cultural groups can be supportive and create feelings of belonging, love, and comfort, thereby serving as a “safety net” to catch those who are experiencing problems or stressors. Being a member of a highly integrated group often serves as a suicide deterrent.
Group membership, however, can sometimes require stress-inducing obligations and high levels of commitment, which can then lead to the adoption of behavioral and attitudinal norms, rather than thinking for oneself. These types of groups can feel repressive and stifling and may actually contribute to suicidal thoughts and feelings. In some instances, groups can even demand that someone die by suicide as an offering for the “greater good.”
A norm is a rule that is socially enforced, and a group, community, or nation promotes what is the norm regarding attitudes and behaviors. Social norms regarding suicide can influence whether or not it is stigmatized as well as its frequency. Many societies and religious traditions ban suicide and view it as sinful or taboo behavior. Others portray suicide as a legitimate behavior in certain circumstances.
Societies that are experiencing upheaval and unrest have higher rates of suicide. Social change that results in the breakdown of a culture’s traditional values can accompany a rise in suicide rates (Mental Help, 2023).
| Level of influence | Risk factors |
|---|---|
| (CDC, 2022e; Alvarez et al., 2022; Coimbra et al., 2022) | |
| Individual |
History of:
|
| Relationship |
Negative life events:
|
| Community |
Traumatic history:
|
| Society |
Negative stereotypes about:
|
(See also “Protective Factors” later in this course.)
Suicide Risk According to Age
Suicide occurs throughout the lifespan, affecting individuals in various age groups differently, and some have higher suicide rates than others.
CHILDREN AND ADOLESCENTS
Suicide is the second leading cause of death among U.S. children and adolescents ages 10–19 years, causing more deaths than any single major illness and second only to unintentional injuries (CHA, 2023). The number of children ages 5–11 who have died by suicide has increased significantly between 1999 and 2020, most of these being children between 10–11 years old and 75% being male. Younger children who die by suicide are more likely to be of above-average intelligence, which possibly exposes them to the developmental level of stress experienced by older children.
Puberty may have a negative impact, especially for girls. Girls who mature early have been found to be more likely to have a lifetime history of disruptive behavior disorder and suicide attempts than their peers.
During adolescence, abstract and complex thinking begin to develop, and these youth become more capable of contemplating life circumstances, envisioning a hopeless future, generating suicide as a possible solution, and planning and executing a suicide attempt.
During adolescence, the prevalence of depression increases and becomes twice as high among girls than boys, which explains some differences in rates of suicide between boys and girls. As puberty progresses, most boys develop a positive self-image, but girls, particularly White girls, have a diminished sense of self-worth.
After puberty, the rate of suicide increases with increasing age. Potential reasons for this include an increased access to firearms and potentially lethal drugs; increased rates of psychiatric illness, substance abuse, and other comorbidities; or a history of aggressive, impulsive conduct with a tendency to act out emotions in damaging ways.
The risk of suicide among children and adolescents is increased due to:
- Family tensions
- Emotional and physical abuse
- Violence
- Lack of family connectivity
- Parental mental health problems
- Death of a loved one
- Family homelessness
- History of foster care and adoption
- Bullying
- Sexual orientation
- Substance abuse
(Kennebeck & Bonin, 2021; Sruthi, 2022; Nationwide Children’s Hospital, 2021)
SUICIDE IN ADOLESCENTS
Adolescents generally have a high suicide attempt rate, and those who are involved in certain subcultures have an even higher risk. For instance, there is an increased incidence of self-harm activities (such as cutting) in the “goth,” “emo,” and “punk” populations. Adolescents involved in repeated self-injury are up to eight times more likely to attempt suicide (Soreff, 2022).
It has been found that the rise in suicide and suicide attempts by adolescents correlates with the rise in electronic communication and social media. Increased digital media and smartphone use may influence mental health through several mechanisms, including the displacement of time spent in in-person social interactions, disruption of in-person social interactions, interference with sleep time and quality, cyberbullying, toxic online environments, and online information about self-harm (Twenge, 2020).
YOUNG ADULTS
Young adults experience mental health challenges at higher rates than any other age group. Close to half of those ages 18–24 struggle with mental health issues, and in 2021, 25.5% of young adults seriously considered suicide, including 10% of college students, and over 1,000 college students died by suicide. For specific ethnic and cultural groups, rates of suicide are even higher. Among American Indian and Alaska Native young adults, the rate of suicide is 2.5 times higher than that of their peers.
Many young adults continue to deal with the consequences of the COVID-19 pandemic, which has resulted in high levels of depression, loneliness, anxiety, and trauma.
The top reasons for suicide among young adults include the following:
- Depression, anxiety, and other mental health disorders
- History of substance abuse
- Exposure to violence, abuse, or other trauma, either chronic or acute
- Social isolation and loneliness
- Losing a family member through death or divorce
- Financial or job loss
- Conflict within relationships
- Starting or changing psychotropic medications
- Feeling stigmatized
- Lack of a support system
(Newport Institute, 2022)
CASE
JACOB
Avery, a registered nurse, was working the nightshift in the emergency department when an ambulance arrived with a young male patient who was discovered sitting inside his car with the engine running in a closed garage. When his mother found him, she called 911. On arrival, the patient was conscious but disoriented and was receiving high-dose oxygen via a facemask.
The young man’s name was Jacob, and he was 17 years old. His mother informed the staff that Jacob “has not been himself lately.” She went on to describe him as withdrawn and quiet, having problems sleeping, and without an appetite. He was no longer attending school functions because he felt “too tired.” He was also having problems with his girlfriend, expressing fear that she wanted to break up with him.
As Avery was drawing a blood sample, Jacob opened his eyes, pulled off the facemask, looked around, whispered, “Oh, no, I’m still here,” and began to cry.
(continues)
MIDDLE-AGED ADULTS
Middle age (35–64 years) is a time of maximum risk, with suicide rates increasing in both middle-aged men and women, although men are much more likely than women to die by suicide. Middle-aged adults account for 47.2% of all suicides in the United States, and suicide is the ninth leading cause of death for this age group (CDC, 2022d).
Middle age is a period characterized by high familial and social expectations, increased self-confidence, leadership, and community contribution, making midlife a time of well-being and peak functioning as well as a time of high stress. Well-being during this phase of life can vary considerably, from being confident and resilient when meeting changes and difficulties, to being nervous or overanxious in response to stressful events and conflicts.
Suicide rates for middle-aged women have increased more quickly compared to rates for men in recent years. Many of these women are in the “sandwich” generation, those who take care of their children as well as older parents. They are more likely to be very stressed as a result of the responsibilities they carry, increasing their risk for suicide.
Unemployment has been found to be present in 43.2% of those who die by suicide in midlife and is associated with an almost fourfold increased risk of suicide. Separation and divorce increase suicide risk by more than three times. People in this age group, especially men, consider work position, employment, and marital relationship as indicators of their social identity, and problems in these areas can be deeply distressing (AACI, 2020; Qin et al., 2022).
DEATHS OF DESPAIR (DoD)
Over the past 20 years, there has been an increased mortality rate among middle-aged adults attributable to suicide, drug overdose, and alcohol abuse. These deaths are often referred to as “deaths of despair.” Socioeconomic factors related to these deaths include:
- Low socioeconomic position and education levels
- Working in jobs with high insecurity
- Unemployment
- Living in rural areas
(Beseran et al., 2022)
OLDER ADULTS
Adults ages 65 and older comprise just 12% of the population but make up approximately 18% of suicides. Men 65 and older face the highest overall rate of suicide. Older adults tend to plan suicide more carefully and are also more likely to use more lethal methods. Among people who attempt suicide, 1 in 4 older adults will succeed, compared to 1 in 200 youths. Even if an older adult survives a suicide attempt, they are less likely to recover from the effects.
Loneliness has been found to top the list of reasons for suicide among this age group. Many of them are homebound, live on their own, and may lack the social connections needed to thrive. Other reasons may include:
- Grief over the loss of family members and friends, and anxiety about their own death
- Loss of self-sufficiency and independence
- Greater likelihood of illnesses and chronic and/or debilitating diseases such as arthritis, cardiac problems, stroke, or diabetes, which compromise quality of life
- Loss of vision and hearing make it harder to do the things they’ve always enjoyed doing
- Cognitive impairment and dementia, which can affect a person’s decision-making abilities and increase impulsivity
- Financial stress, such as living on a fixed income and/or struggling to pay bills or afford food
- Clinical depression brought on by physical, emotional, and cognitive struggles
(NCOA, 2021)
Terminally Ill and Disabled Individuals
Individuals who are terminally ill or disabled may elect to end their life by assisted suicide or euthanasia. There are different terms applied to the practice of helping a terminally ill or disabled person die by suicide. These can include medical aid in dying, physician-assisted suicide, death with dignity, right to die, or assisted suicide.
The term euthanasia means “good death.” It is an umbrella term for taking measures to end the life of someone with unbearable suffering associated with terminal illness. When a physician provides the means to die by suicide but does not administer it, it is known as passive voluntary euthanasia in the form of physician-assisted suicide. When a second party fulfills a dying person’s request to be put to death, it is referred to as active voluntary euthanasia.
In the United States, Oregon was the first state to legalize physician-assisted suicide in 1994. Since then, it has become legal in California, Colorado, Hawaii, Maine, New Jersey, New Mexico, Vermont, Washington, and the District of Columbia. Montana has legal physician-assisted suicide via a Supreme Court ruling, as there is nothing in state law prohibiting a physician from honoring a terminally ill, mentally competent patient’s request. Other states consider assisted suicide illegal (Triage Cancer, 2023; Johnson, 2022).
WASHINGTON STATE DEATH WITH DIGNITY ACT
In 2008 Washington passed the Washington Death with Dignity Act, Initiative 1000. This act allows terminally ill adults who wish to end their life to request lethal doses of medication from medical and osteopathic physicians. These individuals must be Washington residents who are 18 years of age or older, mentally competent, and terminally ill with less than six months to live as verified by two physicians.
Patients must first make an oral request to a physician, followed by a written request 15 days later, followed by a 15-day waiting period. There is then a 48-hour waiting period before picking up prescribed medications from a pharmacy.
The Death with Dignity Act has allowed adult residents to request lethal doses of medication from a physician. In 2023, a total of 545 Washington residents participated in the Death with Dignity program. Medication was prescribed by 257 different physicians and dispensed by 62 different pharmacists.
The Department of Health received death certificates for 524 persons, for whom 427 died after taking the medication, 41 died without taking the medication, and for the remainder, it is unknown if they took the medication before dying.
Of the 427 who died after taking the medication, 86% were enrolled in hospice care, and 88% died at home or in a private residence. The average age of these individuals was 76 years. End-of-life concerns among participants who died in 2023 included:
- Less able to engage in activities making life enjoyable, 86%
- Loss of autonomy, 81%
- Loss of dignity, 57%
- Burden on family, friends, or caregivers, 51%
- Loss of control of bodily functions, 46%
- Inadequate pain control or concerns about pain control, 41%
- Financial implications of treatment, 10%
(WSDOH, 2024)
Suicide Risk among Specific Populations
Although suicide affects all groups of the population, the risk and protective factors for suicide may differ. The following summarizes risk and protective factors among specific populations.
PERSONS WITH DEMENTIA
Overall, people with dementia have no higher risk of dying by suicide than the general population, but the risk is significantly increased in three groups of people with dementia: those diagnosed before the age of 65, those in the first three months following diagnosis, and those with dementia and psychiatric comorbidity. In people younger than 65 years and within three months of diagnosis, suicide risk was seven times higher than in those without dementia.
Patients with early dementia may have greater cognition, giving them more insight into their disease and better enabling them to carry out a suicide plan. Severe dementia, however, could protect against suicide by decreasing a person’s capacity to implement a suicide plan. Also, impairment in cognition and personal activities of daily living are associated with greater risk of nursing home admission, which in itself is a risk factor for suicide (Alothman et al., 2022; Joshaghani et al., 2022).
CAREGIVERS
More than 21% of the U.S. population serves as caregivers to someone with an illness or disability. They are usually spouses, older children, parents, and family friends. Men and women equally share in the responsibility, which is fulfilled mostly by those ages 38–64. In 2020, 24% of caregivers were looking after more than one person. As a result of their significant social, economic, and personal contributions, caregivers experience high rates of physical and mental illness, social isolation, and financial distress. They are also at high risk for suicide.
In a U.S. study asking hospice and palliative social workers to identify patients and caregivers at risk for suicide in the previous year, 55.4% reported one or more caregivers who exhibited warning signs of suicide, 6.8% reported one caregiver who had attempted suicide, and 4.1% reported one caregiver who died by suicide (Herman & Parmar, 2022; O’Dwyer et al., 2021).
MILITARY SERVICE PERSONNEL
Suicides among military service personnel have been steadily rising during the past 10 years, and suicide is now the second-leading cause of death among this group. Greater than 90% of military suicides are by male personnel who are most often younger than 35 years of age. The most common method used for military personnel to die by suicide is a firearm.
In a study asking a group of active-duty soldiers why they tried to kill themselves, all of the soldiers indicated a desire to end intense emotional distress. Other common reasons included the urge to end chronic sadness, a means of escaping people, or a way to express desperation. In addition, rates of mental health problems have risen 65% in the military since 2000, with nearly one million troops diagnosed with at least one mental health issue. Risk for suicide increases when military personnel experience both depression and posttraumatic stress together (MSRC, 2022; ABCT, 2022).
Experiencing child abuse, being sexually victimized, and exhibiting suicidal behavior before enlistment are significant risk factors for service members and veterans, making them more vulnerable to suicidal behavior when coping with combat and multiple deployments. Military personnel reporting abuse as children have been found to be three to eight times more likely to report suicidal behavior. Sexual trauma of any type increases the risk for suicidal behavior. Men who have experienced sexual trauma are less likely than females to seek mental health care, which they may see as a threat to their masculinity. This is a strong predictor of suicide attempts in military personnel. Service members who attempted suicide before joining the military are six times more likely to attempt suicide post enlistment (APA, 2023).
Suicide among women in the military has increased at twice the rate of male service members. When compared to civilian women, those in the service are two to five times more likely to die by suicide. The primary reason is sexual trauma, particularly incidences of harassment and rape while stationed overseas, resulting from a pervading military culture that is antagonistic toward women in the military (Gorn, 2023).
