Identifying and Reporting Child Abuse, Neglect, and Trafficking
Online Continuing Education Course

Course Description
This online course covers recognizing indicators of child abuse, child neglect, and child maltreatment for physical, sexual, and psychological abuse, and recognizing child trafficking. Includes risk factors, interventions, and mandated reporting requirements and procedures. Applicable for nursing, occupational therapy, physical therapy, and EMS personnel.
"Very well done." - Yvonne, RN in New Jersey
"Great information in an understandable format." - Lori, RN in California
"Very enlightening and useful!" - Jenna, OT in Louisiana
"This is a very important topic, especially for providers who care for children. Although this is a touchy subject, it is very important that we as healthcare providers can identify and help these children get the help they need. I took this course because it is sometimes hard to talk to parents about the topic." - Kathleen, RN in Alaska
Identifying and Reporting Child Abuse, Neglect, and Trafficking
Copyright © 2024 Wild Iris Medical Education, Inc. All Rights Reserved.
LEARNING OUTCOME AND OBJECTIVES: Upon completion of this course, you will have gained the knowledge to identify and report child abuse, child neglect, and trafficking. Specific learning objectives to address potential knowledge gaps include:
- Define terminology related to child abuse.
- Explain the risk and protective factors contributing to child abuse and neglect.
- Recognize physical and behavioral indicators of abuse, neglect, and trafficking.
- Summarize strategies for responding to victims’ disclosures.
- Describe situations in which mandated reporters must report suspected cases of child maltreatment.
- Discuss the consequences for failing to report suspected child abuse.
TABLE OF CONTENTS
WHAT IS CHILD ABUSE?
The abuse or maltreatment of children is against the law. The government has a responsibility to protect children when parents or other persons legally responsible for a child’s care fail to provide proper care and to intervene in cases of child abuse or maltreatment. Likewise, healthcare professionals have a responsibility to recognize and report suspected child abuse and maltreatment.
State statutes are divided into criminal and civil categories within each state’s statutory codes. Civil statutes provide guidance for mandated reporters and intervention by child protection agencies. Criminal statutes define which acts are criminal and can lead to arrest and prosecution of an offender.
Child abuse and neglect are significant public health problems that can lead to long-term adverse consequences for a child’s health and well-being. Therefore, healthcare professionals have both a legal and professional responsibility to recognize and report suspected child abuse and maltreatment.
Definitions
The Centers for Disease Control and Prevention (CDC) views child maltreatment as a serious public health problem and has developed uniform definitions pertaining to child maltreatment. The CDC states that child abuse and neglect include all types of abuse and neglect of a child under the age of 18 by a parent, caregiver, or another person in a custodial role (e.g., a religious leader, a coach, or a teacher) that results in harm, the potential for harm, or the threat of harm to a child. CDC definitions include:
- Child Maltreatment: Any act or series of acts of commission or omission by a parent or other caregiver that results in harm, potential for harm, or threat of harm to a child
- Child Abuse (Acts of Commission): Words or overt actions that cause harm, potential harm, or threat of harm to a child. Acts of commission are deliberate and intentional and include:
- Physical abuse
- Sexual abuse
- Emotional abuse
- Child Neglect (Acts of Omission): The failure to provide for a child’s basic physical, emotional, or educational needs or to protect a child from harm or potential harm, including failure to provide:
- Housing
- Food
- Clothing
- Education
- Access to medical care
- Validation and responding appropriately to a child’s feelings
(See also “Types of Abuse” below for more details.)
FEDERAL GUIDANCE TO STATES
Federal legislation offers guidance to states by identifying a minimum set of acts or behaviors that define child abuse and neglect. The federal definition may be found in the Child Abuse Prevention and Treatment Act (CAPTA) (42 U.S.C.A § 5106g). Child abuse and neglect is defined, at minimum, as “any recent act or failure to act on the part of a parent or caregiver that results in death, serious physical or emotional harm, sexual abuse or exploitation, or an act or failure to act that presents an imminent risk of serious harm.” A child is defined as “a person who is under the age of 18 years of age and is not an emancipated minor.”
This legislation sets minimum standards for states that accept CAPTA funding, but each state provides its own definitions of maltreatment within civil and criminal statutes (CWIG, 2023).
Different states and government entities vary in their legal definitions of these terms. Therefore, it is important for healthcare professionals to know the definitions for child abuse and other related terms in the state(s) in which they live or practice.
ABUSED CHILD IN RESIDENTIAL CARE
Residential care and group homes, both public and private, provide a structured environment for children who have specific needs. These children may have behavioral health issues or disabilities. In the context of child maltreatment laws, the age limit may be extended up to 21 years old in some states if the child has a disabling condition and resides in a residential care setting.
Types of Abuse
Four commonly recognized categories of abuse are physical abuse, sexual abuse, emotional abuse, and human trafficking.
PHYSICAL ABUSE
Physical abuse of a child includes any intentional use of physical force that can result in physical injury of a child that is inflicted by a parent, caretaker, or another person in a custodial role. Type of acts include biting, kicking, hitting, shaking, burning, or other types of physical force. The legal definition of physical abuse also includes actions that pose a substantial risk of physical injury to the child even if no injury is sustained (CDC, 2024b).
SEXUAL ABUSE
Child sexual abuse generally includes any attempted or completed sexual activity or contact with a child by a caregiver. Examples include touching, fondling, penetration, or exposing a child to other sexual activities. In 36 states, the definition of sexual abuse includes human trafficking, including sex trafficking or trafficking of children for sexual purposes (CDC, 2024b; CWIG, 2022).
Child sexual abuse does not need to include physical contact between a perpetrator and a child. Some forms of child sexual abuse include:
- Exhibitionism (exposing oneself to a minor)
- Fondling
- Intercourse
- Masturbation in the presence of a minor or forcing a minor to masturbate
- Obscene phone calls, text messages, emails, or digital interaction
- Producing, owning, or sharing pornographic images or movies of children
- Sex of any kind with a minor, including vaginal, oral, or anal sex
- Sex trafficking (see below)
- Any other sexual conduct that is harmful to a child’s mental, emotional, or physical welfare
(RAINN, 2024)
EMOTIONAL ABUSE
Emotional abuse involves actions that harm the self-esteem or emotional health of a child. Behaviors may involve shaming, rejecting, name-calling, and suppressing love or affection. Emotional abuse may lead to impaired psychological growth and development and involves words, actions, and indifference. This form of abuse may be hard to recognize because there are no visible injuries. Children who are sexually or physically abused may also be emotionally abused.
Emotional abuse may include:
- Verbal abuse
- Constant criticism
- Shaming
- Name-calling
- Excessive demands on a child’s performance (e.g., expectations of high grades in school or becoming “champion” school athletes)
- Not allowing a child to attend school
- Threats
- Rejecting
- Withholding affection
- Isolation
- Negligence
(Kids Matter, 2022; CDC, 2024b)
TRAUMA AND ADVERSE CHILDHOOD EXPERIENCES
Trauma may impact a child or family, and its effects may become apparent to the many professionals who are mandated reporters of child abuse and maltreatment. It is important to remember that trauma alone may not rise to the level of child abuse or maltreatment. Instead, many effects of trauma and adverse childhood experiences can be addressed by supporting children and families and increasing protective factors against these effects (NYS OCFS, 2022).
Trauma is an intense event that threatens a person’s life or safety in a way that is too much for the mind to handle and leaves the person powerless. Trauma can bring about physical reactions such as rapid heart rate, tense muscles, or shallow breathing. Common traumatic events could be going through or seeing:
- Family violence
- Sexual abuse
- Emotional abuse
- Violence in the community
For many parents, having a child removed from the home and dealing with the child welfare system are traumatic events. In that way, trauma impacts the work of a mandated reporter in addressing possible child maltreatment or abuse.
Adverse childhood experiences (ACEs) are negative experiences that occur during childhood. Research has shown that ACEs can have lasting impacts on physical, emotional, and mental health throughout a person’s life. Research shows that ACEs are very common in all socioeconomic groups; 61%–67% of the U.S. population has experienced at least one ACE.
Children who have experienced numerous adverse experiences have higher rates of negative health outcomes, including depression, obesity, substance use, anxiety, heart disease, and early death. Other factors can intensify the effects of ACEs, including poverty, racism, generational trauma, and frequent unintended or indirect discrimination. Child maltreatment and abuse are adverse childhood experiences (NYS OCFS, n.d.-a).
HUMAN TRAFFICKING
There are different types of human trafficking, also known as trafficking in persons.
The crime of sex trafficking of children is a type of child abuse increasingly encountered in the healthcare setting. It is defined in the Trafficking Victims Protection Act (18 USC §1591) as “to recruit, entice, harbor, transport, provide, obtain, or maintain by any means a person, or to benefit financially from such action, knowing or in reckless disregard that the person has not attained the age of 18 years and will be caused to engage in a commercial sex act.”
In 2023, an estimated 1 in 6 of the 28,800 U.S. children who were reported to the National Center for Missing and Exploited Children (NCMEC) as missing were likely trafficked. It is likely that an estimated 19% of the children who ran away from foster care also became involved in sex trafficking in the same year. And NCMEC received 18,400 reports of child sex trafficking in 2023 (NCMEC, 2024).
According to U.S. federal law (22 USC § 7102), labor trafficking is the recruitment, harboring, transportation, provision, or obtaining of a person for labor or services through the use of force, fraud, or coercion for the purposes of subjection to involuntary servitude, peonage, debt bondage, or slavery. As with sex trafficking, force, fraud, or coercion do not need to exist if the labor trafficking victim is under the age of 18.
Child labor trafficking may include agricultural, domestic service, or factory work where workers provide involuntary labor. Labor trafficking can also occur in beauty services, restaurants, small businesses, or informal settings. Some common situations include peddling and traveling sales crews where young people are moved from town to town selling cheap products such as jewelry or magazines for little or no pay. Other situations include drug dealing in which children are forced to sell drugs.
Sometimes labor trafficking may occur when a child is staying with a custodial family member or nonfamily member and is forced to work. Children are controlled through fear and abuse by their traffickers. It is possible that a child is a victim of labor and sex trafficking simultaneously (NCSSLE, 2021).
Types of Neglect
Neglect is defined as the failure of a parent or other person with responsibility for the child to provide a child with basic physical and emotional needs such as food, clothing, shelter, education, and healthcare to the degree that the child’s health, safety, and well-being are threatened with harm (CDC, 2024a).
PHYSICAL NEGLECT
Physical neglect is the failure to provide a child with adequate food, shelter, clothing, education, hygiene, medical care, or supervision needed for normal growth and development. Leaving a young child or children without supervision by a responsible person is a type of neglect (Childhelp, 2021). Infants and toddlers should never be left alone, even briefly. While older preteens may be responsible and independent enough to be left alone, some older teenagers are too irresponsible or have special needs that limit their ability to be safe if left alone.
EMOTIONAL NEGLECT
Emotional neglect includes parent or other caretaker behaviors that cause or have the potential to cause serious cognitive, affective, or other behavioral health problems. The resulting emotional impairment must be clearly attributable to the unwillingness or inability of the parent or other person legally responsible for the child to exercise a minimum degree of care toward the child.
MEDICAL NEGLECT
Medical neglect is the failure to provide a child with necessary medical or mental health treatment. Some states make provisions for parents who choose not to seek certain forms of medical care for a child due to religious beliefs.
EDUCATIONAL NEGLECT
Educational neglect is the failure to educate a child (e.g., failure to enroll a child in school or preventing a child from attending school) or attend to special education needs (e.g., failure to obtain remedial education services). About half the states, the District of Columbia, American Samoa, Puerto Rico, and the Virgin Islands include failure to educate a child as required by law in their definition of neglect (CWIG, 2022).
ABANDONMENT
Abandonment is a form of neglect in many states. A child is generally considered to be abandoned when a parent’s whereabouts are unknown, the child has been left alone and suffers serious adverse consequences, or the parent fails to maintain contact with or provide reasonable support for a specified period of time.
SAFE HAVEN LAWS
“Safe haven” laws designate specific locations as safe places for parents to relinquish their unharmed newborns. The focus of safe haven laws is to protect newborns from endangerment by providing parents with an option to criminal abandonment and to protect law-abiding parents from criminal liability. Provisions of safe haven laws vary from state to state.
- These laws are usually limited to infants, and the age of the children who may be left at a safe haven varies among states. For example, in some states and Puerto Rico, only infants who are 72 hours old or younger may be relinquished to a designated safe haven, while other states allow infants up to 1 month of age.
- In most states, either parent may surrender a baby to a safe haven, but in a few states only the mother may relinquish her infant.
- Each state specifies what locations may function as safe havens. Hospitals, emergency medical services providers, healthcare facilities, and fire stations are common locations.
To date, all 50 states, the District of Columbia, and Puerto Rico have enacted safe haven legislation. Healthcare professionals must be aware of the laws governing safe haven acts in the states in which they practice and live (CWIG, 2021).
| Abuse | Neglect |
|---|---|
|
Parent or other persons legally responsible:
|
Parent or other persons legally responsible impair a child’s physical, mental, or emotional condition by:
|
CHILD ABUSE VICTIM DEMOGRAPHICS
Nationally in 2021 an estimated 600,000 children were victims of abuse and neglect. The actual number of victims could be higher because of the COVID-19 pandemic in 2021.
- 15% of all victims were in their first year of life.
- 28% of child maltreatment victims were under 2 years of age.
- The victimization rate of girls was 8.7 per 1,000 and of boys was 7.5 per 1,000.
- Native American or Alaska Native children had the highest rate at 15.2 per 1,000 children of the same race or ethnicity, and African American children had the second highest rate at 13.1 per 1,000 children of the same race or ethnicity.
- 76% of victims were neglected, 16% were physically abused, 10% were sexually abused, and 0.2% were victims of sex trafficking.
In 2021, it is estimated that 1,820 children died in the United States as the result of abuse or neglect. Boys had a fatality rate of 3.01 and girls had a rate of 2.15 per 100,000. Fatality rates were 5.6 per 100,000 for African American children, 1.94 for White children, and 1.44 for Hispanic children. This disproportionality may be due to a variety of complex factors and reflect larger societal dynamics (National Children’s Alliance, 2024).
RISK AND PROTECTIVE FACTORS
Health professionals must remain alert for risk factors that may increase the likelihood of child abuse and maltreatment. Risk factors may be either characteristics of a caregiver or of a child and may go undetected. Similarly, certain factors have been shown to safeguard children from experiencing adverse effects such as abuse and neglect.
Risk Factors for Perpetrating Child Abuse
A caregiver may have certain characteristics that increase the likelihood that they may become a perpetrator of child abuse or neglect. When health professionals observe indicators of possible abuse, they should consider whether the presence of risk factors in a caregiver may signal a need to examine the situation more carefully.