There is strong evidence that among veterans who experienced combat trauma, the highest suicide risk has been observed in those who were wounded multiple times and/or were hospitalized as a result of being wounded.
Studies that looked specifically at combat-related posttraumatic stress disorder (PTSD) found that the most significant predictor of both suicide attempts and the preoccupation with thoughts of suicide is combat-related guilt about acts committed during times of war. Those with only some PTSD symptoms have been found to report hopelessness or suicidal ideation three times more often than those without PTSD (VA, 2022a).
OCCUPATION-RELATED SUICIDE
Professions that are associated with high suicide rates include law enforcement, public safety officers, physicians, and firefighters. These professionals often work long, irregular hours; witness all types of injuries; and have exposure to guns, all of which places them at high risk for suicide. Many of these professionals use alcohol, and often the trigger is divorce. Physicians have a particularly high rate of divorce because of job-related stress and the reluctance to seek help (O’Rouke & Siddiqui, 2022).
Among female nurses, the risk of death by suicide is nearly twice the risk observed in the general population. The COVID-19 pandemic has placed nurses at substantially higher risk for poorer mental health relative to other health professions (Lee & Friese, 2021).
Suicide Protective Factors
Although there are many risk factors for suicide, there are also factors that protect people from making an attempt or dying by suicide. These protective factors are both personal and environmental.
Personal protective factors include:
- Values, attitudes, and norms that prohibit suicide, such as strong beliefs about the meaning and value of life
- Strong problem-solving skills
- Social skills, including conflict resolution and nonviolent ways of handling disputes
- Good health and access to mental and physical healthcare
- Strong connections to friends and family as well as supportive significant others
- Strong sense of cultural identity
- A healthy fear of risky behaviors and pain
- Optimism about the future and reasons for living
- Sobriety
- Medical compliance and a sense of the importance of health and wellness
- Good impulse control
- A strong sense of self-esteem or self-worth
- A sense of personal control or determination
- Strong coping skills and resiliency
- Being married or a parent
External/environmental protective factors include:
- Opportunities to participate in and contribute to school or community projects and activities
- Strong relationships, particularly with family members
- A reasonably safe and stable environment
- Availability of consistent and high-quality physical and behavioral healthcare
- Financial security
- Responsibilities and duties to others
- Cultural, religious, or moral objections to suicide
- Owning a pet
- Restricted access to lethal means
(WMU, 2023; CDC, 2022e)
SUICIDE SCREENING AND ASSESSMENT
Because a significant proportion of individuals who die by suicide have seen a health professional within a few days prior to their suicide attempt, suicide screening and assessment of risk for suicide are important steps to be taken in all healthcare settings.
Suicide prevention screening refers to a quick procedure in which a standardized instrument or tool is used to identify individuals who may be at risk for suicide and in need of assessment. It can be done independently or as part of a more comprehensive health or behavioral health screening. Suicide assessment, as opposed to screening, refers to a more comprehensive evaluation done by a clinician to confirm a suspected suicide risk, to estimate imminent danger, and to decide on a course of treatment.
Suicide Screening
There is debate about the benefits of screening all patients (universal screening) for suicide risk factors and whether screening actually reduces suicide deaths. The general view, however, is that such screening should only be undertaken if there is a strong commitment to provide treatment and follow-up, since there is some evidence that screening improves outcomes when it is associated with close follow-up and treatment. Instead of universal screening, some recommend that screening be done only for those presenting with known risk factors (selective or targeted screening). Despite this lack of uniform guidance, health systems are implementing suicide screening protocols, and screening tools are already widely used in primary care settings (O’Rourke et al., 2022).
U.S. PREVENTIVE SERVICES TASK FORCE RECOMMENDATIONS
Previously the U.S. Preventive Services Task Force (USPSTF) concluded that there was insufficient evidence to assess the balance of benefits and harms of screening for suicide risk in adolescents, adults, and older adults in primary care. The USPSTF, however, recommended screening for major depressive disorder in adolescents ages 12–18 years and in the general adult population, including pregnant and postpartum persons, noting that screening should be implemented with adequate systems in place to ensure accurate diagnosis, effective treatment, and appropriate follow up. The 2022 draft recommendation statements are consistent with these previous recommendations (USPSTF, 2022).
JOINT COMMISSION RECOMMENDATIONS
The Joint Commission requires that all individuals from age 12 and above in all medical settings be screened for suicidal ideation using a validated tool. Patients who are screened and found positive for suicide risk on the screening tool should receive a brief suicide safety assessment conducted by a trained clinician to determine whether a more comprehensive mental health evaluation is required (TJC, 2023).
AMERICAN ACADEMY OF PEDIATRICS
The American Academy of Pediatrics’ age recommendations for screening state:
- Youth ages 12 and over: Universal screening
- Youth ages 8–11: Screen when clinically indicated
- Youths under age 8: Screening not indicated; assess for suicidal thoughts/behaviors if warning signs are present
Young people require screening more frequently than adults, as adolescence and young adulthood are times of rapid developmental change, and circumstances can shift frequently (AAP, 2022).
SCREENING TOOLS
The following are validated, evidence-based suicide risk screening tools:
- Beck Fast Scan: Seven questions that can help determine the intensity and severity of depression
- Suicide Risk Screen: 10-item questionnaire often used to screen for suicide in young people
- Patient Health Questionnaire (PHQ): Nine questions about self-harm, also used to identify patients at high risk of suicide
- SAFE-T: Can be used in an outpatient setting; offers insight into the extent and nature of suicidal thoughts and harmful behavior
- Columbia-Suicide Severity Rating Scale (C-SSRS): Available in multiple languages for prehospital use to assess for the presence of harmful behavior; also assesses for any known suicide attempts and suicide ideations and behaviors
- Ask (ASQ) Suicide Screening: Four brief questions to screen medical patients ages 8 years and above
- SBQ-R: A psychological, four-item questionnaire to identify risk factors for suicide in adolescents and adults
(NIMH, 2022; Columbia University, 2021; CEBC, 2020)
Recognizing Suicide Warning Signs
Besides screening for risk factors for suicide, it is important to be able to recognize statements, behaviors, and moods that indicate an individual may be at immediate risk for suicide.
Statements by a patient that constitute a suicide warning sign include language about:
- Killing oneself
- Feeling hopeless
- Having no reason to live
- Being a burden to others
- Feeling trapped
- Having unbearable pain
Behaviors that may signal risk—especially when related to a painful event, loss, or change—include:
- Increased use of alcohol or drugs
- Searching for a method to end their life, e.g., online search
- Withdrawing from activities
- Risky behaviors
- Isolating from family and friends
- Sleeping too much or too little
- Visiting or calling people to say goodbye
- Giving away prized possessions
- Aggression
- Fatigue
- Writing a will and making final arrangements
People considering suicide often display one or more of the following moods:
- Depression
- Anxiety
- Loss of interest
- Irritability
- Humiliation/shame
- Agitation/anger
- Relief/sudden improvement
(AFSP, 2023a)
CASE
GREGORY, AGE 12
Michaela is a school social worker serving children who have emotional disturbances. One of the students, Gregory, age 12, has problems with depression, irritability, interpersonal skills, and learning skills. Michaela has developed a trusting relationship with Gregory and sees him twice a week to improve his ability to function at school and with his peers.
On Monday Gregory met with Michaela and seemed more withdrawn than usual. When Michaela asked him how he was feeling, he just shrugged his shoulders and said, “Okay, I guess. I’m not sleeping very well lately.” He then started to say something else but stopped himself short. He didn’t say anything more even though Michaela asked him several other questions attempting to assess his mood. This was not unusual behavior for Gregory, but Michaela had a feeling that things were not quite right today. She felt he really wanted to talk to her about something but just wasn’t able to.
When he left the room that day, Michaela gave Gregory a piece of paper with her phone number written on it and told him he could call her if he wanted to talk. Gregory picked up his things, thanked her, and left.
Later that day, as Michaela was gathering her notes and files and getting ready to leave, she found an envelope that was addressed to her. She opened the envelope and discovered a handwritten note from Gregory that said he was happy to have her for a friend and that he wanted to say thank you for all she’d done for him.
Just then her telephone rang. It was Gregory, who was crying and saying he was trying to kill himself. He was scared and wanted someone to help him. Michaela asked him where he was, and he told her he was in his bedroom. She tried to keep him on the phone while she went into her files to get his home address, but he abruptly said goodbye and hung up the phone. Michaela immediately dialed 911 and gave this information to the dispatcher. She then hurried to the principal’s office, and the secretary contacted Gregory’s mother and father.
Later that evening, Michaela received a call at home from Gregory's mother, who said that when the police arrived, they found Gregory hanging from the towel rack in his bathroom, unconscious but still alive. She thanked Michaela for giving Gregory her phone number and for intervening. Gregory’s mother told her she believed her son would welcome a visit from her as soon as he was feeling better.
Discussion
Michaela has worked to develop a trusting relationship with Gregory and has awareness of his baseline moods and behaviors. Today, Michaela became concerned that Gregory was not behaving as usual. She recognized that he was trying to tell her something. She reached out by providing a phone number for him to call her if he decided he wished to talk. In her interactions with him today, she began to recognize the following warning signs that Gregory may be at a crisis point:
- He reported a change in his sleeping habits (not sleeping well lately).
- He displayed increased withdrawal (not wanting to talk).
- He left Michaela a note that could only be interpreted as a goodbye.
When Michaela received the distress call from Gregory with clear indications of suicidal intent, she reacted immediately to intervene, establishing his locale and calling 911. This was followed by calling his parents and reporting to designated authorities at the school.
If Michaela had not received Gregory’s phone call, she would instead have called his parents or, if they could not be contacted, called 911 to have a welfare check completed for a young person who may be considering suicide.
Suicide Risk Assessment
The purpose of a suicide risk assessment is to determine a patient’s risk and protective factors with a focus on identification of targets for intervention. The most effective assessment begins with the establishment of a therapeutic relationship with the patient.
ESTABLISHING RAPPORT
The initial contact with a person with suicidal thoughts may occur in many different settings—home, telephone, inpatient unit, outpatient clinic, practitioner’s office, rehabilitation unit, long-term care facility, or hospital emergency department. Being skilled at establishing rapport quickly is essential for all clinicians. It is imperative that the person be given privacy, be shown courtesy and respect, and be made aware that the clinician wants to understand what has happened or is happening to them.
Basic Attending Skills
Basic attending and listening skills are valuable in establishing rapport and a therapeutic alliance in order to obtain information, set the foundation for the treatment plan, and assist in determining interventions. These skills range from nondirective listening behaviors to more active and complex ones.
Positive attending behaviors are nonverbal and include:
- Eye contact. Maintaining eye contact communicates care and understanding and can show empathy and an interest in the person’s situation. Cultures vary in what is considered appropriate. Asian and Native Americans, for example, may view eye contact as aggressive.
- Body language. Usually leaning slightly toward the patient and maintaining a relaxed but attentive posture is effective. This may also include mirroring, which involves matching the patient’s facial expression and body posture.
- Vocal qualities. These include tone and inflections of the interviewer’s voice. Tonal quality may move toward “pacing,” which is matching the patient’s vocal qualities. Vocal qualities can be used to lead the patient.
- Verbal tracking. This involves using words to demonstrate that the interviewer has accurately followed what the patient is saying, such as restating or summarizing what the patient has said.
Negative attending behaviors include:
- Overuse of positive attending behaviors, which can become negative or annoying
- Turning away from the patient
- Making infrequent eye contact
- Leaning back from the waist up
- Crossing the legs away from the patient
- Folding the arms across the chest
(Grieve, 2023)
Listening Skills and Action Responses
Effective interviewing also requires nondirective and directive listening as well as directive action responses.
Nondirective listening responses are described below:
- Silence is a skill requiring practice to be comfortable with. It is very nondirective, and if used appropriately, it can be very comforting for the patient.
- Nondirective questioning includes asking for clarification, more facts, and details, best done by using open-ended questions.
- Paraphrasing, or reflection, is a verbal tracking skill that involves restating or rewording what the patient has said. There are three types of paraphrasing that can be utilized:
- Simple paraphrasing gives direction but involves rephrasing the core meaning of what the patient has said.
- Sensory-based paraphrasing involves the interviewer using the patient’s sensory words in the paraphrase (visual, auditory, kinesthetic, etc.).
- Metaphorical paraphrasing involves making an analogy or metaphor to summarize the patient’s core message.
- Intentionally directive paraphrasing is solution-focused and attempts to lead the patient toward more positive interpretations of reality.
- Empathizing is used to show that the listener identifies with the patient’s information and allows the patient the right to their feelings.
- Supporting includes agreement, offers to help, reassurance, and focusing on the here and now.
- Analyzing is helpful in gaining different alternatives and perspectives by offering an interpretation of the patient’s message, making sure the person will be receptive.
- Summarization is an informal summary of what the patient has said. It should be interactive, encouraging, and supportive, and include positives or strengths that may help the patient cope.
(Wrench et al., 2022)
Directive listening skills:
- Validating feelings involves acknowledgement and approval of the patient’s emotional state. It can help patients accept their feelings as normal or natural and can enhance rapport.
- Interpretive reflection of feeling, also referred to as advanced empathy, goes beyond surface feelings or emotions to uncover deeper, underlying feelings, which can bring about strong emotional insights or defensiveness.
- Interpretation, also known as reframing, is a classic psychoanalytic technique that can produce patient insight or a solution-focused way to help patients view their problems from a new and different perspective.
- Confrontation involves pointing out perceptual inaccuracies or inconsistencies to help the patient see reality more clearly. It works best when excellent rapport has been established, and it can be either gentle or harsh.