Individual risk factors include:
- Caregivers with drug or alcohol issues
- Caregivers with mental health issues, including depression
- Caregivers who don't understand children's needs or development
- Caregivers who were abused or neglected as children
- Caregivers who are young or single parents or parents with many children
- Caregivers with low education or income
- Caregivers experiencing high levels of parenting stress or economic stress
- Caregivers who use spanking and other forms of corporal punishment for discipline
- Caregivers in the home who are not a biological parent
- Caregivers with attitudes accepting of or justifying violence or aggression
Relationship/family risk factors include:
- Families that have household members in jail or prison
- Families that are isolated from and not connected to other people (extended family, friends, neighbors)
- Families experiencing other types of violence, including relationship violence
- Families with high conflict and negative communication styles
Community risk factors include:
- Communities with high rates of violence and crime
- Communities with high rates of poverty and limited educational and economic opportunities
- Communities with high unemployment rates
- Communities with easy access to drugs and alcohol
- Communities where neighbors don't know or look out for each other
- Communities where there is low community involvement among residents
- Communities with few community activities for young people
- Communities with unstable housing and where residents move frequently
- Communities where families frequently experience food insecurity
(CDC, 2024c)
Nationally, the most common risk factors reported with child maltreatment are substance abuse and domestic violence (U.S. DHHS, 2024).
Child Risk Factors
While children are not responsible for being abused, certain factors increase their risk for abuse or neglect:
- Children younger than 4 years of age
- Children with special needs that may increase caregiver burden (disabilities, mental health issues, and chronic physical illnesses)
(CDC, 2024c)
Youth at greater risk for human trafficking include those who have experienced:
- A history of abuse and neglect
- Social disconnection
- Social stigma and exclusion
(NHTTTAC, n.d.)
(See also “Recognizing Trafficking” later in this course.)
PARENTAL SUBSTANCE ABUSE AND CHILD ABUSE
Parental substance abuse greatly increases the incidence of child abuse and neglect. A review of research on parental substance abuse and its impact on children showed that:
- 1 in 5 children in the United States live in homes with parental substance abuse.
- Parents who are chemically dependent are unable to effectively parent their children.
- The health and development of children is negatively impacted by parental substance abuse.
- Children who grow up in homes with prevalent substance abuse are more likely to misuse drugs and alcohol since such norms are established at a young age.
(Thatcher, 2020)
Protective Factors Against Adverse Childhood Experiences
Individual, family, and community protective factors safeguard children from experiencing adverse effects such as abuse and neglect. There is scientific evidence to indicate that a supportive family environment and social networks have a protective effect against adverse childhood experiences.
Individual and family protective factors include:
- Nurturing relationships in the family
- Stable family relationships where children are safe, cared for, and supported
- Children having positive peer relationships
- Children being successful in school and education being valued by the family
- Children having relationships with caring adults outside the family
- Families being able to provide shelter, food, clothing, and healthcare for children
- Caregivers having college degrees or higher education
- Caregivers being consistently employed
- Families having a good social support network
- Caregivers monitoring children and enforcing rules
- Adults resolving conflict in a nonviolent manner
- Families participating in fun activities together
Community protective factors include:
- Access to financial assistance in the community
- Access to medical and mental health services
- Access to housing that is safe and stable
- Access to good-quality childcare
- Access to good-quality preschool
- Access to good-quality afterschool programming
- Access to work opportunities with policies that are supportive to families
- Strong partnerships in the community between businesses, healthcare, government, and other institutions
- Residents feeling connected and involved with one another
- Violence not being tolerated
(CDC, 2024c)
Resilience and Protective Factors
The ability to bounce back from challenges and hardship is called resilience. This quality has been shown to reduce the negative impacts of ACEs in both parents and children. Certain protective factors can boost resilience in both parents and children. These include:
- Supportive and caring relationships and social connections
- Programs that understand a person’s background and culture
- A healthy lifestyle (e.g., regular exercise, mindfulness, sufficient sleep, a healthy and nutritious diet)
- Economic support/stability for families
- Quality childcare and education early in life
(NYS OCFS, n.d.-c)
Professionals can help reduce the effects of ACEs by supporting children and families to increase these protective factors.
RECOGNIZING PHYSICAL ABUSE
There are many possible indicators of child maltreatment or abuse, and these indicators should be viewed together, not in isolation. Similarly, each indicator must be considered in relation to the child’s current age and circumstances and in the context of their physical condition or behavior. These indicators are not all-inclusive, and some children may not demonstrate signs or symptoms of abuse or neglect.
Another important aspect to assessing for possible abuse is obtaining an explanation for the presenting concern and whether that explanation is consistent with the observed physical and behavioral indicators. Abuse or maltreatment should never be assumed.
The mandated reporter is encouraged to consider any prior experiences with the child and possible differences between past and present observations.
Any assessment must be objective and free from implicit or explicit bias.
Physical Indicators of Physical Abuse
Healthcare professionals must be alert for physical injuries that are unexplained or inconsistent with the parent or other caretaker’s explanation or the developmental state of the child. However, it is important to remember that indicators of maltreatment or abuse may not always be of a physical nature or visible to view.
BRUISING
Bruising is the most common indicator of physical child abuse, and attention to bruises can be an important factor in identifying children who are at risk of physical abuse. It is important to know both normal and suspicious bruising patterns when assessing children’s injuries. Normal bruising usually occurs in the front of the body over bony areas such as the forehead, knees, shins, and elbows.
The TEN-4-FACESp validated clinical screening tool, developed by Dr. Mary Clyde Pierce, can be used to evaluate bruises in children under 4 years of age. The tool guides the clinician to assess bruising associated with three components (regions, infants, patterns) if there is no reasonable explanation for a bruise (Pierce et al., 2021). Children who are under 4 years should not have any bruises in the areas indicated in the chart below, and infants under 4 months should have no bruises anywhere. The size of the bruise is not as important as the location.
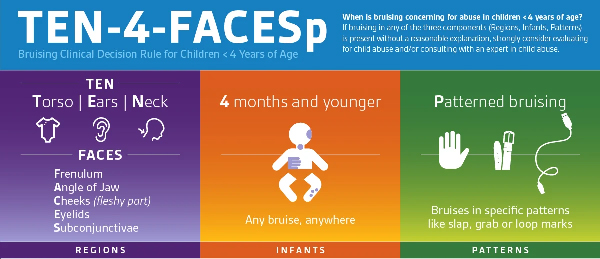
(Source: © Ann and Robert H. Lurie Children’s Hospital of Chicago.)

This pattern signals the blow of a hand to the face of a child. (Source: Research Foundation of SUNY, 2011.)

Regular patterns reveal that a looped cord was used to inflict injury on this child. (Source: Research Foundation of SUNY, 2011.)
LACERATIONS OR ABRASIONS
Typical indications of unexplained lacerations and abrasions that are suspicious include:
- On the face, lips, or mouth
- To external genitalia
BURNS
Unexplained burns include:
- Cigar or cigarette burns, especially on soles, palms, back, or buttocks
- Immersion burns by scalding water (sock-like, glove-like, doughnut-shaped on buttocks or genitalia; “dunking syndrome”)
- Patterned like an electric burner, iron, curling iron, or other household appliance
- Rope burns on arms, legs, neck, or torso

A steam iron was used to inflict injury on this child. (Source: Research Foundation of SUNY, 2011.)
FRACTURES
Unexplained fractures may include:
- Fractures to the skull, nose, or facial structure
- Multiple or spiral fractures
- Fractures in various stages of healing
(SD DSS, 2020)
HEAD INJURIES
Typical indications of unexplained head injuries include:
- Absence of hair and/or hemorrhaging beneath the scalp due to vigorous hair pulling
- Subdural hematoma (a hemorrhage beneath the outer covering of the brain, due to severe hitting or shaking)
- Retinal hemorrhage or detachment, due to shaking
- Whiplash or pediatric abusive head trauma (see box below)
- Eye injury
- Jaw and nasal fractures
- Tooth or frenulum (of the tongue or lips) injury
PEDIATRIC ABUSIVE HEAD TRAUMA
Pediatric abusive head trauma (AHT) is an inflicted head injury in children that can be caused by various mechanisms, including rotational and contact forces to the head as well as shaking. Secondary brain injury may occur as a result of hypoxia, ischemia, or inflammation, and almost all children who experience AHT develop serious long-term health problems. Impairments that result from AHT may include encephalopathy, intellectual disability, cerebral palsy, cortical blindness, seizure disorders, behavior problems, and learning disabilities. Endocrine dysfunction is commonly seen in survivors of AHT and may be observed years after the event.
AHT is the chief cause of child abuse deaths in children under the age of 5 in the United States, with approximately one third of all child abuse deaths attributed to AHT. Furthermore, up to 1 in 4 children who suffer AHT will die from resulting injury (CDC, 2024d).
The clinical presentation of infants or children with AHT can vary. Findings may be subtle and include:
- Bruising (see “TEN-4-FACESp” above)
- Oral injuries such as frenulum tears
- Retinal hemorrhages that are numerous, found in all layers of the retina, extend to the periphery of the retina, or retinoschisis (blood in the macula)
- Skull fractures
- Cerebral edema
- Subdural hemorrhages
- Spinal subdural hemorrhages
AHT should be considered when infants or young children present with:
- Fussiness or altered mental status
- Vomiting
- Apnea
Short falls (less than 5 feet) are often the explanation given to the provider for the injury; however, serious injury or death is unlikely to result from a short fall. In addition to conducting a thorough examination with imaging when AHT is suspected, clinicians should report to Child Protective Services and educate parents about the dangers of AHT from shaking or striking a child or impacting the child’s head against a surface. It is also important to educate parents about alternatives to soothe a crying baby (Narang et al., 2020).
Behavioral Indicators of Physical Abuse
Careful assessment of a child’s behavior may also indicate physical abuse, even in the absence of obvious physical injury. Behavioral indicators of physical abuse include the following:
- Withdrawal
- Problems with school or work
- Illegal or violent behavior
- Abuse of others
- Suicide attempts
- Self-harm
- Poor social skills
(Mayo Clinic, 2024)
MEDICAL CHILD ABUSE
Medical child abuse (MCA) is a relatively rare form of child abuse, although the incidence is difficult to determine because this form of child abuse is often unrecognized. In MCA, an adult falsifies an illness in the child under their care. Formerly known as Munchausen syndrome by proxy, MCA leads to unnecessary medical interventions and is potentially lethal (Horner, 2021).
Warning signs include:
- Unexplainable persistent problems
- Discrepancies of the history, findings, and clinical presentation
- A working diagnosis of a very rare condition
- Signs and symptoms only occur when the adult with the disorder is alone with the child
- The caregiver insists on hand-carrying medical records or states they are missing
- Other family members have had similar problems without explanation
- The caregiver routinely relates histories in a dramatic or exaggerated manner
- The caregiver is or has been a healthcare provider or has a history of a factitious disorder or extensive healthcare problems
- Members of the healthcare team are suspicious
(Feldman et al., 2020)
RECOGNIZING NEGLECT
Child neglect is the most common type of child maltreatment and occurs when parents and caregivers do not provide basic needs to children such as food, shelter, education, emotional validation, and medical care. Although all families experience stress from time to time, neglect is more likely to occur in families that are dealing with multiple stressors. It is important to remember that when parents and caregivers fail to provide basic needs to children because of poverty, this is not the same as neglect.
Physical indicators of neglect include:
- Consistent hunger
- Poor hygiene (skin, teeth, ears, etc.)
- Inappropriate attire for the season
- Failure to thrive (physically or emotionally)
- Positive indication of toxic exposure, especially in newborns, such as drug withdrawal symptoms, tremors, etc.
- Delayed physical development
- Speech disorders
- Consistent lack of supervision, especially in dangerous activities or for long periods of time
- Unattended physical problems or medical or dental needs
- Chronic truancy
- Abandonment
(Clermont County CPS, 2021)
A child may also demonstrate behavioral indicators of neglect such as:
- Begging or stealing food
- Extended stays at school (early arrival or late departure)
- Constant fatigue, listlessness, or falling asleep in class
- Alcohol or other substance abuse
- Delinquency, such as shoplifting
- Reports there is no caretaker at home
- Runaway behavior
- Habit disorders (sucking, nail biting, rocking, etc.)
- Conduct disorders (antisocial or destructive behaviors)
- Neurotic traits (sleep disorders, inhibition of play)
- Psychoneurotic reactions (hysteria, obsessive-compulsive behaviors, phobias, hypochondria)
- Extreme behavior (compliant or passive, aggressive or demanding)
- Overly adaptive behavior (inappropriately adult, inappropriately infantile)
- Delays in mental and/or emotional development
- Suicide attempt
(Clermont County CPS, 2021; NYS OCFS, n.d.-b)
CASE
Since his parents divorced when he was 8 years old, Riley, the youngest of four children, has spent every other week at his father’s apartment without his siblings so that he and his father could have “one-on-one time.”
By the age of 9, Riley began exhibiting signs of anxiety and anger. The boy’s teacher, Shondra Williams, noticed that he was late to school and that he arrived to school with no lunch on the days he spent at his father’s. In addition, he complained of a stomachache every day and asked the school nurse to call his mother. On several occasions he tried to leave school and run home as soon as his father dropped him off but was always seen by the staff.
When Riley came to school one day with sutures on the back of his hand, Mrs. Williams asked him to tell her what had happened. He said that his father had locked him outside in his underwear, so he punched the window to get in and cut his hand. Later that day, as Riley sat alone without eating at lunchtime, Mrs. Williams asked him privately if there was enough food in the home in order to determine if the family might need assistance. Riley told her that his father said he was fat and didn’t need any lunch.
Mrs. Williams, a mandated reporter, believed there was reasonable cause for her to suspect abuse. She conferred with the school administration and then called ChildLine to report her concerns about Riley.
An investigation revealed that Riley was having severe separation anxiety from his mother and siblings. His father’s apartment was filled with storage items, and there was no bed at the residence for Riley, who slept on a mat on the floor. There was also no food in the refrigerator, regarding which Riley’s father had stated that the child was “too fat and that he did not want to keep any food around.”
Riley was screened in to Child Protective Services (CPS) because he was diagnosed with a severe anxiety disorder by the school psychologist. A multidisciplinary team helped Riley and his family. Riley began seeing the school counselor, and at the recommendation of CPS, his visitation schedule was amended to exclude overnights with his father. In addition, his father was ordered by the court to attend parenting classes. Riley’s symptoms improved within a few months after counseling, treatment with anti-anxiety medication, and the revised visitation schedule.
RECOGNIZING SEXUAL ABUSE
Child sexual abuse involves the coercion of a dependent, developmentally immature person to commit a sexual act with someone older. For example, an adult may sexually abuse a child or adolescent, or an older child or adolescent may abuse a younger child. A perpetrator does not have to be an adult in order to sexually abuse a child (RAINN, 2024).
The fact that sexual abuse may be carried out by a family member or friend further increases the child’s reluctance to disclose the abuse, as does shame and guilt plus the fear of not being believed. The child may fear being hurt or even killed for telling the truth and may keep the abuse secret rather than risk the consequences of disclosure. Very young children may not have sufficient language skills or vocabulary to describe what happened (Clermont County CPS, 2021; RAINN, 2024).
Child sexual abuse is found in every race, culture, and class throughout society. Girls are sexually abused more often than boys; however, this may be due to boys’—and later, men’s—tendency not to report their victimization.
Most perpetrators of child sexual abuse are people who are known to the victim. As many as 93% of children who are sexually abused under the age of 18 know the abuser. There is no particular profile of a child molester or of the typical victim. Even someone highly respected in the community—the parish priest, a teacher, or coach—may be guilty of child sexual abuse. Anyone, including parents, can be a perpetrator, and most are male.
Negative effects of sexual abuse vary from person to person and range from mild to severe in both the short and long term. Victims may exhibit anxiety, difficulty concentrating, and depression. They may develop eating disorders, self-injury behaviors, substance abuse, or suicide. The effects of childhood sexual abuse often persist into adulthood (Clermont County CPS, 2021; RAINN, 2024).