(Panna, 2020)
When attempting to elicit information from suicidal persons, it should be remembered that challenging or direct questions, which could be interpreted as critical, will rarely be of benefit. The individual with suicidal thoughts should be encouraged and given the opportunity to express thoughts and feelings and be allowed to discharge pent-up and repressed emotions. Asking open-ended questions encourages the person to elaborate on their answers, which can provide important context on their level of risk, access to means, and presence of intent (Aamar, 2021).
| Person’s Statement | Appropriate Responses |
|---|---|
| Everyone will be better off without me. |
|
| I just can’t bear it anymore. |
|
| I just want to go to sleep and not deal with it again. |
|
| I want it to be over. |
|
| I won’t be a problem much longer. |
|
| Things will never work out. |
|
| It is all so meaningless. |
|
ASSESSING SUICIDAL INTENT
Once it is determined that suicidal ideations are present, the next step is to determine whether the patient has active (thoughts of taking action) or passive (wish or hope to die) intent. The patient should be asked if the thoughts are new and if there are changes in the frequency or intensity of chronic thoughts. It is also important to inquire about the patient’s ability to control these thoughts.
The next step is to determine if the patient has developed a suicide plan and their degree of intent. This includes asking whether or not they have made any preparations and what they are. It is also important to determine whether the patient has a history of impulsive behaviors or substance use that may increase impulsivity, and whether they have a past history of suicidal ideation and behavior.
In addition, the clinical interview includes observing whether the patient is disconnected, disengaged, or shows a lack of rapport, as these signs are associated with an increased risk of suicide (Schreiber & Culpepper, 2022).
MURDER AND SUICIDE
Although infrequent, combined homicide/murder and suicide do occur. Any question of suicide must be coupled with an inquiry into the person’s potential for homicide. A murder-suicide is an incident where a homicide is followed by the perpetrators’ suicide, typically immediately or within 24 hours after the homicide. The vast majority of murder-suicides occur in the context of an emotionally dependent relationship that is threatened in some way. Perpetrators of homicide-suicide are more likely to be male and more likely to have recently experienced a separation (often marital) that has led to significant domestic conflict and violence. Homicide-suicides are generally perpetrated in an intrafamilial setting, with women and/or children most often the victims (Johnston, 2020).
Suicide Risk Assessment Tools
Although various suicide risk assessment tools are available, experts have repeatedly come to the conclusion that there is not any one tool that can predict who will die by suicide to any useful degree.
There are many tools available to assist healthcare professionals in determining suicidal intent. These assessment tools are used to assess a person’s intent to carry through. They are often used when positive results have been obtained with one of the screening tools mentioned above. The following are validated/evidence-based suicide risk assessment tools:
- Ask Suicide Screening Questions (ASQ) Toolkit is a four-item suicide screening tool designed to be used for people of all ages in emergency departments, inpatient units, and primary care facilities.
- Columbia-Suicide Severity Rating Scale (C-SSRS), Risk Assessment version. The risk assessment version of this tool provides a checklist of protective and risk factors for suicide and is used along with the C-SSRS screening tool. It is appropriate in all settings for all ages and for special populations in different settings. The tool features a clinician-administered initial evaluation form, a “since last visit” version, and a self-report form. The Columbia protocol questions have also been incorporated into the SAMHSA SAFE-T model with recommended triage categories.
- Beck Scale for Suicide Ideation (BSI). This 21-item self-report instrument can be used in inpatient and outpatient settings for detecting and measuring the current intensity of the patient’s specific attitude, behaviors, and plans to die by suicide during the preceding week. It assesses the wish to die, desire to make an active or passive suicide attempt, duration and frequency of ideation, sense of control over making an attempt, number of deterrents, and the amount of actual preparation for the contemplated attempt.
(TJC, 2023)
Clinical Interview
The clinical interview is the “gold standard” for suicide assessment and intervention. Topics covered during this interview include suicidal ideation, plans, self-control, intent, and safety planning.
There are three effective approaches to asking about suicide:
- Use a normalizing tone. About 60% of people who died by suicide denied suicidal ideation when asked by a healthcare provider, indicating the presence of psychological and interpersonal barriers to disclosure. It is helpful to use a statement that normalizes suicide ideation, such as: “I asked you this question because almost all people at one time or another have thoughts about suicide.”
- Use gentle assumption. To make it easier for patients to disclose suicidal ideation, the interviewer assumes that certain thoughts and behaviors are already occurring in the person and gently structures questions accordingly. So, instead of asking if the person has been thinking about suicide, ask “When was the last time you had thoughts about suicide?”
- Assess the person’s mood. An exploration of mood states might include asking permission to discuss mood, and then asking patients to rate their mood using a zero–10 scale. This is followed by questions that refer to the worst or lowest mood rating the person has ever had as well as what was happening at those times that made them feel so down. In order to end with a positive note, the patient is asked about the best mood rating they’ve ever had.
Explore suicidal ideation. When the patient discloses the presence of suicidal ideation, collaboratively explore the frequency, triggers, duration, and intensity of the suicidal thoughts. During this process, it is important to show curiosity, empathy, and interest instead of judgment. If the patient denies suicidal thoughts and the denial appears to be genuine, acknowledge and accept the denial, but if the denial seems forced or is combined with symptoms of depression or other risk factors, acknowledge and accept the denial but return to the topic later.
Explore suicide plans. Once rapport is established and the patient has talked about suicidal ideation, it is important to explore suicide plans. If patients admit to a plan, further exploration is crucial. Evaluation includes assessing the specificity of the plan, its lethality, availability of the means, and proximity of social support (i.e., availability of individuals who might intervene and rescue the patient) (see “Assessing the Plan, Lethality, and Risk” below).
Assess self-control. This requires asking directly about self-control and observing for agitation, arousal, or impulsivity. Arousal and agitation adversely affect self-control and are the inner push that drives persons toward suicidal acts (Sommers-Flanagan, 2022).
STEPS TO TAKE WHEN A PATIENT REFUSES ASSESSMENT
- Obtain information from other sources, such as:
- Collateral reports from staff
- Patient’s past medical records
- Past suicide attempts
- Past nonsuicidal self-injury
- Past episodes of suicidal thinking
- Mental status assessment
- For patients who are competent and refuse services, document efforts made to gain cooperation.
- Document an explanation of the limitations of assessment and how level of risk was determined.
(Obegi, 2021)
CASE
GRACE
Alex is an occupational therapist who received a referral from a primary care physician for a patient named Grace, who has trigeminal neuralgia. Trigeminal neuralgia is characterized by severe unilateral paroxysmal facial pain and often described by patients as the “world’s worst pain.” Alex is familiar with this syndrome and its label as the “Suicide Disease” because, even though the disease isn’t fatal, many afflicted with it take their own lives due to the intolerable and unbearable pain.
When Grace arrives for her first appointment, Alex quickly establishes rapport with her by using basic attending and listening skills. He reviews the disease process, describes what types of therapy he can offer, and discusses the aims of occupational therapy management in terms of adapting Grace’s activities of daily living in response to her pain and improving her quality of life. After performing Grace’s initial evaluation, Alex asks Grace to be involved in setting some realistic and meaningful short- and long-term goals for her treatment.
At each session throughout the course of Grace’s treatment, Alex engages her in conversation using open-ended questioning, during which he observes her and listens for red flags that may indicate suicidal thinking. During one session, he notices that she has become more withdrawn, appears sad and listless, and begins to talk about how she doesn’t think she can continue to deal with the pain much longer. Alex then asks her direct questions to screen her for suicide risk. After scoring the risk assessment tool, he contacts her physician for follow up.
Discussion
Alex has worked to establish a trusting relationship with Grace, and being aware of the potential outcome of this disorder, listens to her and observes her very carefully. When there is a change in her behavior and talk of feeling hopeless, he recognizes them as red flags and proceeds to screen her for suicide risk, asking the six questions included in the screening version of the Columbia Suicide Severity Rating Scale. Upon completion of the screening, he contacts her physician, who will determine management.
ASSESSING THE PLAN, LETHALITY, AND RISK
The evaluation of a suicide plan is extremely important in order to determine the degree of suicidal risk. When assessing the lethality of a plan, it is important to learn all the details about the plan, the method chosen, and the availability of means. People with definite plans for a time, place, and means are at high risk for suicide. Someone who is considering suicide without making a plan is at lower risk.
Suicidal deaths are more likely to occur when persons use highly damaging, fast-acting, and irreversible methods—such as jumping from heights or shooting—and do so when rescue is fruitless.
IMPULSIVITY AND SUICIDE
Some suicides are carefully planned and deliberate, while others appear to have been impulsively decided upon, involving little or no planning. Impulsiveness is thought to play an instrumental role in suicide because of the presumption that suicidal behaviors are carried out via rash decisions with little consideration for the consequences. A study of survivors of nearly lethal suicide attempts found that 1 in 4 individuals deliberated for less than 5 minutes. Another study found that 48% reported deliberating less than 10 minutes (HSPH, 2023a).
A recent study has found an altered pattern of ventromedial prefrontal cortex and frontoparietal connectivity in impulsive people who exhibit suicidal behavior, as well as reduced ventromedial prefrontal cortex value signals. This altered connectivity has been found to be disrupted in people who attempted suicide and is believed to underlie disrupted choice processes in a suicidal crisis (Wislowska-Stanek et al., 2021; Brown et al., 2020).
Methods of Suicide and Lethality
The desire for a painless method of suicide often leads individuals to choose a method that tends to be less lethal. This results in attempted suicides that do not end in death. For every 25 attempts, there is one death. For drug overdoses, the ratio is around 40 to 1.
The following are methods of suicide and the likelihood that they will result in death:
- Firearms: 82.5%
- Drowning/submersion: 65.9%
- Suffocation/hanging: 61.4%
- Gas poisoning: 41.5%
- Jumping: 34.5%
- Drug/poisoning: 1.5%
- Cutting/piercing: 1.2%
- Other: 8.0%
(HSPH, 2023b)
It is of utmost importance for clinicians to recognize that these methods, as well as other highly lethal suicide methods, are widely accessible and must be considered when determining the disposition of someone who has suicidal ideations.
Factors that influence the lethality of a chosen method include:
- Intrinsic deadliness. A gun is intrinsically more lethal than a bottle of pills.
- Ease of use. If a method requires technical knowledge, for example, it is less accessible than one that does not.
- Accessibility. Given the brief duration of some suicidal crises, a gun in the cabinet in the hall is a greater risk than a very high building 10 miles away.
- Ability to abort mid-attempt. More people start and stop mid-attempt than carry through. It is easier to interrupt a hanging or to call 911 after overdosing than to stop a method such as jumping off a bridge or using a gun.
- Acceptability to the individual. The method must be one that does not cause too much pain or suffering. For example, fire is readily accessible, but it is a method seldom used in the United States.
(HSPH, 2023b)
MEANS RESTRICTION
There is strong evidence that reducing access to or the toxicity of a commonly used and highly lethal means is associated with reductions in suicides. Means restriction leads to a temporary or permanently delayed suicide attempt by allowing for the suicide crisis to pass. Means restriction can also allow for delay in order to find a substitution means, which on average are less lethal. Delays can save some lives, but not all. (See also “Reducing Access to Lethal Means” later in this course.)
Level of Risk
A clinical judgment that is based on all the information obtained during assessment should help to assign a level of risk for suicide and determine the setting of care.
Patients who are low risk of suicide:
- Are experiencing recent suicidal ideation or thoughts
- Have no specific current suicide plan
- Have no clear intent to act
- Have not planned or rehearsed a suicide act
- Have identifiable and multiple protective factors
- Have limited risk factors
- Have no history of suicidal behaviors
- Have evidence of self-control
- Have supportive family members or significant others
- Have a high degree of ambivalence
Most people with suicidal ideation do not necessarily want to die; they just do not want to continue living in an intolerable situation or state of mind. This ambivalence is one of the most important tools for working with such persons. Almost everyone with suicidal thoughts is ambivalent about dying, leaning toward suicide at one moment in time, and then leaning toward living the next. The healthcare professional can use this ambivalence to help focus the person on the reasons why they should live.
Patients who are at moderate risk:
- Have current suicide ideation
- Have no clear plan for suicide
- Have had no preparatory behavioral or rehearsal of act
- Have limited or no intention to act
- Have limited identifiable protective factors
- Are able to control the impulse
- Have the ability to maintain safety, independent of external support
- Have no recent suicidal behavior
- Have supportive family or significant others
- Have a high degree of ambivalence
Patients who are at high/severe/imminent risk:
- Have strong, persistent suicidal ideation
- Have strong intention to plan or act
- Have a specific suicide plan
- Have access to lethal means
- Have minimal protective factors
- Have impaired judgment
- Have poor self-control either at baseline or due to substance use
- Have inability to maintain safety, independent of external support
- Have a poor social support network
- Have severe psychiatric symptoms and/or an acute precipitating event
- Have a history of prior suicide attempt
(VA, 2022b)
PREDICTING SUICIDE BY RISK LEVEL
There has been no improvement in the accuracy of predicting suicides in the past 40 years.
- 95% of “high-risk” patients will not die by suicide.
- 50% of suicides are from “low-risk” patients.
- 50% of individuals who complete suicide have no prior history of suicide attempts.
(PsychDB, 2021)
Differentiating between Non-Suicidal Self-Injury and Suicide Attempt
Healthcare professionals are increasingly confronted with another problem related to suicide attempts called non-suicidal self-injury (NSSI). DSM-5 defines NSSI as the “deliberate, self-inflicted destruction of body tissue without suicidal intent and for purposes not socially sanctioned” (APA, 2013).
Self-harm is a sign of emotional distress, and adolescents are at the highest risk, with approximately 15% of teenagers and 17%–35% of college students having been found to inflict self-harm injury. Both males and females have similar rates of NSSI. Studies have found the following reasons given for engaging in self-harm behavior:
- To feel a sense of control over the body or life situations
- To punish oneself for perceived faults
- To reduce negative emotions
- To feel “something” instead of numbness or emptiness
- To avoid certain social situations
- To receive social support
The greatest difference between suicide and self-harm is intent. Suicide is a method that can end pain, but self-harm is an act to enhance coping with feelings and stressors. Some individuals find that pain from self-injury is reassuring when they are feeling numb or disconnected from the world around them. NSSI, however, can increase the risk of suicide because of the emotional problems that trigger self-injury and the pattern of damaging the body in times of distress.
It is important to keep in mind that the act of self-harm induces pain receptors that trigger the brain to feel an adrenaline “rush.” This can readily become addictive and highly dangerous (Discovery Mood & Anxiety Program, 2023; Mayo Clinic, 2022).