Indicators of Sexual Abuse
Physical evidence of sexual abuse may not be present or may be overlooked. Victims of child sexual abuse are seldom injured due to the nature of the acts. Most perpetrators of child sexual abuse go to great lengths to “groom” the children by rewarding them with gifts and attention and try to avoid causing them pain in order to ensure that the relationship will continue.
If physical indicators occur, they may include:
- Symptoms of sexually transmitted diseases, including oral infections, especially in preteens
- Difficulty in walking or sitting
- Torn, stained, or bloody underwear
- Pain, itching, bruising, or bleeding in the genital or anal area
- Bruises to the hard or soft palate
- Pregnancy, especially in early adolescence
- Painful discharge of urine or repeated urinary infections
- Foreign bodies in the vagina or rectum
- Painful bowel movements
(Clermont County CPS, 2021; RAINN, 2024; NYS OCFS, n.d.-b)
Children’s behavioral indicators of child sexual abuse include:
- Unwillingness to change clothes for or participate in physical education activities
- Withdrawal, fantasy, or regressive behavior, such as returning to bedwetting or thumb-sucking
- Inappropriate, bizarre, suggestive, or promiscuous sexual behavior
- Inappropriate sexual knowledge for age
- Verbal disclosure of sexual assault
- Involvement in commercial sexual exploitation
- Forcing sexual acts on other children
- Extreme fear of closeness or physical examination
- Suicide attempts or other self-injurious behaviors
- Layered or inappropriate clothing
- Hiding clothing
- Lack of interest or involvement in activities
(Clermont County CPS, 2021; RAINN, 2024; NYS OCFS, n.d.-b)
RECOGNIZING TRAFFICKING
The media often portrays trafficking victims as women who are in chains or have a sign written on their hands that says, “Help Me.” However, this is not what most trafficking victims look like. When victims of human trafficking present in healthcare settings, it is uncommon for them to self-disclose that they are victims. They have significant trust issues, and even when asked directly, they are not likely to disclose that they are victims. The exploiter may also accompany victims, and as with victims of domestic violence, that presence will discourage victims from making any disclosures to a clinician.
It is important for healthcare providers to ask about exploitation because up to 88% of adolescent victims of trafficking reported an encounter with a healthcare provider during the time that they were being exploited (Polaris, 2024).
Physical Signs
- Signs or a history of deprivation of food, water, sleep, or medical care
- Physical injuries typical of abuse, such as bruises, burns, cuts, scars, prolonged lack of health or dental care, or other signs of physical abuse
- Brands, scars, clothing, jewelry, or tattoos indicating someone else’s “ownership”
- Presence of sexually transmitted infections
- Pregnancy
- Possession of cell phones, jewelry, large amounts of cash, or other expensive items that appear inconsistent with the patient’s stated situation
- Substance abuse or dependence signs and symptoms
- Clothing that is inappropriate for the weather or emblematic of commercial sex
(Polaris, 2024)
Psychological/Emotional Signs
- Fear, anxiety, depression, nervousness, hostility, flashbacks, or avoidance of eye contact
- Restricted or controlled communication or use of a third party to translate with no indicator of inability to understand English
- Inconsistencies in the history of the illness or injury
- Denial of victimization
- Attempted suicide, submissiveness, fearfulness, self-harm, or other signs of psychological abuse
- Appearing to be controlled by a third party (e.g., looking for permission to speak, not being left alone)
- Isolation from family or former friends
- Fear of employer
- Described or implied threats to self or family/friends
- History of running away
(Polaris, 2024)
Environmental/Situational Signs
- Working and living in the same place
- Lacking the freedom to leave their working or living conditions
- Being escorted or kept under surveillance when they are taken somewhere
- Not being in control of their own money
- Having no, or few, personal possessions
- Frequently lacking identifying documents, such as a driver’s license or passport
- Indicators of being a minor in a relationship with a significantly older adult
- Not knowing their own address
- Being in possession of hotel keys
(Polaris, 2024)
Signs in the Healthcare Setting
- Delaying seeking care for an illness
- Malnourishment
- Physical injuries consistent with long-term abuse, such as bruises in various stages of healing or signs of physical or sexual abuse
- Substance use
- Poor hygiene
- Health conditions of vulnerability such as disabilities and mental health issues
- Giving scripted answers/stories
- Minimizing abuse or injuries
- Being anxious
- Not being aware of location, date, or time of day
- Hesitating when answering questions about an injury or illness
- Symptoms related to depression or PTSD
- Presence of a third party who monitors the child’s responses, answers for them, behaves in an aggressive or verbally abusive manner, insists on filling out paperwork, or demands to remain in the room with the child
- Leaving against medical advice or seeming pressured to leave quickly
- Reporting not having a fixed address
(Polaris, 2024)
SCREENING FOR COMMERCIAL SEXUAL EXPLOITATION OF CHILDREN (CSEC)
There are several downloadable validated screening tools for CSEC and a variety of known risk factors for victimization that have been identified through research. Greenbaum and colleagues (2018) developed a short, six-question screening tool for CSEC that can be used effectively for youth in the healthcare setting by a clinician. This short questionnaire also differentiates between victims of sex trafficking and youth who may have experienced sexual assault or abuse without sex trafficking. Each positive response is given a 1-point score. A cut-off score of 2 indicates a patient suspected for CSEC and indicates further questioning by someone trained in a trauma-informed approach (Ellis et al., 2022).
- Is there a previous history of drug and/or alcohol use?
- Has the youth ever run away from home?
- Has the youth ever been involved with law enforcement?
- Has the youth ever broken a bone, had a traumatic loss of consciousness, or sustained a significant wound?
- Has the youth ever had a sexually transmitted infection?
- Does the youth have a history of sexual activity with more than five partners?
INDICATORS IN A VIRTUAL ENVIRONMENT
Mandated reporters must be aware of indicators of abuse or maltreatment that can be assessed for in a virtual environment for such children who attend school remotely, visit doctors using telemedicine, or participate in therapy sessions on virtual platforms.
Recommendations for assessing for potential abuse or maltreatment when interacting in a virtual environment include:
- Use reliable technology with adequate lighting and sound.
- Confirm the child’s physical location in the event you need to contact emergency services.
- Provide clear channels to reach out, such as email, phone, chat, text, or online tools.
- Make sure the child is present for at least part of the virtual interaction.
- Be alert if a child turns off a webcam or is very hesitant to use one.
- Ask everyone to introduce themselves who is in the room with the child or who enters the room after the visit starts.
- Be alert for indications that a child is trying to communicate something without someone else in the room noticing.
- Pay attention to nonverbal cues (e.g., if a child’s demeanor or behavior is different when someone else enters the room).
- Listen for concerning statements a child makes, including to siblings or peers.
- Be alert for altercations between children or adults. (Even if altercations do not rise to a level of suspected abuse, they may create an opportunity for a conversation about safety or managing stress.)
- Observe the child’s body for possible physical indicators, even if only the face, neck, shoulders, or chest may be visible.
- Note behavior in the child that indicates depression or anxiety.
- Ask if there is enough privacy for the child or parent to discuss sensitive matters. This may mean asking nonparticipating household members to move to a different room.
- Assess the environment (e.g., Are there noticeable unsafe conditions? Is there appropriate supervision for the child? Are young children watching even younger siblings?)
- Watch carefully, verbalize one’s observations, and ask if the family agrees.
(NYS OCFS, 2022)
CASE
A mother brought her 12-year-old daughter, Chantal, to the emergency department. She said that her daughter had been complaining about painful urination and wanted to check if she might have a bladder infection. The triage nurse, Janelle, asked the mother, who appeared to be in the last trimester of pregnancy, to fill out some paperwork while she took the girl to the bathroom for a urine specimen.
Janelle noticed that the daughter appeared fearful and sat in silence while her mother did all of the talking. When they were alone behind closed doors, Janelle asked Chantal if there was anything that she wanted to talk about privately. Chantal responded by shaking her head no, but Janelle sensed that the girl was holding something back.
Chantal was able to produce a clear, pale yellow urine specimen and then followed the nurse to an exam room. Janelle asked her if she had any pain when she urinated, and Chantal said yes. The nurse asked her if she had begun menstruating, and the child said she had not.
Janelle brought the mother into the exam room to wait with her daughter. After obtaining a brief history from the mother, the physician ordered a urinalysis. The urinalysis was negative. The doctor did an external genital exam that revealed numerous vesicular lesions on her labia. The child denied any sexual activity. The doctor cultured the lesions for herpes and asked the mother to step into his office to discuss his findings.
Once Janelle and Chantal were alone again in the room, the child burst into tears and told the nurse that her mother’s boyfriend had been rubbing his “private” on her and said that if she told anyone, her mother would go to jail. The nurse stopped questioning the child and reported her suspicion of child sexual abuse according to state laws and procedures. The nurse knew that victims of child sexual abuse should only be minimally questioned until they could undergo a forensic interview.
On the following day, Chantal was interviewed by a child forensic interview specialist in a child-friendly advocacy center. She and her mother, who was also a victim of child sexual abuse, received counseling for over a year. Following the investigation, the mother’s boyfriend was eventually tried and convicted of sexual abuse.
RECOGNIZING AND RESPONDING TO VICTIMS’ DISCLOSURES
It is difficult for young children to describe abuse. They may only disclose part of what happened, or they may make an indirect disclosure such as, “My stepdad keeps me up at night.” It is important not to rush the child and to listen to their concerns so that the child feels safe and supported. If a child discloses abuse, the following actions by the healthcare professional will help the child:
- Avoid denying what the child discloses.
- Provide safety and reassurance.
- Listen without making assumptions.
- Do not interrogate.
- Limit questioning to only four queries:
- What happened?
- When did it happen?
- Where did it happen?
- Who did it? (How do you know them?)
- Do not make promises.
- Document the child’s statements using exact quotes.
- Remain nonjudgmental and supportive.
- Understand the dynamics of abuse and neglect.
- Report suspicions to the authorities.
(Childhelp, 2021)
Interviewing for Sexual Assault
If a child or adolescent discloses sexual abuse to a trusted adult or there is cause for the adult to suspect sexual abuse, the adult should not question the child further. They should instead contact Child Protective Services or, if the child is in imminent danger, the police. These professionals have protocols in place to interview the child by a child interview specialist while police, prosecutors, and caseworkers observe.
Such forensic interviewers are trained to communicate in an age- and developmentally appropriate manner. Coordination of services with a child forensic interviewer is essential to minimize trauma and to ensure the use of evidence-based practices to listen more effectively to the child. Forensic interviewers rely on critical thinking, ethical standards, and professional judgment. They must participate in ongoing training and peer review. The American Professional Society on the Abuse of Children published updated practice guidelines for forensic interviewing in 2023 (APSAC Taskforce, 2023).
Management
A physically abused child is screened for emergent needs. Once stability has been established, the child undergoes a history and physical. ChildLine should be informed when there is a suspicion of abuse and the child may need to be seen in an in-patient facility so that lab work and imaging can be done.
A child who has been sexually abused is also evaluated for physical, mental, and psychosocial needs. Baseline testing is performed for sexually transmitted infections (STIs) for children of all ages. Pregnancy testing and empiric treatment for STIs may also be given to adolescent victims. STI prophylaxis and emergency contraception may be offered if the patient presents within 120 hours. Medication may include a regimen of non-occupational post-exposure prophylaxis (nPEP) if the patient presents within 72 hours. Evaluation at the earliest opportunity can be helpful to examine for anogenital injury and collect forensic evidence (CDC, 2021).
Photographing Evidence
Whenever there are allegations of suspected child abuse or neglect, any records of physical findings may be used as evidence at a trial. Therefore, photos, diagrams, and accurate reporting of medical examination findings are invaluable. Such documentation should use language that is not open to misinterpretation.
If photographs will be needed, it is a good idea to inform the child or adolescent and encourage them to participate in the process. Photographs are another form of medical documentation that can provide objective, visual documentation of abuse. There should be a protocol for releasing the photos after a formal request, and a chain of custody may be necessary as well.
REDUCING BIAS IN REPORTING
A mandated reporter’s decision to report child abuse can change the course of the life of a child and family members and have long-lasting and devastating impacts on both families and communities. Therefore, it is important for professionals to be aware of the potential for implicit biases and to ensure that such biases do not impact their decision-making. Instead, decisions must be made based on the objective facts of a situation.
A proven strategy to reduce bias and increase awareness regarding one’s own beliefs is to ask oneself the question, would I make a different decision about reporting if the child or family in a situation of suspected child maltreatment or abuse were of a different:
- Race?
- Ethnicity?
- Gender?
- Gender identity?
- Sexual orientation or expression?
- Religion?
- Immigration status?
- Primary spoken language?
- Culture?
- Age?
- Neighborhood where they reside?
- Presence of a disability?
- Occupation?
- Socio-economic status of the family?
If the answer is yes, bias may be impacting one’s decision to make a report.
Another strategy when assessing information received about a child and their family is to ask analytical and evaluative questions and use critical thinking. This includes:
- Identifying the specific concerns about the current situation
- Gathering adequate information about the current situation
- Analyzing that information to separate facts from assumptions
- Recognizing the possibility of bias in one’s personal opinions
- Developing multiple hypotheses that could explain the situation
- Determining whether making a report is legally required
- If not, determining whether an alternative option is better, such as connecting the individual or family to appropriate services in their community
(NYS OCFS, 2022)
REPORTING CHILD ABUSE AND NEGLECT
The government has a responsibility to protect children when parents fail to provide proper care and to intervene in cases of child maltreatment. The federal Child Abuse Prevention and Treatment Act (CAPTA) requires each state to have a system in place that requires certain individuals to report suspected child abuse and neglect. All states list the mandated reporters, responsibilities of institutions, standards for making reports, and how confidentiality of the reporting party is maintained.
Who Must Report Abuse?
Anyone may report suspected child abuse at any time and is encouraged to do so. Such reports are typically confidential and may be made anonymously by members of the public.
Nearly all states designate certain professions whose members are mandated by law to report child maltreatment. Typically, these individuals have frequent contact with children. Such persons may include:
- Social workers
- Teachers and other school personnel
- Physicians, nurses, and other healthcare workers
- Mental health professionals
- Child care providers
- Medical examiners or coroners
- Law enforcement officers
Some other professions include film or photograph processors, computer technicians, substance abuse counselors, probation or parole officers, and attorneys and clergy in certain circumstances. Domestic violence workers, animal control or humane officers, and court-appointed special advocates are also required to report in some states.
In more than one third of states, any person who suspects child abuse or neglect is required to report it. In most of those states, professionals who are mandated to report are also listed, but all persons who are aware of abuse are required to report.
It is important that all professionals be informed of the laws that pertain to the jurisdiction(s) of their own practice (CWIG, 2023).
What Situations Require That a Report Be Made?
State statutes vary, but generally a mandatory reporter must make a report when they suspect or have reason to believe that a child is abused or neglected. The reporter does not have to provide proof of the suspected abuse or neglect (CWIG, 2023).
(For state-by-state information on mandated reporting, see “Child Welfare Information Gateway” in the “Resources” section at the end of this course.)
REASONABLE CAUSE
There can be “reasonable cause” to suspect that a child is abused or maltreated if, considering the physical evidence observed or information that had been disclosed and based on the reporter’s own training and experience, it is possible that the injury or condition was caused by neglect or by nonaccidental means.