ASSESSMENT OF NSSI PATIENTS
Assessment of the patient who presents with non-suicidal self-injurious behavior includes:
- Determining what type of injury and how many types of injuries the patient has inflicted
- Determining how often non-suicidal self-injury occurs and how long it has been occurring
- Determining the function of NSSI for the patient
- Assessing for coexisting psychiatric disorders
- Estimating the risk of suicide attempt
- Determining how willing the patient is to participate in treatment
The most common examples of NSSI include cutting or stabbing the skin with a sharp object and burning the skin. Patients often injure themselves repeatedly in a single session, creating multiple lesions in the same location, typically in areas that are easily hidden but accessible, such as the forearms, chest, abdomen, or front of the thighs. The behavior is often repeated, resulting in extensive patterns of scarring (Moutier, 2022).
Signs of NSSI that may be found during the physical examination include:
- Scars, often in patterns
- Fresh cuts, scratches, bruises, bite marks, or other wounds
- Wearing long sleeves or long pants to hide self-injury, even in hot weather
- Frequent reports of accidental injury
(Mayo Clinic, 2022)
Once signs of NSSI are identified, an assessment tool can be used to aid in diagnosing NSSI and differentiating patients who are at increased risk of suicide. These may be either self-administered or clinician-administered. Examples include:
- Self-Harm Behavior Questionnaire (SHBQ)
- Suicidal Behaviors Questionnaire (SBQ)
- Self-Injurious Thoughts and Behaviors Interview (SITBI)
- Suicide Attempt Self-Injury (SASSI)
- The Ottawa Self-Injury Inventory (OSI)
- The Child Behavior Checklist (CBCL)
(Wikiversity, 2021)
CASE
NEALA
Neala, a 14-year-old female, has been referred to Jensen Huang, DPT, for physical therapy evaluation and treatment of persistent back pain localized to the paraspinal muscles of both the thoracic and lumbar areas. Neala arrives with her mother and, during the clinical interview, tells Jensen that she carries a heavy backpack throughout the day at school, spends several hours a day sitting and playing video games, and is feeling depressed and anxious “because I hurt so much.”
Neala is asked to undress and put on a gown for her physical assessment. While examining Neala, Jensen notices multiple crescent-shaped bruises and scabs on her upper arms and the front of her thighs. When Jenson asks her what might have caused these marks, Neala shrugs her shoulders and replies, “Oh, I don’t know.”
As Jensen continues his examination, he again asks Neala if she has any idea what could have caused these strange marks, and Neala replies, “I just pinched myself.” On further questioning, Neala tells Jensen they were made by pinching her skin between her fingernails, and that she does this when she is feeling down and anxious. She tells Jensen she learned how to do this on a website and that it “takes the miseries away.”
Discussion
Jensen identifies Neala’s behavior as most probably non-suicidal self-injury. Although the pinching is not a method for suicide, NSSI in adolescence is a risk factor for suicide attempts throughout adulthood and is a complex behavior that requires professional treatment. Following examination, Jensen meets with both Neala and her mother to discuss treatment options for her back pain and to inform them that he will contact the referring physician for a referral for evaluation of Neala’s NSSI behaviors.
Documentation of Suicide Risk Assessment
Good documentation is basic to clinical practice. Accurate, sufficiently detailed, and concise records of a patient’s treatment allow for quality care and communication among providers. The best records reflect awareness of risk and the process of professional judgement that recognized it, took steps to reduce it, and balanced it with patient needs. The following documentation should be present in the record:
- Reason for suicide assessment
- Review of past available records
- Evaluation of warning signs and risk and protective factors
- Initial and ongoing suicide risk assessment
- Access to lethal means and mitigation
- Consultations with colleagues
- Referrals to behavioral health
- Rationale and follow-up for treatment options
- Safety planning and discharge coordination
- Plans for follow-up
(Stefan, 2020)
MODELS OF CARE FOR PATIENTS AT RISK FOR SUICIDE
A model of care is a set of interventions that can be consistently carried out in various settings to ensure that people get the right care, at the right time, by the right provider or team, and in the right place. Newer models of care for management of patients at risk for suicide include:
- Crisis support and follow-up (e.g., center hotline)
- Brief intervention and follow-up
- Suicide-specific outpatient management
- Emergency respite care
- Tele–mental health
- Inpatient psychiatric hospitalization, with suicide-specific treatment
(EDC, 2022)
Crisis Support and Follow-Up
Crisis support and follow-up can include mobile crisis teams, walk-in crisis clinics, hospital-based psychiatric emergency services, peer-based crisis services, and other programs designed to provide assessment, crisis stabilization, and referral to an appropriate level of ongoing care. Crisis centers can also serve as a connection to the patient between outpatient visits and are helpful for patients with barriers to accessing outpatient mental health services. Crisis services also include care coordination. Mobile crisis teams provide care in the community at the location of the person who has suicidal thoughts (EDC, 2022).
Brief Intervention and Follow-Up
Brief interventions range from a single, in-person session, to a computer-administered intervention in a primary care office, to an online screening and feedback intervention that can be done on a personal electronic device. Brief interventions can be an immediate intervention and also can be used in conjunction with any other level of care. Safety planning is recommended for those who refuse outpatient care. Outreach and follow-up are provided through phone calls, letters, and texts (EDC, 2022).
Suicide-Specific Outpatient Management
Suicide-specific outpatient management involves several sessions that may include dialectical behavior therapy, cognitive therapy for suicide prevention (CT-SP), and collaborative assessment and management of suicide (CAMS). It is critical that outpatient mental health providers monitor patients between appointments and follow up when patients miss appointments (EDC, 2022).
Emergency Respite Care
Emergency respite care is an alternative to inpatient or emergency department services for a person in a suicidal crisis when the person is not in immediate danger. Respite centers are usually located in residential facilities designed to be more like a home than a hospital. These facilities may include staff members who are peers who have lived experience of suicide. Respite care is increasingly being utilized as an intervention and may include help with establishing continuity of care and provision of longer-term support resources, as well as support by text, phone, or online following a stay (EDC, 2022).
Tele–Mental Health
Tele–mental health involves electronic communication to provide clinical mental health services from a distance. Healthcare organizations can use these services to provide emergency assessments and treatment, especially for those patients located in remote geographic regions and for organizations with limited access to mental health resources (EDC, 2022).
Hospitalization
Inpatient hospitalization is the most restrictive option for addressing suicide risk. Research has found that patients may be at higher risk immediately after discharge from inpatient care. The reasons why this may happen are not known; however, experts have questions as to whether there is something about the experience of hospitalization itself that may be harmful. Involuntary hospitalization has been found to be associated with increased risk of suicide both during the hospitalization and afterward. It is therefore recommended that hospitalization be carefully weighed against other options (EDC, 2022).
MANAGEMENT OF THE PATIENT AT RISK FOR SUICIDE
Patients at risk for suicide are cared for in multiple healthcare settings, including primary care, emergency departments, outpatient facilities, and inpatient facilities.
Primary Healthcare Settings
Standards for suicide prevention in primary care include primary care provider education, practice-wide implementation of screening, and effective interventions to reduce risk, including safety planning with removal of lethal means and providing caring contact around higher-risk care transitions, such as after psychiatric inpatient or emergency room discharge.
Following screening and risk assessment, referral to a higher level of care, such as behavioral health specialist and/or emergency services, is made for those with acute risk. Patients with nonacute risk are asked to complete a brief suicide safety assessment to determine if, and how soon, a comprehensive mental health evaluation is needed. Interventions for nonimminent risk that can be provided in the primary care setting include safety planning, removal of lethal means, and timely contacts following care transitions.
After a patient has been identified as at an elevated risk for suicide, safety planning during the visit is recommended. This consists of a written list of coping strategies and sources of support prioritized to assist patients with addressing a suicidal crisis, as well as with the removal or reduction of lethal means. Primary care providers can endorse public health interventions such as the pharmacy/police collection boxes for extra medications and firearms as safety measures (Spottswood et al., 2022).
Emergency Department Management
The emergency department is often the entrance into the medical system for individuals who have attempted suicide or are having suicidal thoughts.
Upon admission, a medical assessment is completed to evaluate for and treat acute medical issues. Vital signs, history of present illness, and focused physical and neurological examinations are conducted for every patient with a psychiatric complaint. One-to-one observation is ordered when there is any question of self-injurious behavior. In addition, a temporary emergency hold is ordered to ensure that the patient is not able to leave until there is an opportunity to complete a suicide risk assessment. Intoxicated patients who present with suicidal ideation are held until clinically sober and then reevaluated.
Following assessment, if the patient is deemed “low risk,” a safe discharge plan is developed and documented, clearly stating what protective factors justify the discharge (see below). If patients at any time are assessed as higher than “low risk,” a psychiatric consultation must precede any discharge. An emergency hold may be placed according to state requirements and the patient notified.
If a moderate- or high-risk patient does not opt for voluntary hospitalization or at any point withdraws their voluntary status and they are determined to pose a danger to themselves or others, they should be held under an emergency hold until a comprehensive evaluation can be completed.
It is important to document the determination of risk, noting protective and risk factors that justify the decision to either involuntary hold the patient for psychiatric consultation or discharge to home (Rohrer & Dudek, 2022).
EMERGENCY DEPARTMENT DISCHARGE PLANNING
Providers in the emergency department determine whether to discharge and refer the patient for outpatient treatment or to admit for inpatient care. When being discharged to outpatient care from the emergency department, each patient is provided a plan for follow-up. The following is a discharge planning checklist:
- Involve the patient as well as family and friends in the development of the discharge plan.
- Schedule an urgent follow-up appointment (preferably within 24 hours, or when possible, within 7 days of discharge) with a mental healthcare provider, primary care provider, or other outpatient provider.
- Verbally review and discuss the patient care plan, including a review of medications, and confirm that the patient understands them by using the teach-back technique. A safety plan may be used to address elements of patient care related to suicide risk (see box below).
- Discuss barriers, such as lack of health insurance, that may interfere with following the care plan and identify possible solutions or alternatives.
- Provide a crisis center phone number.
- Discuss limiting access to lethal means. (See “Reducing Access to Lethal Means” below.)
- Provide written instructions and educational materials.
- After obtaining consent, share the patient’s health information with referral providers.
(NSPL, 2023)
SUICIDE SAFETY PLAN
Safety planning is a clinical process involving listening, empathizing with, and engaging the patient in the development of a series of action steps to be taken in the event the patient experiences suicide ideation, arranged in order of increasing response intensity. A safety plan also includes a collaboratively written list of coping strategies and sources of support the patient can use before or during a suicidal crisis. The plan is brief, written in the patient’s own words, easy to read, and involves the following steps:
- Warning signs or triggers (thoughts, images, mood, situation, behavior) that a crisis may be developing
- Internal coping strategies for diversion (relaxation technique, physical activity) without contacting another person
- People and social settings that provide distraction
- People whom the patient can ask for help when in crisis
- Professionals or agencies the patient can contact during a crisis
- Making the environment safe, including lethal means removal
- Optional step identifying reasons for living
When introducing the suicide safety plan process, the clinician takes these steps:
- Informs the patient that the purpose of the plan is to help them recognize when a crisis may escalate so that they know to refer to their plan and take action to reduce risk
- Helps the individual identify strategies that are simple and easy to use
- Obtains feedback from the patient about the likelihood of using the strategies
- Identifies barriers and problem-solves ways to overcome them
After the plan has been developed, the clinician does the following:
- Assesses the likelihood that the overall safety plan will be used
- Discusses where the safety plan will be kept and how it will be located during a crisis
- Reviews the plan periodically when the patient’s circumstances or needs change
(Stanley, 2021; Hindman & Fleming, 2022)
CASE
JACOB (continued)
The emergency department nurse, Avery, quietly spoke to Jacob, asking him if he knew where he was. When he didn’t reply, she told him he was in the hospital being treated for carbon monoxide poisoning. He said, “Then I didn’t die?” She replied, “No, you didn’t.”
Avery waited a second or two and then asked Jacob how he was feeling. He said he was feeling very sad and disappointed. Using active listening skills, Avery encouraged him to talk. He expressed feelings of sadness, anger, and frustration, and said, “Nothing is going right in my life. I just want to get out of it!”
Assuming a suicide attempt, Avery asked Jacob, “When did you first think of harming yourself?” He replied, “Yesterday. My girlfriend told me she wanted to break up and date someone else.” Avery said, “That must have been very hard for you.” He agreed that it was.
Avery asked him if he had ever had suicidal thoughts before, and he said that he “does every so often now.” She then asked him what he meant by “every so often now,” and he replied that he’s been thinking this way for the past few months, ever since the beginning of the school year.
Discussion
Because Jacob had used a high-risk method to attempt to kill himself, Avery considered him to be at high risk for self-harm. She helped him undress and put on a hospital gown. Then she called in an ED tech to stay with Jacob while she went to report his condition and discuss treatment with the ED team. Another team member went through Jacob’s belongings to remove any objects he might use to try to harm himself again.
A psychiatric evaluation was ordered for Jacob, following which it was determined that he had signs and symptoms consistent with the diagnosis of major depression. Jacob and his mother were informed that the safest place for Jacob at the time would be in the hospital, where he could begin treatment. He was admitted voluntarily to the hospital’s acute psychiatric unit.
(continues)
Outpatient Behavioral Health Management
Patients with elevated but not imminent risk of suicide require aggressive treatment that can be provided in an outpatient setting. Interventions are initiated at an intensity that is appropriate to the level of risk. Effective interventions in outpatient management include:
- Providing appropriate therapeutic treatment and aggressive treatment for psychiatric disorders
- Involving family members/caregivers or those close to the patient in regular monitoring until safety has been further established:
- Providing the patient and caregivers 24-hour access to clinical support in case of urgent need
- Instructing family/caregivers to take the patient to the emergency department if decompensation occurs or, if patient refuses, to call the police
- Informing the patient that safety takes precedent, and that even though the patient may object, a clinician may reach out to others for additional history to alleviate the risk of suicide
- Ensuring restriction of access to all lethal means of suicide, particularly firearms and medications; discussing with family members and/or police about temporarily making them inaccessible to the patient (see also “Reducing Access to Lethal Means” later in this course)
- Scheduling sufficient numbers of clinical contacts so that the patient will feel connected and supported
- Discussing how to identify and avoid triggers for relapse of suicidal ideation and to recognize warning signs
- Educating the patient and family/caregivers about the disinhibiting effects of alcohol and other drugs
- Discussing coping strategies and sources of support to distract from suicidal ideation
(Schreiber & Culpepper, 2022)
Inpatient Behavioral Health Management
Inpatient hospitalization is the most restrictive option and is nearly always indicated for patients with a recent suicide attempt or at high risk of imminent suicide. Involuntary hospitalization may be necessary for patients who do not agree with plans for hospitalization (see box below).
Inpatient mental health treatment involves admission to a hospital or clinic for at least one overnight stay. Key suicide prevention strategies considered in this setting include staff trained in suicide risk assessment, modification of the physical environment to ensure patient safety, and provision of increased monitoring during high-risk periods. It is also critical that patient discharge plans ensure continuity of care for suicide risk (SPRC, 2020a; Schreiber & Culpepper, 2022).
INVOLUNTARY HOSPITALIZATION
Involuntary hospitalization (or commitment) means placing a person in a psychiatric hospital or unit without their consent. The laws governing involuntary hospitalization vary from state to state, but in general, they confine involuntary commitment to persons who are mentally ill and/or under the influence of drugs or alcohol and are deemed to be in imminent danger of harming themselves or others. In most states, an involuntary psychiatric commitment cannot extend beyond 72 hours without a formal hearing. This 3-day period allows patients to receive basic medical treatment.
According to Washington State Law, Title 71, Chapter 71.05 RCW, an individual can be involuntarily committed when the person refuses voluntary admission and the healthcare professionals “regard such person as presenting as a result of a behavioral health disorder an imminent likelihood of serious harm, or as presenting an imminent danger because of grave disability.” A petition is a legal request filed by a designated mental health professional for not more than 120 hours (5 days, excluding weekends and holidays) for evaluation and treatment before a probable cause hearing must be held. Following the 72-hour hold, if needed, a court hearing can result in additional commitments of 14, 90, or 180 days. The goal is to stabilize the patient sufficiently so that they can return to the community as quickly as possible (AFSP, 2022b; Washington State Legislature, n.d.).
(See also “Ethical Issues and Suicide” later in this course.)
A decision to admit a patient to a psychiatric hospital is mainly based on an assessment of the danger a patient represent to themselves or others. The safety of the patient, therefore, is an essential prerequisite for admission, being aware that inpatient psychiatric suicide accounts for approximately 5% of all suicides. Several factors are involved, including a severe mental disorder in an acute phase, a recent suicide attempt, and the effects of stigmatization, especially in the case of involuntary hospitalization.
Patients in a psychiatric hospital setting require four levels of observation:
- General observation, with staff knowing a patient’s location at all times
- Intermittent observation, by monitoring the patient’s location every 15 minutes (and performing these checks at varying intervals of less than 15 minutes so that the patient cannot predict the exact time of the next check)
- Within sight, maintained 24 hours a day when there is a high risk of a self-aggressive act
- Within reach, requiring the patient to be within reach of a clinician at all times, including in the bathroom, when there is the highest risk
INPATIENT TREATMENT PLANNING
On admission to an acute psychiatric unit, a nurse meets with the patient to complete a nursing assessment and to orient the patient to the unit. During this interview, the presenting problem is identified and a nursing diagnosis is made. The most important concern on admission is patient safety. This may be written as: “Risk for suicide, or risk for self-directed violence related to (likely cause), as manifested by (specific behaviors).”
The initial care plan typically includes:
- Prevention of self-harm, suicide attempts, or escalation of either
- Monitoring the patient 24 hours a day
Within 24 hours, the patient is evaluated by the admitting psychiatrist and a multidisciplinary team that often includes a psychologist, medical practitioner (physician, physician’s assistant, or nurse practitioner), an RN, a social worker, and an occupational therapist. Following evaluation, the team meets with the patient to discuss the treatment plan. The plan should identify short- and long-term goals, steps to achieve them, and the professionals responsible for helping to achieve them. During hospitalization, some form of psychotherapy will also be provided.
The treatment plan outcome criteria for a patient with suicidal intent might include:
- Patient remains safe and free from harm.
- Patient cooperates with level of observation and supervision.
- Patient cooperates with healthcare team members to discuss suicidal ideation, intentions, or plans.
- Patient will be involved in appropriate interventions and treatment.
- Patient will state willingness to learn new coping strategies.
- Patient will express a positive future orientation and the will to live.
- Patient returns to a safe environment when discharged.
(APNA, 2023; Elsevier Clinical Skills, 2020)
CASE
JACOB (continued)
Robert, the psychiatric nurse who received Jacob’s admission orders, greeted Jacob on his admission and helped him get settled and oriented to the unit. Jacob’s belongings were checked in, and his belt and shoelaces were removed. Robert then spent the next hour interviewing Jacob about the events surrounding his suicide attempt. Following the interview, Robert’s nursing diagnosis was: “Risk for suicide related to depression and adverse life events as manifested by his attempted suicide by carbon monoxide poisoning.”
The initial treatment plan involved establishing suicide precautions and assigning a psychiatric technician for 24-hour monitoring. Robert, as RN, was to monitor and record Jacob’s mood, behavior, and pertinent verbatim statements every 15 minutes.
In the morning, Robert presented Jacob’s history to the team that included the psychiatrist, Dr. Ramos; the social worker, Marion; and the occupational therapist, Nancy. Following their discussion, Robert and Jacob met with Dr. Ramos, who continued the assessment of Jacob’s depression and possible need for medication. Jacob was also seen by the social worker for evaluation and input into the treatment plan.
With Jacob’s collaboration, the treatment team wrote the following treatment plan:
Problem
Depression as manifested by sadness, frustration, anger, low energy, withdrawal, sleep and eating disturbances, and suicidal ideation with suicide attempt.
Long-Term Goal
Symptoms of depression will be significantly reduced, with absence of suicidal ideation by discharge.
Short-Term Goals
- Jacob will not self-harm and will report an absence of suicidal ideation by the end of one week.
- Jacob will sleep six to eight hours each night by the end of two weeks.
- Jacob will consume three meals each day plus snacks by the end of one week.
- Jacob will begin psychotherapy to learn to identify negative and maladaptive thoughts and how to replace them with more positive and adaptive thinking.
- Jacob will begin to learn new coping skills, including problem solving and emotional regulation.
- Jacob will actively take part in the unit milieu.
- Jacob will actively take part in occupational and/or creative art therapies.
Interventions
- Individual therapy will be provided by the social worker or clinical psychologist to help Jacob learn and implement coping skills and to help him identify, process, and resolve his feelings and concerns.
- Family therapy will be provided by the social worker to develop a post-discharge crisis plan, to provide psycho-education about depression and suicide, and to increase Jacob’s parents’ ability to support and encourage him to use new coping skills.
- Occupational therapy will help Jacob identify those aspects of his activities of daily living that are in need of change and will make recommendations to the treatment team regarding discharge planning.
- The psychiatrist and the RN will provide medication management.
Evaluation
Ongoing evaluation of Jacob’s mental status and effectiveness of the treatment plan is conducted and the treatment plan modified as needed.
INPATIENT DISCHARGE PLANNING
Discharge planning is begun at the time of admission and revised throughout the stay. A written discharge plan is developed along with the patient, family member, or other authorized representative and the treatment team. Requirements of the discharge plan include:
- The patient is medically stable, and treatment of any underlying psychiatric diagnoses has been arranged.
- A comprehensive suicide assessment and risk assessment is completed within 24 to 48 hours prior to discharge.
- At the time of discharge an appropriate treatment plan is in place.
- Other collaborators and consultants are in agreement with the discharge arrangements.
- A needs assessment, including questions regarding the patient’s income, housing situation, insurance, and aftercare support, has been completed.
- Education regarding suicide, stigma, treatment options, and management strategies have been provided.
- An effective, collaboratively written safety plan is in place, and all attempts to remove potentially lethal means of harm have been made.
- A family member, friend, or other support person who will provide assistance to the patient following discharge has been identified and notified in advance of the patient’s discharge.
- The patient and caregiver/family have been provided an explanation of the next planned level of care with written copies of the treatment plan, including details of any medications, safety plan, date of follow-up appointments, and crisis contact numbers.
- Patient has contact information for outpatient support, and a follow-up appointment has been scheduled within seven days of discharge.
- Follow-up with the patient will be conducted, ideally within 48 to 72 hours.
(APNA, 2023; USDHHS, n.d.)
TREATMENT MODALITIES FOR PATIENTS AT RISK FOR SUICIDE
Patients with suicidal thoughts warrant some form of emotional support or psychotherapy with a focus on learning more adaptive ways of coping in the future. They may also warrant medications for treatment of specific mental disorders such as major depression. Following assessment, each practitioner in each setting determines which treatment modality would be of most benefit for that particular patient.
Cognitive Behavioral Therapy
Cognitive behavioral therapy (CBT) is a “solutions-oriented” type of talk therapy that can be provided for both adults and adolescents. It is based on these core principles:
- Psychological issues are partly based on:
- Problematic or unhelpful patterns of thinking
- Learned patterns of unhelpful behavior
- Problematic core beliefs, including central ideas about the self and the world
- People experiencing psychological issues can learn better ways of coping with them.
CBT aims to help the patient identify harmful thoughts, assess whether they are an accurate depiction of reality, and if they are not, to employ strategies that challenge and overcome them.
Internet-delivered cognitive behavior therapy between a patient and therapist has also been shown to significantly decrease suicidal ideation among patients with severe depression (Cleveland Clinic, 2023a; CDC, 2022f).
Dialectical Behavior Therapy
Dialectic behavior therapy (DBT) is a type of cognitive-behavioral therapy that focuses on current situations and solutions. It is used for individuals with severe and persistent suicidality and who experience emotions very intensely. DBT is a 6-month to year-long therapy that involves a greater commitment on the part of both therapist and patient. It consists of four types of sessions:
- DBT pre-assessment to ascertain if DBT is a good fit for the patient
- Individual therapy to lessen suicidal and self-harming behaviors, to restrict actions that interfere with effective therapy, to remove obstacles to success, and to assist in replacing harmful behaviors with new skills
- Skills training in groups
- Telephone crisis coaching
(Cleveland Clinic, 2023b; VYAS, 2022)
Problem-Solving Therapy
Problem-solving therapy (PST) is a brief form of treatment that teaches and empowers patients to solve the here-and-now problems contributing to suicidal ideation, self-directed violence, and hopelessness. Interventions include psychoeducation, interactive problem-solving exercises, and motivational homework assignments (VA, 2022c).
Collaborative Assessment and Management of Suicidality (CAMS)
CAMS is a therapeutic framework that emphasizes a collaborative assessment and treatment planning process between the patient and the clinician. Central to the CAMS approach is the use of the Suicide Status Form (SSF), which is a multipurpose clinical assessment and treatment planning, tracking, and outcome tool. CAMS and SSF can be used in a single session context or for ongoing care. When used in ongoing care, it assists the clinicians in organizing the sessions to target and treat suicide “drivers” and resolve suicidality (CSPAR, 2021).
Milieu Therapy
Milieu therapy is a type of psychotherapy that has been used in psychiatric hospitals, psychiatric wards in general hospitals, and group living situations for many years. Milieu therapy provides a healing culture rich in therapeutic interpersonal relationships and provides for optimum safety and comfort. It is a structured environment designed for teaching psychosocial skills and limiting maladaptive behavior (Belsiyal & Rentala, 2022).
Group Therapy
Group therapy offers numerous advantages as a suicide prevention strategy. Groups diminish social isolation and increase social support with those experiencing similar problems. Social relationships are critically important suicide risk and protective factors. Suicide group interventions can directly target social relationships by fostering a sense of community and belonging among group members (Sullivan et al., 2021).
Creative Arts Therapy
Creative arts therapies can support mental health. These therapies facilitate dialogue, reduce stigma, and enhance expression, coping skills, empathy, and personal and cultural resonance, all of which address risk factors for suicide. They can also address the motivational phase, facilitating expression of emotions such as entrapment, loneliness, and burdensomeness, thereby cultivating belonging and protecting against suicidal ideation (Sonk, 2021).
Medications
Some medications have been shown to be effective related to suicide prevention. These include:
- Clozapine (Clozaril): The only medication to date with FDA approval for suicide risk reduction; has significant side effects that require close lab monitoring
- Ketamine: Leads to rapid reduction of depressive symptoms and suicidal ideation in as little as one day, which is especially critical for people at high risk for self-harm; given by infusion under careful medical supervision or as a nasal spray (eskatamine/Spravato) along with an oral antidepressant
- Antidepressants:
- SSRIs:
- Citalopram (Celexa)
- Escitalopram (Lexapro) (approved for adolescents 12 years of age and older)
- Paroxetine (Paxil)
- Fluoxetine (Prozac) (currently approved for patients over the age of 8 years)
- Sertraline (Zoloft)
- SNRIs:
- Venlafaxine (Effexor)
- Disvenlafaxine (Pristiq, Khedezla)
- Duloxetine (Cymbalta)
The FDA requires labeling on all antidepressants to include strong warnings about risks of suicidal thinking and behavior in children, adolescents, and young adults (Anderson, 2023; Black, 2023; DeGiorgi, 2022).
SUICIDE PREVENTION STRATEGIES
Effective suicide prevention is a comprehensive undertaking requiring the combined efforts of every healthcare provider and addressing different aspects of the problem. A model of this comprehensive approach includes:
- Identifying and assisting persons at risk. This may include suicide screening, teaching the warning signs of suicide, and providing gatekeeper training (see below).
- Ensuring access to effective mental health and suicide care and treatment in a timely manner and coordinating systems of care by reducing financial, cultural, and logistical barriers to care.
- Supporting safe transitions of care by formal referral protocols, interagency agreements, cross-training, follow-up contacts, rapid referrals, and patient and family education.
- Responding effectively to persons in crisis by ensuring crisis services are available that provide evaluation, stabilization, and referrals to ongoing care.
- Providing for immediate and long-term postvention to help respond effectively and compassionately to a suicide death, including intermediate and long-term supports for people bereaved by suicide (see “Postvention for Suicide Survivors” below).
- Reducing access to lethal means by educating families of those in crisis about safe storage of medications and firearms, distributing gun safety locks, changing medication packaging, and installing barriers on bridges.