Certainty is not required. The reporter need not be certain that the injury or condition was caused by neglect or by nonaccidental means. The reporter need only be able to entertain the possibility that it could have been neglect or nonaccidental in order to possess the necessary “reasonable cause.” It is enough for the mandated reporter to distrust or doubt what is personally observed or information that had been disclosed to the reporter about the injury or condition.
In child abuse cases, many factors can and should be considered in the formation of that doubt or distrust. Physical and behavioral indicators may also help form a reasonable basis of suspicion. Although these indicators are not diagnostic criteria of child abuse, neglect, or maltreatment, they illustrate important patterns that may be recorded in the written report when relevant.
How Is a Report Made?
In most jurisdictions, a telephone report should be made immediately and then followed by a written report. States often provide standardized forms for this purpose, and many jurisdictions offer electronic reporting.
Most healthcare facilities also have policies and procedures in place regarding the reporting of suspected child abuse. Healthcare professionals and other mandatory reporters must know what guidelines are in place at their place of employment as well as state mandates.
At the time of an oral telephone report, frequently to a state-subsidized 800 number, a Child Protective Services (CPS) specialist will typically request the following information:
- The condition of the child
- Names and addresses of the child and parents or other person responsible for care
- Location of the child at the time of the report
- Child’s age, gender, and race
- Nature and extent of the child’s injuries, abuse, or maltreatment, including any evidence of prior injuries, abuse, or maltreatment to the child or their siblings
- Name of the person or persons suspected to be responsible for causing the injury, abuse, or maltreatment (“subject of the report”)
- Family composition
- Any special needs or medications
- Whether an interpreter is needed
- Source of the report
- Person making the report and where reachable
- Actions taken by the reporting source, including taking of photographs or X-rays, removal or keeping of the child, or notifying the medical examiner or coroner
- Any additional information that may be helpful
A reporter is not required to know all of the above information in making a report; therefore, lack of complete information does not prohibit a person from reporting. However, information necessary to locate a child is crucial.
(See also “Childhelp National Child Abuse Hotline” in the “Resources” section at the end of this course.)
CASE
Esmerelda, a school teacher, stops by her friend Janie’s house for coffee. While she is there, Janie’s son, Caden, who is a student in Esmerelda’s class, runs into the kitchen and for no apparent reason aggressively shoves his 2-year-old sister, who falls to the floor. Caden, age 7, has been diagnosed with a spectrum disorder. While the toddler is not injured, Janie yells at Caden, picks him up, and throws him across the kitchen, where he slides into a cabinet, hitting the back of his head.
Concerned for his well-being, Esmerelda examines Caden and finds that he is okay. Even so, Esmerelda recognizes the importance of taking action for the safety of her student. She empathizes with Janie and expresses her concern for the family. She acknowledges how frightening and stressful it must be for Janie to have a child with a serious condition. She then shifts to a professional role, asking Janie if she can refer Caden to a program for children with learning differences that is provided by the school district. Janie tearfully agrees, and Esmerelda makes a call to the school district to gather information about the program.
Esmerelda is aware that she is a mandated reporter of child abuse in her state because she is a teacher who has responsibility for her students. She also has reasonable cause to suspect that Caden may be a victim of child abuse due to the severity of the incident that she observed. Esmerelda lets Janie know that she must make an immediate report of suspected child abuse. When calling in her report by phone, Esmerelda describes the incident, including Janie’s desire to help her child and her voluntary interest in a referral to services that can help her.
Esmerelda makes a point to call Janie the next day and frequently thereafter. Two months later, Janie tells Esmerelda that a social worker helped her find a program in which she is learning appropriate new ways of dealing with the challenge of Caden’s learning differences.
Mandatory Notification of Substance Exposed Infants
The CAPTA Reauthorization Act of 2003 contained legislation that called for mandated reporters to notify Child Protective Services when infants were identified as affected by substance abuse or withdrawal symptoms resulting from in-utero exposure to substances. The CAPTA Reauthorization Act of 2010 included additional legislation requiring that mandated reporters notify CPS for infants affected by fetal alcohol spectrum disorder (FASD). In 2016, further changes to CAPTA were made in response to the nation’s opioid epidemic, for instance, no longer specifying “illegal” in regard to substance abuse.
CAPTA also requires a plan of safe care, immediate screening, risk and safety assessment, and timely investigation for substance- and alcohol-affected infants. Safe care plans must address the affected caregiver as well as the infant. CAPTA also requires that states report data on affected infants and create and provide oversight systems to assure that safe care plans are implemented (U.S. DHHS, 2024).
HEALTHCARE PROVIDERS REQUIRED TO REPORT
The healthcare providers required to submit this notification vary by state but generally include licensed hospitals or healthcare facilities or persons who are licensed, certified, or otherwise regulated to provide healthcare services. These professions typically include physician, podiatrist, optometrist, psychologist, physical therapist, certified nurse practitioner, registered nurse, nurse midwife, physician’s assistant, chiropractor, dentist, pharmacist, and those accredited or certified to provide behavioral health services.
PLAN OF SAFE CARE
After notification of a child born affected by substance use or withdrawal symptoms resulting from prenatal drug exposure or a fetal alcohol spectrum disorder, a multidisciplinary team meets prior to the child’s discharge from the healthcare facility. The meeting informs an assessment of the needs of the child and the child’s parent(s) and immediate caregiver(s) to determine the most appropriate lead agency for developing, implementing, and monitoring a plan of safe care. Depending on the needs of the child and parents/caregivers, ongoing involvement of a county agency may not be required.
The child’s parents and immediate caregivers must also be engaged to identify the need for access to treatment for any substance use disorder or other physical or behavioral health condition that may impact the safety, early childhood development, and well-being of the child.
For the purpose of informing the plan of safe care, the multidisciplinary team may include public health agencies, maternal and child health agencies, home visitation programs, substance use disorder prevention and treatment providers, mental health providers, public and private children and youth agencies, early intervention and developmental services, courts, local education agencies, managed care organizations, private insurers, hospitals, and medical providers.
The intent of legislation that addresses substance-exposed newborns in recent years was to improve the care for these infants and families by involving CPS when the mother has a substance abuse disorder. A study by the Johns Hopkins University shows that reporting drug-exposed babies to CPS is often perceived as punitive and can be a deterrent to parents seeking treatment, prenatal care, or psychotherapy. It is important that providers are aware that in some states, substance use alone or a positive toxicology screen in a newborn is insufficient to generate a report to CPS, and there must be other identified concerns. Policymakers should try to improve guidance given to providers and find ways to help women with substance use disorder receive treatment early in pregnancy (McCourt et al., 2022).
Consequences for Failing to Report
Nearly every state imposes a penalty of a fine or incarceration for mandated reporters who willfully do not report suspected child abuse or neglect. Such mandated reporters may be charged with a misdemeanor or felony for the failure to report. In several states, mandated reporters can also be held liable by civil statutes for damages that result from their failure to report (CWIG, 2019).
Perhaps more importantly, failure to report can also lead to more serious consequences for the child and family. CPS cannot act until child abuse is identified and reported—that is, services cannot be offered to the family nor can the child be protected from further suffering.
Legal Protections for Reporters
CAPTA requires states to provide immunity from liability for individuals making good-faith reports of child abuse or neglect. States must comply with this mandate in order to be eligible for federal grants. In addition, the identity of the reporter is protected from disclosure to the alleged perpetrator (CWIG, 2023).
Mandatory reporting laws may recognize the right to maintain confidential communications between professionals and their clients, patients, or congregants. In order to provide protection to maltreated children, the reporting laws in most states and territories restrict this privilege for mandated reporters.
Among the requirements for receiving federal funding under CAPTA is that states must also preserve the confidentiality of all child abuse and neglect reports and records. This mandate protects the privacy of the child and their parents or guardians, except in certain limited circumstances. All jurisdictions have provisions that protect abuse and neglect records from public view, and many jurisdictions include specific provisions for this purpose (CWIG, 2022).