- Enhancing life skills and resilience to prepare people to safely deal with challenges such as economic stress, divorce, physical illness, and aging. Skill training, mobile apps, and self-help materials can be considered.
- Promoting social connectedness and support to help protect people from suicide despite their risk factors. This can be accomplished through social programs and other activities that reduce isolation, promote a sense of belonging, and foster emotionally supportive relationships.
(SPRC, 2020b)
Public Health Suicide Prevention Strategies
The Centers for Disease Control and Prevention “Suicide Prevention Resource for Action” details the strategies based on the best available evidence to help states and communities prevent suicide.
- Strengthen economic supports
- Strengthen household financial security
- Stabilize housing
- Create protective environments
- Reduce access to lethal means among persons at risk of suicide (see below)
- Reduce substance use through community-based policies and practices
- Improve access and delivery of suicide care
- Cover mental health conditions in health insurance policies
- Increase provider availability in underserved areas
- Provide rapid and remote access to help
- Create safer suicide care through systems change
- Promote healthy connections
- Promote healthy peer norms
- Engage community members in shared activities
- Teach coping and problem-solving skills
- Support social emotional learning programs
- Teach parenting skills to improve family relationships
- Support resilience through education programs
- Identify and support people at risk
- Train gatekeepers (see below)
- Responses to crises
- Plan for safety and follow up after an attempt
- Provide therapeutic approaches
- Lessen harms and prevent future risk
- Intervene after suicide (postvention) (see below)
- Report and message about suicide safely
GATEKEEPER TRAINING PROGRAMS
Gatekeeper training (GKT) is one of the most widely used suicide prevention strategies. It involves training people who are not necessarily clinicians to be able to identify individuals experiencing suicidality and refer them to appropriate services. GTK improves people’s knowledge, skills, and confidence in helping those who experience suicidal ideation and enhances positive beliefs about the efficacy of suicide prevention (Hawgood et al., 2023).
One example of gatekeeper training, QPR, involves three steps—Questions, Persuade, and Refer—that can be learned in as little as two hours (Purdue University, 2022).
VETERANS HEALTH ADMINISTRATION PREVENTION FRAMEWORK
Within the Department of Veterans Affairs (VA), the Veterans Health Administration’s approach to suicide prevention is based on a public health framework that focuses on intervention within populations rather than a clinical approach that intervenes with individuals.
This public health perspective considers questions such as:
- Where does the problem begin?
- How can we prevent it from occurring in the first place?
The VA follows this systematic approach:
- Define the problem by collecting data to determine the who, what, where, when, and how of suicide deaths.
- Identify and explore risk and protective factors using scientific research methods. Develop and test prevention strategies.
- Assure widespread adoption of strategies shown to be successful.
(VA, 2018)
Under the Veterans Comprehensive Prevention, Access to Care, and Treatment (COMPACT) Act of 2020, veterans in suicidal crisis can receive free emergency healthcare at any VA or non-VA healthcare facility (VA, 2023).
Resources available for veterans and their families include:
- Suicide Prevention Coordinator, available at each VA medical center, who provides veterans with counseling and other services; as appropriate, callers to the Veterans Crisis Line are referred to their local coordinator
- Coaching Into Care, a national telephone service to educate, support, and empower family members and friends seeking care or services for a veteran (call 888-823-7458)
- Veterans Crisis Line (call 988 or text 838255)
- Suicide Safety Plan template
- inTransition, a free, confidential program offering coaching and specialized assistance over the phone for active-duty service members, Guard and Reserve members, and veterans who need access to mental health care
- Make the Connection, an online resource that connects veterans, family members, friends, and other supports with information and solutions to issues affecting their lives
- Vet Centers’ readjustment counseling services
(VA, 2018)
Washington State Suicide Prevention Initiatives
Washington State’s first suicide prevention plan was written in 1995 by DOH and the University of Washington’s School of Nursing to address youth suicide prevention. That plan was revised in 2009 and again in 2014. Washington’s first comprehensive plan for suicide prevention for people of all ages was released in 2016, and the latest plan was released in 2025 and will extend through 2034.
The Washington Suicide Prevention Plan (WSDOH, 2025) is guided by five core principles:
- Centering lived experience
- Partnerships and collaborations
- Safe and effective messaging and reporting
- Evidence-based prevention
- Culturally informed approaches
Washington’s plan is further organized into four strategic directions, each with specific goals and objectives. These play an important part in a comprehensive approach to suicide prevention and align closely with the 2024 National Strategy for Suicide Prevention:
- Healthy and connected individuals, families, and communities
- Multisector suicide prevention
- Treatment and crisis services
- Data collection, quality improvement, and research
Forefront Suicide Prevention is a Center of Excellence at the University of Washington focused on reducing suicide. Forefront has trained more than 30,000 health and school professionals and community members statewide in suicide awareness, intervention, and response skills. Efforts include:
- LEARN Suicide Prevention, a training in suicide awareness, intervention, and response skills
- Forefront Community Organizers, a volunteer support network for those who have attempted suicide and those who have lost a loved one to suicide
- Forefront Cares peer-to-peer mentoring program for newly bereaved individuals
- Safer Homes, Suicide Aware, a campaign that focuses on safe storage of medications and firearms (see box below)
Reducing Access to Lethal Means
When a person is at risk for suicide, actions are required to removal lethal means. There are many actions that can be taken by families, organizations, healthcare providers, and policymakers to reduce access to lethal means of self-harm. Examples include reducing access to medications and safe storage of firearms.
Responsible firearm storage involves keeping them locked and preferably unloaded, and separating firearms and ammunition when not in use. Secure storage options include either storing firearms away from home or locked at home in a secure gun safe, gun cabinet, or lockbox. In addition, unloaded firearms can be secured with a gun-locking device or can be disassembled with parts securely locked in separate locations.
When considering temporary gun storage with friends or relatives, under federal law, a person should not ask someone to store their firearm if that person is prohibited from possessing a firearm.
Reducing means of suffocation includes taking measures to reduce suicide by hanging. About 10% of suicides by hanging occur in the controlled environments of hospitals, prisons, and police custody. The remainder occur in the community, where ligatures and ligature points are all widely available. Healthcare systems can reduce suicide by hanging by installing collapsible shower heads, light fixtures, door knobs, and providing bedding that is resistant to tearing.
Safety measures available for individual storage and disposal of prescription and nonprescription drugs include drug lockboxes, drug buyback programs, and confidential drug return programs. Many states, including Washington also have similar online tools to identify local collection sites and resources (NAASP, 2020). (See also “Resources” at the end of this course.)
Collaborating with members of the community to increase public safety can include:
- Instituting lethal means counseling policies in health and behavioral healthcare settings and training healthcare providers in those settings
- Passing policies that exempt at-risk patients from 90-day refill policies
- Working with gun retailers and gun owner groups on suicide prevention efforts
- Distributing free or low-cost gun locks or gun safes
- Ensuring that bridges and high buildings have protective barriers
(SPRC, 2020d)
WASHINGTON’S SAFER HOMES, SUICIDE AWARE
In Washington, about 75% of gun deaths are suicides, and medication overdoses are the most frequent type of suicide attempt. Safer Homes, Suicide Aware, a program led by the University of Washington’s Forefront Suicide Prevention center, focuses on access to lethal means, particularly firearms and medications. The program targets men ages 35–64 and veterans, groups that are statistically more likely to use firearms in suicide attempts. Efforts include:
- Partnering with firearms retailers, medical providers, pharmacy professionals, and veteran-serving organizations to make sure each group understands its crucial role in preventing suicides.
- Engaging directly with community members at public events ranging from gun shows to National Night Out gatherings.
- Offering free locks in exchange for participation in a survey about secure storage practices and suicide risk awareness
(WSDOH, 2025)
Postvention for Suicide Survivors
All settings should incorporate postvention as a component of a comprehensive approach to suicide prevention. Postvention is a term often used in the suicide prevention field. It is an organized response in the aftermath of a suicide to accomplish any one or more of the following:
- To facilitate the healing of individuals from grief and stress of suicide loss
- To alleviate negative effects of exposure to suicide
- To prevent suicide among people who are at high risk after exposure to another’s suicide
Postvention ensures that individuals and families who have experienced a suicide and/or suicide attempt are offered support. Postvention activities are intended to normalize anger, minimize self-blame, help survivors find meaning in the victim’s life, and be sensitive to cultural differences regarding suicide.
Key principles for creating a comprehensive postvention effort include:
- Planning ahead to address individual and community needs
- Providing immediate and long-term support
- Tailoring responses and services to the unique needs of suicide-loss survivors
- Involving survivors of suicide loss in planning and implementing postvention efforts
All suicide prevention efforts should include a comprehensive postvention component that reduces risk and promotes healing for the immediate family and reaches out into the community to support the broader group of loss survivors, including friends, coworkers, first responders, treatment providers, and others exposed to the death (SPRC, 2020e).
INSURANCE COVERAGE FOLLOWING SUICIDE OR ATTEMPTED SUICIDE
There are federal protections to ensure that most health insurance plans will pay for medical care resulting from a suicide attempt. There are, however, many forms of health insurance, and some plans may expose people to substantial uncovered costs after an attempted suicide (NAMI, 2021).
Many people have life insurance policies. However, a suicide clause is a standard clause in life insurance policies that limits payments made to survivors of a policyholder who dies by suicide within a certain period after purchasing the policy. Insurance companies typically do not pay a death benefit if the covered person dies by suicide within the first two years of coverage, commonly known as the exclusion period.
When the exclusion period ends, the policy’s beneficiaries can receive a death benefit if the covered person dies by suicide (Cornell Law School, 2021).
POSTVENTION SERVICES AVAILABLE IN WASHINGTON STATE
Programs are available throughout Washington State to support people who have lost a loved one to suicide, such as Washington Support after Suicide, formerly known as CC Cares, offered by Crisis Connections. This program serves those newly bereaved by suicide. It was originally started and nurtured by Forefront Suicide Prevention at the University of Washington (Crisis Connections, 2025).
The Washington State Department of Health also lists many grief support resources on its website, such as the Healing Conversations Program for survivors of suicide loss. (See also “Resources” at the end of this course.)
POSTVENTION SUPPORT TO MILITARY FAMILIES
Military-sponsored programs for families and next of kin have been established to assist military dependents. Most commonly, a casualty assistance office works with them. Mental health and counseling services are available to all dependents, as are religious, financial, and legal services. A military family life consultant is available to work with the families.
- Casualty Assistance Program provides support for understanding all benefits and other forms of assistance.
- Veterans Affairs Bereavement Counseling offers bereavement support to parents, spouses, and children of active-duty and Guard or Reserve members who died while on military duty.
- Tragedy Assistant Program for Survivors (TAPS) is a national nonprofit veterans service organization that provides services to help stabilize family members in the immediate aftermath of a suicide.
- TRICARE provides mental health care services during bereavement; outpatient psychotherapy is covered for up to two sessions per week in a combination of individual, family, group, or collateral sessions.
- Bereavement camps and other groups for children include:
- Comfort Zone Camp
- The Dougy Center
- Eluna
- Good Grief Camps
- SnowballExpress
CASE
ALICIA AND PHILLIP
Alicia and Phillip, ages 15 and 17, were aware that their father had lost his job several months ago due to his company’s downsizing. He has been unsuccessful finding new employment, and they have been living on credit cards and handouts from family. They could see that their father was becoming more and more withdrawn, isolating himself, and avoiding activities he usually enjoyed. He no longer played golf with his buddies and had taken to drinking more alcohol. Their mother was concerned that he was becoming depressed and urged him to see a counselor. He told the family he was fine and would be okay once he found another job.
On Friday, as they arrived home from school, Alicia and Phillip saw an ambulance leaving their home. A police car stood in front of the house, and their mother met them at the door. She said something awful had happened. Their father had taken the handgun from his bedside table and shot himself in the head while she was out running errands.
Suddenly, their lives were turned upside down. Everything became surreal. Alicia and Phillip could not believe their father was dead. Only vaguely did they remember the people who came and went or the memorial service their mother arranged. Everything was a blur. They were in profound shock and denial.
The local newspaper headlined the news. The school nurse recognized the surname of Alicia and Phillip and consulted the school psychologist and principal. She called the teens’ mother, offering support and care. She referred the family to local resources, including an ongoing support group for suicide survivors offered by the local mental health agency. The nurse also arranged a suicide prevention workshop at the high school.
Alicia and Phillip joined the survivor group and did well. Their mother sought individual counseling for assistance with her grieving process and the aftermath of her loss.
Discussion
This case study outlines the efforts made to provide postvention care for a family that has experienced the loss of a loved one. The focus is on providing referrals to resources and support services, as well as efforts to teach the teen’s schoolmates about suicide prevention.
ETHICAL ISSUES AND SUICIDE
Healthcare providers are guided by a code of ethics based on these principles:
- Autonomy: Respect for the individual’s self-determination
- Beneficence: Doing the greatest possible good
- Nonmaleficence: Preventing or minimizing harm
- Justice: Fairness and equal access to care
Suicide prevention, however, offers several ethical dilemmas. Emergent intervention may include:
- Actions taken without the individual’s consent
- Actions which limit a person’s freedom
- Actions which often feel and are disempowering
These challenge ethical imperatives, including:
- The right of a person to autonomous choice versus the need to protect vulnerable people (do no harm)
- Confidentiality versus the release or solicitation of information in order to prevent harm
- Freedom of choice to decide to live or die versus everything necessary should be done to preserve life
Involuntary hospitalizations and compulsory treatment can raise legal and ethical issues, as they violate basic civil rights, restrict the freedom of individuals, and impose significant responsibilities on physicians. This high sense of responsibility may cause physicians to cross their limits and ignore the autonomy of individuals while exercising their authority.
Healthcare providers’ duty to do no harm (nonmaleficence) can contradict the autonomy of a patient with suicidal ideation. Reporting suicide ideation to members of the healthcare team not providing direct care to a patient complies with the beneficence principle; however, this would breach patient confidentiality. This leads to a dilemma; neither can be chosen without violating the other.
The ethical principle of autonomy calls for respect, dignity, and choice, and therefore a person should not be coerced or manipulated into treatment if they are capable of autonomous decision-making. Taking away a person’s freedom when no crime has been committed is a very serious enterprise. Cases involving a suicidal patient are the classic example of what is considered justified involuntary hospitalization. However, there is ambivalence concerning this, and it is argued by some that the risk of suicide by itself may not be sufficient justification and can increase the risk of suicide following discharge.