REPORTING IMPLICATIONS OF HIPAA
Mandated reporters often express reluctance to report child abuse because they are concerned they may compromise patient privacy under the Health Insurance Portability and Accountability Act (HIPAA) of 1996. HIPAA provisions do not, in fact, inhibit the responsibilities of mandated reporters of child abuse and neglect. HIPAA 164.512, b (1) states that “a covered entity may use or disclose protected health information for the public health activities and purposes described in this paragraph to a public health authority or other appropriate government authority authorized by law to receive reports of child abuse or neglect.” This means that mandated reporters may report suspected child abuse and neglect to a local agency that is authorized to receive the information. The agency may be a social services department or a police department, for example (U.S. DHHS, 2020).
CONCLUSION
Child abuse and neglect negatively impact the health and well-being of society. Child victimization is not only a social problem but also a serious public health issue. Child abuse and neglect affect not only the victims while they are children but also shape the adults these children will become. Prevention of child abuse and neglect is a fundamental goal to create healthy children who will in turn become healthy adults.
Research on child abuse and neglect indicates that its incidence can be reduced and its harmful effects can be diminished through prevention and treatment. Individuals, communities, and society must provide safe environments for all children.
Mandated reporters are obligated to report suspected child abuse and neglect. Reporting suspected child abuse is their duty as professionals, but it is also an opportunity to help improve the health and well-being of children and take part in creating a healthier society.
RESOURCES
Abandoned Infant Protection Act Information Hotline
866-505-SAFE (7233)
American Professional Society on the Abuse of Children
Childhelp National Child Abuse Hotline
800-422-4453 (call or text)
Child Welfare Information Gateway
Council on Child Abuse and Neglect (American Academy of Pediatrics)
National Center for Missing and Exploited Children
National Runaway Safeline
800-RUNAWAY (786-2929)
State statutes database (CWIG)
REFERENCES
NOTE: Complete URLs for references retrieved from online sources are provided in the PDF of this course.
APSAC Taskforce. (2023). Forensic interviewing of children. https://apsac.org
CAPTA, 42 U.S.C.A. § 5106g(4). (2010). Child Abuse Prevention and Treatment Act. https://www.acf.hhs.gov
Centers for Disease Control and Prevention (CDC). (2024a). Child abuse and neglect prevention: About child abuse and neglect. https://www.cdc.gov
Centers for Disease Control and Prevention (CDC). (2024b). About child abuse and neglect. https://www.cdc.gov
Centers for Disease Control and Prevention (CDC). (2024c). Child abuse and neglect prevention: Risk and protective factors. https://www.cdc.gov
Centers for Disease Control and Prevention (CDC). (2024d). About abusive head trauma. https://www.cdc.gov
Centers for Disease Control and Prevention (CDC). (2021). Sexually transmitted infections treatment guidelines, 2021: Sexual assault or abuse of children. https://www.cdc.gov
Childhelp. (2021). What is child abuse? https://childhelphotline.org
Child Welfare Information Gateway (CWIG). (2023). Mandatory reporting of child abuse and neglect. U.S. Department of Health and Human Services, Administration for Children and Families, Children’s Bureau. https://www. childwelfare.gov
Child Welfare Information Gateway (CWIG). (2022). Definitions of child abuse and neglect. U.S. Department of Health and Human Services, Administration for Children and Families, Children's Bureau. https://www.childwelfare.gov
Child Welfare Information Gateway (CWIG). (2021). Infant safe haven laws. https://www.childwelfare.gov
Child Welfare Information Gateway (CWIG). (2019). Penalties for failure to report and false reporting of child abuse and neglect. U.S. Department of Health and Human Services, Children’s Bureau. https://www.childwelfare.gov
Clermont County Children’s Protective Services (CPS). (2021). Detecting child abuse and neglect. https://cps.clermontcountyohio.gov
Ellis A, Brown A, Martini A, Page E, Lin L, & Vaughn M. (2022). Application of a child sex trafficking screening tool in patients with abuse: A retrospective chart review in the pediatric emergency department. Journal of Pediatric Health Care, 36(4), 330–38. https://www.sciencedirect.com
Feldman M, Sheridan M, & Xiong G. (2020). Factitious disorder imposed on another. Medscape. https://emedicine.medscape.com
Greenbaum VJ, Dodd M, & McCracken C. (2018). A short screening tool to identify victims of child sex trafficking in the health care setting. Pediatric Emergency Care, 34, 33–7.
Horner G. (2021). Medical child abuse: Essentials for pediatric health care providers. Journal of Pediatric Health Care, 35(6), 644–50. https://doi.org/10.1016/j.pedhc.2021.01.006.
Kids Matter. (2022). Emotional abuse. https://kidsmatterinc.org
Mayo Clinic. (2024). Child abuse. https://www.mayoclinic.org
McCourt AD, White SA, Bandara S, Schall T, Goodman DJ, Patel E, & McGinty EE. (2022). Development and implementation of state and federal child welfare laws related to drug use in pregnancy. Milbank Q, 100(4), 1076–1120. https://doi.org/10.1111/1468-0009.12591
Narang SK, Fingarson A, Lukefahr J, & Council on Child Abuse and Neglect. (2020). Abusive head trauma in infants and children. Pediatrics, 145(4), Article e20200203. https://pediatrics.aappublications.org
National Center for Missing and Exploited Children (NCMEC). (2024). Child sex trafficking. https://www.missingkids.org
National Center on Safe Supportive Learning Environments (NCSSLE). (2021). Human trafficking in America’s schools: Child labor trafficking. https://safesupportivelearning.ed.gov
National Children’s Alliance. (2024). National statistics on child abuse. https://www.nationalchildrensalliance.org
National Human Trafficking Training and Technical Assistance Center (NHTTTAC). (n.d.). SOAR: Stop: Describe the types of trafficking and common risk factors. https://nhttac.acf.hhs.gov
New York State Office of Children and Family Services (NYS OCFS). (2022). 2022 NYS mandated reporter training syllabus.
New York State Office of Children and Family Services (NYS OCFS). (n.d.-a). Adverse childhood experiences (ACEs). https://ocfs.ny.gov
New York State Office of Children and Family Services (NYS OCFS). (n.d.-b). Signs of child abuse or maltreatment. https://ocfs.ny.gov
New York State Office of Children and Family Services (NYS OCFS). (n.d.-c). Child protective services. https://ocfs.ny.gov
Pierce MC, Kaczor K, Lorenz DJ, et al. (2021). Validation of a clinical decision rule to predict abuse in young children based on bruising characteristics. JAMA Network Open, 4(4), Article e215832. https://doi.org/10.1001/jamanetworkopen.2021.5832
Polaris. (2024). Human trafficking and the healthcare industry. https://polarisproject.org
Rape, Abuse & Incest National Network (RAINN). (2024). Child sexual abuse. https://www.rainn.org
Research Foundation of SUNY/Center for Development of Human Services. (2011). Mandated reporter training: Identifying and reporting child abuse and maltreatment/neglect. http://www.ocfs.state.ny.us/ohrd/materials/58451.pdf
South Dakota Department of Social Services (SD DSS). (2020). Signs of child abuse and neglect. https://dss.sd.gov
Thatcher T. (2020). Families in crisis: How parental substance abuse and mental health impacts kids. https://valleycares.com
U.S. Department of Health and Human Services (U.S. DHHS). (2024). Child maltreatment 2022. Administration on Children, Youth and Families, Children’s Bureau. https://www.acf.hhs.gov
U.S. Department of Health and Human Services (U.S. DHHS). (2020). Health information privacy: Public health. https://www.hhs.gov






Customer Rating
4.9 / 286 ratings