Evidence is accumulating about harms inherent in civil commitment. Three arguments include:
- Inadequate attention has been given to the harms resulting from the use of coercion and the loss of autonomy.
- Inadequate evidence exists that involuntary hospitalization is an effective method to reduce deaths by suicide.
- Some patients with suicidal ideation may benefit more from therapeutic interventions that maximize and support autonomy and personal responsibility.
(Borecky et al., 2019; Colack et al., 2021)
Differing Perspectives
There are several different perspectives when approaching the question of what should be done about a patient who has expressed verbally or by action the wish to die. Three such points of view are the libertarian, the communitarian, and the egalitarian-liberal perspectives.
The libertarian perspective is centered on the idea of autonomy and generally rejects involuntary hospitalization because it:
- Takes away the person’s freedom
- Restricts what the person can do with their body
- Prevents the person from protecting property (job, home)
- Is a means to manage people who do not adhere to social norms
- Coerces and manipulates patients into treatment
- Raises financial issues that may affect the patient and/or infringe on the property rights of other citizens (e.g., use of tax dollars)
- Does not recognize that suicide is sometimes a rational choice based on competent thought and decision-making skills
The communitarian perspective disregards the person’s autonomy and exclusively considers the community values of the clinician making the decision. It views suicide as morally wrong and offensive to the dominant group, and intervention must take place to prevent it.
The egalitarian-liberal perspective emphasizes the equality of access to resources. This approach states that the government’s role is to protect individual rights and that the right to health is a priority. If the right to health is not protected, then the rights of liberty and autonomy may not be possible. Involuntary hospitalization protects the person from a decision-impairing disease or disorder that puts the patient at risk for self-injury or death, and treatment of said disease or disorder gives the patient the right of health. However, the question remains as to how a mental health professional can know in advance that forcible treatment is justified, especially since there are no objective tests to verify whether or not a decision-impairing disease or disorder may or may not exist (Sandu et al., 2018).
CONCLUSION
Suicide—the deliberate ending of one’s own life—is an important public health concern around the world. Many complex factors contribute to a person’s decision to die by suicide, including biologic, psycho-sociocultural elements, and adverse life events. One important thing to consider is that most people are ambivalent about dying by suicide. They are caught in a situation from which they see no way out but to end their lives. This ambivalence is important, as it is the starting point at which an effective intervention can occur.
It is imperative that healthcare professionals understand the ways in which they can assess and manage suicidal individuals and learn the skills necessary to effectively intervene and prevent a suicide from happening. These skills include:
- Recognizing who is at risk, especially those who may be at high risk in the near future
- Learning how to communicate openly with those suspected to be at risk
- Responding to the needs of persons who have attempted suicide and survived in order to prevent future suicidal behavior
- Working with survivors of a suicide loss to help protect them from consequences such as taking their own lives, PTSD, and depression
- Providing suicide prevention education to others
RESOURCES
American Foundation for Suicide Prevention
Ask Suicide-Screening Questions (ASQ)
Columbia-Suicide Severity Rating Scale (C-SSRS)
National Strategy for Suicide Prevention (National Action Alliance for Suicide Prevention)
Suicide & Crisis Lifeline
988 (call or text)
800-273-TALK (8255)
Suicide prevention (National Institute of Mental Health)
Suicide Prevention Resource for Action (CDC)
Suicide resources (CDC)
Washington State
Forefront Suicide Prevention (University of Washington)
Grief support and resources (WA State Department of Health)
Safe medication return (WA State DOH)
Suicide prevention (WA State DOH)
Washington resources (Suicide Prevention Resource Center)
Washington suicide hotlines (Suicide.org)
REFERENCES
AACI. (2020). Healthy living blog-mental health and suicide rates in middle-aged adults. https://aaci.org/healthy-living-blog-mental-health-and-suicide-rates-in-middle-aged-adults/
Aamar R. (2021). Suicide risk assessment: How to talk about suicidal ideation. Relias. https://www.relias.com/blog/suicide-risk-assessment
Akkas F. (2022). Suicides during and shortly after pregnancy are an urgent concern. https://www.pewtrusts.org/en/research-and-analysis/articles/2022/10/06/suicides-during-and-shortly-after-pregnancy-are-an-urgent-concern
Alothman D, Card T, Lewis S, et al. (2022). Risk of suicide after dementia diagnosis. JAMA, 79(11), 1148–54. doi:10.1001/jamaneurol.2022.3094
Alvarez K, Polanco-Roman L, Breslow AS, & Molock S. (2022). Structural racism and suicide prevention for ethnoracially minoritized youth: A conceptual framework and illustration across systems. The American Journal of Psychiatry, 179(6), 422–33. https://doi.org/10.1176/appi.ajp.21101001
American Academia of Pediatrics (AAP). (2022). Screening for suicide risk in clinical practice. https://www.aap.org/en/patient-care/blueprint-for-youth-siuicide-prevention/strategies-for-clinical-settings-for-youth-suicide-prevention/screening-for-suicide-risk-in-clinical-practice/
American Foundation for Suicide Prevention (AFSP). (2023a). Risk factors, protective factors and warning signs. https://afsp.org/risk-factors-protective-factors-and-warning-signs
American Foundation for Suicide Prevention (AFSP). (2023b). Medications as part of the treatment plan. https://afsp.org/medications-as-a-part-of-the-treatment-plan
American Foundation for Suicide Prevention (AFSP). (2022a). Suicide claims more lives than war, murder, and natural disasters. https://supporting.afsp.org/index.cfm?fuseaction=cms.page&id=1226&eventID=5545
American Foundation for Suicide Prevention (AFSP). (2022b). Therapies. https://afsp.org/therapies
American Psychological Association (APA). (2023). Trauma before enlistment linked to high suicide rates among military personnel, veterans. https://www.socialworktoday.com/news/dn_081314.shtml
American Psychological Association (APA). (2022). APA dictionary of psychology. https://dictionary.apa.org/mass-suicide
American Psychiatric Association (APA). (2013). Diagnostic and statistical manual of mental disorders (5th ed.).
America Psychiatric Nurses Association (APNA). (2023). Psychiatric-mental health nurse essential competencies for assessment and management of individuals at risk for suicide. https://www.apna.org/resources/suicide-competencies/?pageid=5684
Anderson L. (2023). Depression, risk of suicide, & treatment options. Drugs.com. https://www.drugs.com/slideshow/antidepressants-managing-side-effects-1079
Association for Behavioral and Cognitive Therapies. (ABCT). (2022). Military suicide. https://www.abct.org/fact-sheets/military-suicide/#:~:text=For%20those%20military,risk%20for%20suicide
Austin A, Craig S, D’Souza S, & McInroy L. (2022). Suicidality among transgender youth: Elucidating the role of interpersonal risk factors. J Interpers Violence, 37, 5–6. doi:10.1177/0886260520915554
Avery S. (2022). Four genes identified as heightening risk of suicidal thoughts/actions. https://psychiatry.duke.edu/news/four-genes-identified-heightening-risk-suicidal-thoughtsactions
Belsiyal CX, Rentala S, & Das A. (2022). Use of therapeutic milieu interventions in a psychiatric setting: A systematic review. J Edu Health Promot, 11, 234.
Beseran E, Pericàs J, Cash-Gibson L, Ventura-Cots M, et al. (2022). Deaths of despair: A scoping review on the social determinants of drug overdose, alcohol-related liver disease and suicide. Int J Environ Res Public Health, 19(19), 12395.
Black R. (2023). Medications for suicidal patients: Ketamine and more. Psycom. https://www.psycom.net/ketamine-suicidal-ideation-treatment
Borecky A, Thomsen C, & Dubov A. (2019). Reweighing the ethical tradeoffs in the involuntary hospitalization of suicidal patients. American Journal of Bioethics, 19(10), 71–83. doi:10.1080/15265161.2019.1654557
Brown V, Wilson J, Hallquist M, Szanto K, & Dombrovski A. (2020). Ventromedial prefrontal value signals and functional connectivity during decision-making in suicidal behavior and impulsivity. Neuropsychopharmacology, 45(6), 1034–41.
California Evidence-Based Clearinghouse for Child Welfare (CEBC). (2020). Suicide behaviors questionnaire–revised (SBQ-R). https://www.cebc4cw.org/assessment-tool/suicide-behaviors-questionnaire-revised
Canadian Psychiatric Association. (2022). Media guidelines for reporting on suicide. https://www.education.ne.gov/wp-content/uploads/2022/05/Suicide-Appropriate-terminology.pdf
Carstensen T, Ørnbøl E, Fink P, Jørgensen T, Dantoft T, et al. (2020). Adverse life events in the general population—a validation of the cumulative lifetime adversity measure. Eur J Psychotraumatol, 11(1), 1717824. doi:10.1080/20008198.2020.1717824
Center for Suicide Prevention and Recovery (CSPAR). (2021). Collaborative assessment and management of suicidality (CAMS). https://www.uwcspar.org/cams-452337.html
Centers for Disease Control and Prevention (CDC). (2025a). Suicide rates by state. https://www.cdc.gov/suicide/facts/rates-by-state.html
Centers for Disease Control and Prevention (CDC). (2025b). Suicide data and statistics. https://www.cdc.gov/suicide/facts/data.html
Centers for Disease Control and Prevention (CDC). (2025c). Health disparities in suicide. https://www.cdc.gov/suicide/disparities/index.html
Centers for Disease Control and Prevention. (2024). Web-based injury statistics query and reporting system (WISQARS). National Center for Injury Prevention and Control. https://www.cdc.gov/injury/wisqars/index.html
Centers for Disease Control and Prevention (CDC). (2022a). Suicide mortality by state. https://www.cdc.gov/nchs/pressroom/sosmap/suicide-mortality/suicide.htm
Centers for Disease Control and Prevention (CDC). (2022d). Disparities in suicide. https://www.cdc.gov/suicide/facts/disparities-in-suicide.html#age
Centers for Disease Control and Prevention (CDC). (2022e). Risk and protective factors. https://www.cdc.gov/suicide/factors/index.html
Centers for Disease Control and Prevention (CDC). (2022f). Prevention strategies. https://www.cdc.gov/suicide/prevention/index.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fviolenceprevention%2Fsuicide%2Fprevention.html
Centers for Disease Control and Prevention (CDC). (2022g). Suicide prevention resource for action. https://www.cdc.gov/suicide/pdf/preventionresource.pdf
Children’s Hospital Association (CHA), Pediatric Health Information System (PHIS). (2023). Addressing pediatric suicide. https://www.childrenshospitals.org/content/behavioral-health/summary/the-state-of-pediatric-suicide
Cleveland Clinic. (2023a). Cognitive behavioral therapy (CBT). https://my.clevelandclinic.org/health/treatments/21208-cognitive-behavioral-therapy-cbt
Cleveland Clinic. (2023b). Dialectical behavior therapy (DBT). https://my.clevelandclinic.org/health/treatments/22838-dialectical-behavior-therapy-dbt
Coimbra BM, Hoeboer CM, Yik J, Mello AF, Mello MF, & Olff M. (2022). Meta-analysis of the effect of racial discrimination on suicidality. SSM Population Health, 20, 101283. https://doi.org/10.1016/j.ssmph.2022.101283
Colack B, Cakar G, Kavas M, & Kizil E. (2021). An ethical assessment on patients involuntarily admitted to the psychiatric ward of a university hospital. Erciyes Medical Journal, 43(3).
Columbia University. (2021). A simple set of 6 questions to screen for suicide. https://www.columbiapsychiatry.org/news/simple-set-6-questions-screen-suicide
Conte Center Suicide Prevention. (2021). Neurobiology of suicide. https://prevention.conte.cumc.columbia.edu/research/projects/neurobiology-of-suicide/
Cornell Law School. (2021). Suicide clause. https://www.law.cornell.edu/wex/suicide_clause
Crisis Connections. (2025). Washington support after suicide. https://www.crisisconnections.org/wasas/
DeGiorgi R. (2022). Ketamine for suicidal ideation. BMJ, 376, 74.
Discovery Mood & Anxiety Program. (2023). The difference between self-harm and attempted suicide. https://discoverymood.com/blog/difference-self-harm-attempted-suicide/
Education Development Center (EDC). (2022). Least restrictive care. https://zerosuicide.edc.org/toolkit/treat/least-restrictive-care
Elsevier Clinical Skills. (2020). Suicide assessment and precautions. http://repository.phb.ac.id/763/1/Suicide-Assessment-and-Precautions-Skill-COVID-19-Toolkit_140420%20%281%29.pdf
Garcia K, Sanchez-Loyo L, Valasco I, & Carreón-Márquez C. (2021). Psychosocial suicide risk factors. Gaceta medica de Caracas, 129(1), 100–9.
Gorn D. (2023). Veterans in America. RAND Corporation. https://www.rand.org/multimedia/podcasts/veterans-in-america/why-so-many-military-women-think-about-suicide.html
Grieve R. (2023). Chapter 3, basic attending and listening skills. http://people.wku.edu/rick.grieve/Clinical%20Interviewing/pp/ChapterThree.pdf
Harvard T. H. Chan School of Public Health (HSPH). (2023a). Duration of suicide crises. https://www.hsph.harvard.edu/means-matter/means-matter/duration/
Harvard T. H. Chan School of Public Health (HSPH). (2023b). Lethality of suicide methods. https://www.hsph.harvard.edu/means-matter/means-matter/case-fatality
Hawgood J, Woodward A, Quinnett P, & De Leo D. (2022). Gatekeeper training and minimum standards of competency: Essentials for the suicide prevention workforce. Crisis: The Journal of Crisis Intervention and Suicide Prevention, 43(6), 516–22.
Herman E & Parmar R. (2022). Taking care of caregivers. Psychiatric Times. https://www.psychiatrictimes.com/view/taking-care-of-caregivers
Hindman R & Fleming S. (2022). Safety planning: An essential feature of cognitive behavior therapy for suicide prevention. https://www.psychiatrictimes.com/view/safety-planning-an-essential-feature-of-cognitive-behavior-therapy-for-suicide-prevention
Johnson G. (2022). Oregon ends residency rule for medically assisted suicide. KATU. https://katu.com/news/politics/oregon-ends-residency-rule-for-medically-assisted-suicide
Johnston J. (2020). The tragedy of murder-suicides. Psychology Today. https://www.psychologytoday.com/us/blog/the-human-equation/202003/the-tragedy-murder-suicides
Joshaghani N, Villa N, Badla O, et al. (2022). How residing in a long-term care facility affects suicidal risk in patients with dementia: A systematic review. Cureus, 14(8), e27858.
Khazan O. (2020). The millennial mental health crisis. The Atlantic. https://www.theatlantic.com/health/archive/2020/06/why-suicide-rates-among-millennials-are-rising/612943/
Kennebeck S & Bonin L. (2021). Suicidal behavior in children and adolescents: Epidemiology and risk factors. UpToDate. https://www.uptodate.com/contents/suicidal-behavior-in-children-and-adolescents-epidemiology-and-risk-factors
Leach L, Too L, Batterham P, Kiely K, et al. (2020). Workplace bullying and suicidal ideation: Findings from an Australian longitudinal cohort study of mid-aged workers. Int J Environ Res Public Health, 17(4), 1448.
Lee K & Friese C. (2021). Deaths by suicide among registered nurses: A rapid response call. J Psychosoc Nurs Ment Health Serv, 59(8), 3–4.
Levin M, Jury N, Mohseni K, et al. (2023). Do antidepressants increase suicide attempts? Do they have other risks? https://www.center4research.org/antidepressants-increase-suicide-attempts-risks/
Maloku A & Maloku E. (2020). Sociological perspective of suicides. Int. J. of Economics, Business and Politics, 4(2), 319–34.
Mayo Clinic. (2022). Self-injury/cutting. https://www.mayoclinic.org/diseases-conditions/self-injury/symptoms-causes/syc-20350950
MentalHelp.net. (2023). Becoming suicidal: Sociocultural contributions. https://www.mentalhelp.net/suicide/sociocultural-contributions/
Military One Source. (2022). Casualty assistance resources. https://www.militaryonesource.mil/family-relationships/survivor-casualty-assistance/survivor-casualty-assistance-resources
Military Suicide Research Consortium (MSRC). (2022). Study reveals top reason behind soldiers’ suicides. https://msrc.fsu.edu/news/study-reveals-top-reason-behind-soldiers-suicides
Monique Burr Foundation (MBF). (2023). Examination of bullying and cyberbullying. https://www.mbfpreventioneducation.org/examination-of-bullying-and-cyberbullying/
Mount Sinai. (2021). Press release. Largest genetic study of suicide attempts confirms genetic underpinnings that are not driven by underlying psychiatric disorders. https://www.mountsinai.org/about/newsroom/2021/largest-genetic-study-of-suicide-attempts-confirms-genetic-underpinnings-that-are-not-driven-by-underlying-psychiatric-disorders
Moutier C. (2022). Suicidal behavior. Merck Manual. https://www.merckmanuals.com/professional/psychiatric-disorders/suicidal-behavior-and-self-injury/suicidal-behavior
National Action Alliance for Suicide Prevention Lethal Means Stakeholder Group (NAASP). (2020). Lethal means & suicide prevention: A guide for community & industry leaders. https://theactionalliance.org/resource/lethal-means-suicide-prevention-guide-community-industry-leaders
National Alliance on Mental Illness (NAMI). (2021). Navigating health insurance following a suicide attempt. https://www.nami.org/NAMI/media/NAMI-Media/Public%20Policy/NAMI-HealthInsuranceCoverageSuicideAttempt-September-2021.pdf
National Council on Aging (NCOA). (2021). Suicide and older adults: What you should know. https://ncoa.org/article/suicide-and-older-adults-what-you-should-know
National Institute of Mental Health (NIMH). (2022). Ask suicide-screening questions (ASQ) toolkit. https://www.nimh.nih.gov/research/research-conducted-at-nimh/asq-toolkit-materials
National Suicide Prevention Lifeline (NSPL). (2023). Follow-up care. https://followupmatters.suicidepreventionlifeline.org/follow-up-starts-here
Nationwide Children’s Hospital. (2021). Understanding why kids die by suicide. https://www.nationwidechildrens.org/family-resources-education/700childrens/2021/09/understanding-why-kids-die-by-suicide
Nevada Division of Public and Behavioral Health (NV DPBH). (2021). Risk and protective factors. https://suicideprevention.nv.gov/Adult/Risk/
Newport Institute. (2022). Preventing suicide among young adults: Statistics and strategies. https://www.newportinstitute.com/resources/mental-health/suicide-among-young-adults/
Obegi J. (2021). Your patient refuses a suicide risk assessment. Now what? Current Psychiatry, 20(4), 451.
O’Dwyer S, Janssens A, Sansom A, Biddle L, et al. (2021). Suicidality in family caregivers of people with long-term illnesses and disabilities: A coping review. Comprehensive Psychiatry, 110, 152261.
Offord C. (2020). What neurobiology can tell us about suicide. The Scientist. https://www.the-scientist.com/features/what-neurobiology-can-tell-us-about-suicide-66922
O’Rourke M, Jamal R, & Siddiqui W. (2022). Suicide screening and prevention. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK531453/
Panna V. (2020). Directive listening skills [Video]. YouTube. https://www.youtube.com/watch?v=lj4qISQAOLA
Pollak J. (2021). Cognitive/neuropsychological functioning and suicidal behavior: A review of research and implications for clinical practice. Psychiatric Times, 38(11).
PsychDB. (2021). Suicide risk assessment (SRA). https://www.psychdb.com/teaching/suicide-risk-assessment-sra
Purdue University. (2022). QPR suicide prevention gatekeeper training available this fall. https://www.purdue.edu/newsroom/purduetoday/releases/2022/Q3/qpr-suicide-prevention-gatekeeper-training-available-this-fall.html
Qin P, Syeda S, Canetto S, Arya V, et al. (2022). Midlife suicide: A systematic review and meta-analysis of socioeconomic, psychiatric and physical health risk factors. Journal of Psychiatric Research, 154, 233–41.
Ramchand R. (2022). Disparities in suicide risk among lesbian, gay, and bisexual adults. McLean Hospital. https://www.mcleanhospital.org/video/disparities-suicide-risk-among-lesbian-gay-and-bisexual-adults
Ramchand R. (2021). Suicide among veterans. RAND Corporation. https://www.rand.org/pubs/perspectives/PEA1363-1.html
Rohrer N & Dudek M. (2022). How to evaluate and care for the suicidal patient in the ED. http://www.emdocs.net/how-to-evaluate-and-care-for-the-suicidal-patient-in-the-ed/
Samaritans. (2022). Myths about suicide. https://www.samaritans.org/how-we-can-help/if-youre-worried-about-someone-else/myths-about-suicide/
Samaritans. (2021). Gender and suicides. https://media.samaritans.org/documents/ResearchBriefingGenderSuicide_2021_v7.pdf
Sandu A, Frunza A, lliescu A, Unguru E, et al. (2018). A metaethical perspective on non-voluntary psychiatric hospitalization. Arch euromedica, 8(1), 117–20.
Schreiber J & Culpepper L. (2022). Suicidal ideation and behavior in adults. UpToDate. https://www.uptodate.com/contents/suicidal-ideation-and-behavior-in-adults
Sharma P. (2021). Common myths about suicide. Mayo Clinic Health Systems. https://www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/8-common-myths-about-suicide
Sommers-Flanagan. (2022). Suicide assessment for clinicians: A strengths-based model. https://www.continuingedcourses.net/active/courses/course114.php
Sonk J, Sams K, & Olsen N. (2021). Systematic review of arts-based interventions to address suicide prevention and survivorship in Australia, Canada, the United Kingdom, and the United States of America. Health Promotion Practice (HPP), 22(1), supplement.
Soreff S. (2022). Suicide. Medscape. https://emedicine.medscape.com/article/2013085-overview#a4
Spottswood M, Lim C, Davydow D, & Huang H. (2022). Improving suicide prevention in primary care for differing levels of behavioral health integration: A review. Front Med. Sec Family Medicine and Primary Care, 9.
Sruthi M. (2022). What age group is the most suicidal? MedicineNet. https://www.medicinenet.com/what_age_group_is_the_most_suicidal/article.htm
Stanley B. (2021). Stanley-Brown safety planning intervention. https://bgg.11b.myftpupload.com/wp-content/uploads/2021/08/Stanley-Brown-Safety-Plan-8-6-21.pdf
Stefan S. (2020). Documentation of assessment and treatment of suicidal patients: Best practices and common pitfalls. https://dsamh.utah.gov/wp-content/uploads/2020/08/Documentation-of-Assement-and-Treatment-Suicidal-Patients.pdf
Suicide Prevention Resource Center (SPRC). (2020a). Inpatient mental health. https://sprc.org/settings/inpatient-mental-health
Suicide Prevention Resource Center (SPRC). (2020b). A comprehensive approach to suicide prevention. https://sprc.org/effective-prevention/comprehensive-approach
Suicide Prevention Resource Center (SPRC). (2020d). Reduce access to means of suicide. https://sprc.org/comprehensive-approach/reduce-means
Suicide Prevention Resource Center (SPRC). (2020e). Postvention as prevention. https://sprc.org/news/postvention-prevention
Sullivan S, Monahan M, Mithcell E, Spears A, et al. (2021). Group treatments for individuals at risk for suicide: A PRISMA scoping review (ScR). Psychiatry Research, 304, 114108.
The Commonwealth Fund. (2020). New international report on health care: U.S. suicide rate highest among wealthy nations. https://www.commonwealthfund.org/press-release/2020/new-international-report-health-care-us-suicide-rate-highest-among-wealthy
The Joint Commission (TJC). (2023). Suicide prevention. https://www.jointcommission.org/resources/patient-safety-topics/suicide-prevention/
Tragedy Assistance Program for Survivors (TAPS). (2023). Caring for the families of America’s Fallen Heroes. https://www.taps.org/
Triage Cancer. (2023). Death with dignity laws. https://triagecancer.org/deathwithdignity
Twenge J. (2020). Increases in depression, self-harm, and suicide among U.S. adolescents after 2012 and links to technology use: Possible mechanism. https://prcp.psychiatryonline.org/doi/full/10.1176/appi.prcp.20190015
UCLA School of Law. (2021). More than 60% of suicide attempts among LGBQ people happen within five years of realizing they are LGBQ. https://williamsinstitute.law.ucla.edu/press/suicide-coming-out-press-release/
U.S. Department of Defense (U.S. DOD). (2025). Department of defense (DOD) quarterly suicide report (QSR), 4th quarter, CY 2024. https://www.dspo.mil/Portals/113/Documents/QSR/DoD-QSR.pdf
U.S. Department of Health and Human Services (USDHHS). (n.d.). Chapter 34. Suicide prevention and care. https://www.ihs.gov/ihm/pc/part-3/p3c34/#3-34.3E
U.S. Department of Veterans Affairs (VA), Office of Suicide Prevention. (2024). 2024 national veteran suicide prevention annual report: Report findings. https://www.mentalhealth.va.gov/docs/data-sheets/2024/2024-Annual-Report-Part-2-of-2_508.pdf
U.S. Department of Veterans Affairs (VA). (2023). Office of public and intergovernmental affairs. https://www.va.gov/opa/pressrel/pressrelease.cfm?id=5852
U.S. Department of Veterans Affairs (VA). (2022a). The relationships between PTSD and suicide. https://www.ptsd.va.gov/professional/treat/cooccurring/suicide_ptsd.asp
U.S. Department of Veterans Affairs (VA). (2022b). VA/DoD Clinical practice guidelines. https://www.healthquality.va.gov/guidelines/mh/srb/
U.S. Department of Veterans Affairs (VA). (2022c). Problem-solving therapy. https://www.mirecc.va.gov/visn19/cpg/recs/9/
U.S. Department of Veterans Affairs (VA). (2018). National strategy for preventing veteran suicide 2018-2028. https://www.mentalhealth.va.gov
U.S. Preventive Services Task Force (USPSTF). (2022). Suicide risk in adolescents, adults, and other adults: Screening. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/suicide-risk-in-adolescents-adults-and-older-adults-screening
University of Washington (UW). (2025). Forefront suicide prevention. https://www.washington.edu/research/research-centers/forefront-suicide-prevention/
VYAS Psychology Training Center. (2022). Application and purpose of Dialectical Behavior Therapy (DBT) in counseling. https://psychologylearnonline.com/application-and-purpose-of-dialectical-behavior-therapy-dbt-in-counseling/
Washington State Department of Health (WSDOH). (2025). 2025 Washington State suicide prevention plan. https://doh.wa.gov/sites/default/files/2025-05/971076-SuicidePreventionPlan.pdf
Washington State Department of Health (WSDOH). (2024). 2023 death with dignity act report. https://doh.wa.gov/sites/default/files/2025-01/422-109-DeathWithDignityAct2023.pdf
Washington State Legislature. (n.d.). Chapter 71.05 RCW, mental illness. https://apps.leg.wa.gov/rcw/default.aspx?cite=71.05
Western Michigan University (WMU). (2023). Protective factors. https://wmich.edu/suicideprevention/basics/protective
Wikiversity. (2021). Evidence-based assessment/Rx4DxTx of self-harm. https://en.wikiversity.org/wiki/Evidence-based_assessment/Rx4DxTx_of_self_harm#Assessment_Table_for_Suicidality_and_NSSI
Wislowska-Stanek A, Kolosowska K, & Maciejak P. (2021). Neurobiological basis of increased risk for suicidal behavior. Cells, 10(10), 2519. https://doi.org/10.3390/cells10102519
World Health Organization (WHO). (2025). Suicide. https://www.who.int/news-room/fact-sheets/detail/suicide
World Population Review. (2025). Suicide rate by country. https://worldpopulationreview.com/country-rankings/suicide-rate-by-country
Wrench J, Punyanunt-Carter N, & Thweatt K. (2022). Listening responses. https://socialsci.libretexts.org/Bookshelves/Communication/Interpersonal_Communication/Book%3A_Interpersonal_Communication_-A_Mindful_Approach_to_Relationships_(Wrench_et_al.)






Customer Rating
5.0 / 137 ratings